Abstract
Transforming growth factor-beta1 (TGF-β1) is a potent peptide that inhibits epithelial and mesenchymal cell proliferation and stimulates the synthesis of extracellular matrix components. This cytokine is produced in a biologically latent complex bound to a latent-associated peptide (LAP), and it is the disassociation of this complex that regulates TGF-β activity. A number of mechanisms have been shown to activate TGF-β1. We show here that reactive oxygen species (ROS), generated by the iron in chrysotile or crocidolite asbestos, mediate the biological activity of TGF-β1. Recombinant human latent TGF-β1 was activated in a cell free system in the presence of asbestos and ascorbic acid. Latent TGF-β1 was overexpressed in both A549 and mink lung epithelial cell lines through an adenovirus vector containing the full-length construct for porcine TGF-β1. This latent TGF-β1 was activated in a concentration-dependant fashion by introducing asbestos into the cell cultures. This activation was reduced significantly through the use of superoxide dismutase, catalase or deferoxamine. Amino-acid constituents of the LAP were oxidized as demonstrated by the appearance of carbonyls detected by Western analysis. The oxidized LAP could no longer form a complex with TGF-β1. Our data support the postulate that ROS derived from asbestos provide a mechanism for activating TGF-β1 in the alveolar environment by oxidizing amino acids in LAP.
Similar content being viewed by others
Main
Asbestos fibers are known to cause lung scarring (asbestosis) in man and animals and are cytotoxic in vitro and in vivo.1 Part of this toxic effect of asbestos has been attributed to reactive oxygen species (ROS). These ROS are formed indirectly through macrophage and inflammatory cell stimulation and directly on the alveolar surfaces through Fenton reactions catalyzed by the iron content of the asbestos.1 ROS have been demonstrated to contribute to asbestos-induced alveolar cell injury and carcinogenesis through generation of DNA strand breaks,2 lipid peroxidation3 and apoptosis.1 These cytotoxic and fibrogenic effects can be decreased through the use of antioxidants4 and through the treatment of asbestos with iron-chelating agents.5
Some investigators assume that chrysotile asbestos does not contain bioavailable iron, but this is not the case. While the basic chemical structure of chrysotile does not include iron,6 the fibers can accumulate Fe2+ and Fe3+ (from 3 to 7%6) as a commonly found component of the ore that is mined.6 In addition, several laboratories have demonstrated that chrysotile fibers accumulate bioactive iron in vitro and in vivo,1 and these ions participate in the toxic, fibrogenic and carcinogenic properties of chrysotile asbestos (for review see Kamp and Weitzman1). In as much as chrysotile is the most commonly used form of asbestos worldwide,6 we typically use this variety of fiber for both in vitro and in vivo studies.7 We have primarily used chrysotile in the studies reported here and have compared these findings with crocidolite asbestos, a fiber with iron as a component of its chemical formula.6
A number of cytokines are thought to be significant contributors in the development of human interstitial fibrosis and in models of pulmonary fibrogenesis. For example, it has been demonstrated that inhalation of asbestos enhances tumor necrosis factor-α (TNF-α),7 transforming growth factor-α (TGF-α),8 platelet-derived growth factor (PDGF) isoforms,9 transforming growth factor beta (TGF-β),10, 11 as well as fibronectin expression at sites of fiber deposition,10 correlating with elevated levels of cellular proliferation,9 and extracellular matrix (ECM) deposition in both rats10, 12 and mice.11 Of these factors, TGF-β1 is the most potent in upregulating genes involved in collagen and fibronectin biosynthesis.13 TGF-β1 also is a chemoattractant for monocytes and neutrophils.13 In addition, TGF-β1 is an inhibitor of inflammation and epithelial cell proliferation and can either stimulate or reduce mitogenesis in fibroblasts.14 It has been shown that transduction of biologically active TGF-β1 into the lungs of rats through an adenovirus vector produces an inflammatory and fibrogenic response.15 We have shown, using this same vector, that when active TGF-β1 is transduced into the lungs of fibrogenic-resistant TNF-α receptor knockout mice, the TGF-β1 alone is sufficient to induce fibroproliferative lung disease.16
TGF-β1 is produced in a latent complex, which consists of TGF-β1 noncovalently bound to a latent-associated peptide (LAP).17 It is the removal of the LAP, which allows TGF-β1 to be biologically active. This activation step is a major controlling point in the regulation of TGF-β1 biological activity, but the mechanisms controlling TGF-β1 activation are only partially understood. Several activation mechanisms have been shown, including proteolytic and enzymatic processes,17 as well as integrin binding.18, 19 Some earlier work provided evidence that ROS could play a role in activating TGF-β. For example, Ehrhart et al20 demonstrated activation of TGF-β1 in irradiated murine mammary glands.20 They further supported these data by demonstrating the activation of recombinant TGF-β1 in vitro in the presence of ionizing radiation, as well as in the presence of iron catalyzed Fenton reactions, demonstrating a mechanism of direct ROS-induced activation of TGF-β1.21 In further support of this concept, Dai et al22 showed that iron containing dusts increase the amounts of TGF-β1 and procollagen,5 and they subsequently showed that this iron is significant in the generation of fibrosis.
Since asbestos fibers are an excellent source of ROS,1, 23 we are proposing in the work presented here that activation of TGF-β1 by ROS could control the biological activity of TGF-β1 in asbestos-induced fibrogenesis, and possibly in any situation where there is generation of ROS and lung injury. We postulate that asbestos-associated iron mediates the generation of ROS with consequent activation of latent TGF-β1 and demonstrate that asbestos-derived ROS activate recombinant latent TGF-β1 in a cell free system. Furthermore, mink lung epithelial cells (MLEC) and A549 cells transduced with an adenovirus vector containing the full-length construct for latent TGF-β1 release large amounts of inactive peptide. We show that exposure of this latent TGF-β1 to chrysotile asbestos causes an increase in the biologically active form of TGF-β1. Amino acids within the LAP apparently are oxidized, thus preventing the LAP from forming a complex with TGF-β1. The activation of TGF-β1 is abrogated by treatment of the cells with the antioxidants superoxide dismutase (SOD) and catalase or the iron chelator deferoxamine. If the same reactions take place in vivo, a mechanism could be in hand to explain the activation of TGF-β1 during the development of fibrogenesis where reactive oxygen species are present.
Materials and methods
Asbestos and Reagents
Chrysotile and crocidolite asbestos were provided by NIEHS (NIEHS, Research Triangle Park, NC, USA) and were used as defined previously.24 Recombinant human (rh) TGF-β1 and rh-LAP were purchased from R&D systems (R&D systems, Minneapolis, MN, USA). Fetal bovine serum, trypsin/EDTA, and penicillin/streptomycin were GIBCO products from Invitrogen (Invitrogen Corp. Carlsbad, CA, USA). All of the remaining reagents were purchased from Sigma chemicals (Sigma-Aldrich, St Louis, MO, USA).
Protein derivatization with 2,4-dinitrophenyl-hydrazine (DNPH)
Protein oxidation in the form of carbonyl carbons was detected using Oxyblot Protein Oxidation Detection Kit (Chemicon International, Temecula, CA, USA). Briefly, proteins were denatured with 6% SDS. Samples were then derivatized by adding DNPH (1:1) and incubated at room temperature for 15 min, followed by the addition of neutralization solution.
SDS-PAGE and Western analysis
Proteins were loaded on a NuPAGE 10% Bis-Tris gel (Invitrogen Life Technologies, Carlsbad, CA, USA) and run at 200 V for 1 h. Proteins were transferred onto Invitrolon PVDF (Invitrogen Life Technologies, Carlsbad, CA, USA). Powdered milk (5% in Tris-buffered saline, 0.1% Tween (TBST)) was used as blocking solution throughout. Membranes were blocked for 1 h, followed by incubation with either rabbit anti-DNPH (1:150, 1 h) (Chemicon International) or goat anti-human LAP (1:100 overnight, 4°C) (R&D Systems). After incubation, membranes were washed 3 × in TBST, and incubated with appropriate secondary antibody (goat anti-rabbit Ig or rabbit anti-goat Ig) conjugated to horseradish peroxidase. For 1 h followed 3 × washes in TBST and 3 × wash in TBS. Proteins were detected with chemiluminescence (Amersham).
Cell culture
A human epithelial cell line, A549, with characteristics of alveolar type II cells as well as MLE cells were used for this study. The cells were obtained from American Type Culture Collection (Rockville, MD, USA). Cells were cultivated in Dulbecco's modified Eagles medium (DMEM) with 2% penicillin/streptomycin and 10% fetal bovine serum, at 37°C, in an atmosphere of 5% CO2 and 95% humidity. For MLECs, DMEM was supplemented with tricine (6.73 g/l). For maintenance of stock cultures, cells were grown to near confluence and dislodged using 0.5% trypsin and 0.2% EDTA. Cells were then resuspended in growth media and plated.
Preparation of chrysotile and crocidolite
Weighed aliquots of chrysotile and crocidolite asbestos (10 mg) were autoclaved and diluted in sterile PBS to a final concentration of 1 mg/ml. The asbestos was sheared by passage through 18, 21, 25 and 27 gauge needles (10 × each), followed by sonication for 2 h prior to its administration to cell culture. It is well known that there are many more chrysotile fibers per unit mass than there are crocidolite fibers.25 Thus, in the studies reported here, we have not made direct dose–response comparisons of the two fiber types, but it is clear that both chrysotile and crocidolite contain bioactive iron that generates ROS.
For experiments requiring incubation of asbestos (1 mg/ml) with citrate (10 mM) or ascorbate (500 μg/ml), all samples were incubated in the dark under constant agitation in an environmental shaker. Subsequently, samples were centrifuged (5 min, 4000 rpm) to pellet the asbestos and the supernant used for further studies.
Adenovector preparation
Replication deficient, human adenovirus type-5 genome-based recombinant virus expressing the full length, latent porcine TGF-β1 was provided by Dr Jack Gauldie (McMaster University, Hamilton, ON, Canada).15 The methods for propagation and purification of recombinant adenovirus were previously described.15, 16 Briefly, the adenovector was grown up in 293 cells and the virus was purified by two rounds of CsCl-gradient centrifugation. The CsCl was removed by chromatography of the virus suspension in Econo-Pac 10DG desalting columns (Bio-Rad Laboratories, Hercules, CA, USA). Fractions of the virus in 10% glycerol were pooled in phosphate-buffered saline (PBS). Total virus particles were measured spectrophotometrically (260 nm) and infectious particles were assessed by measuring plaque forming units (PFU) in 911 cells. Plaques were counted on day 4 and 5.
Treatment of cells
Cells were seeded into 24-well tissue culture plates 50 000 cells/well and allowed to grow for 24 h to near confluence in DMEM with 10% FCS. After 24 h, the media was changed to serum free or 1% DMEM. After 24 h, the cultures were infected with TGF-β1 with an MOI of 10.26 After 24 h, sheared chrysotile was placed on the cells. Media were removed from the cells and the cells were trypsinized at the appropriate time points to measure TGF-β1 and cytotoxicity.
Cytotoxicity assay
Cytotoxicity was measured using a trypan blue-exclusion assay. Briefly, cells were trypsinized to remove the monolayer. Cells were passed several times through a pipette tip to break up any clumps. 10 μl Aliquots were removed and 2 μl of 0.4% trypan blue (Sigma Chemicals) was added to the cells. Cells were then pipetted onto a hemocytometer and counted. Dead cells were counted as trypan blue staining cells.
Measurement of TGF-β1
Elisa Active and total TGF-β1 were measured using a Duoset ELISA kit (R&D systems). Briefly, 96-well plates are coated overnight with capture antibody diluted in PBS. Afterwards, the wells are emptied, washed with PBS+Tween 20 (PBST), followed with the addition of blocking solution for 1 h. After a PBST wash, samples and standards are added to the plate and incubated for 2 h at room temperature. Wells were aspirated and washed with PBST, followed by the addition of detection antibody. After a 2-h incubation, wells were aspirated and washed with PBST. Streptavidin–HRP was added to each well and incubated for 20 min, followed by aspiration and PBST washing. Substrate solution was added for the color reaction, followed by the addition of stop solution. The optical density of each well was determined using a microplate reader set at 450 mn. Standards were run in duplicate and sample concentrations were determined by plotting their absorbance along the standard curve.
Mink lung cell assay The mink lung cell assay is a well-defined assay used to quantify the bioactivity of TGF-β1.27 Mink lung cells are highly sensitive to the growth inhibitory effects of TGF-β1. Briefly, cells were plated at 1.5 × 105 cells/well in a 24-well plate. Cells were allowed to go overnight for attachment and growth in 10% FCS–DMEM supplemented with tricine. The following day, DMEM–1% FCS with tricine was added to the cells, with the appropriate samples, and cells were again incubated overnight. To measure growth inhibition, cells were pulsed for 2 h with 3H-thymidine (1uci/well). Radioactive media were drained and cells were washed three times with cold PBS. Cells were scraped from plates in 1 ml PBS and spun. Pellets were resuspended in NaOH (0.3 N) on ice for 15 min, followed by the addition of 20% trichloroacetic acid. After 15 min, the cells were filtered through a GF/A glass fiber filter and rinsed with 90% cold ethanol. Filters were dried and placed in scintillation vials with luminol. 3H incorporation was measured on a scintillation counter as cpm.
PAI-luciferase Mink lung cells stably transfected with the TGF-β1 specific plasminogen activator inhibitor (PAI) promoter27 with a luciferase reporter were plated as described above and luciferase was assayed using the luciferase assay kit (Promega Corp, Madison, WI, USA). Briefly, media were aspirated and cells washed twice in cold PBS before being scraped in Cell Culture Lysis Reagent (CCLR). Cells were vortexed and freeze thawed, and 20 μl of lysate was assayed in 100 μl Luciferase Assay Reagent using a Luminometer (Lumat LB Variable Injector 9507) using a 2 s measurement delay, followed by a 10 s measurement read. Results were reported as relative light units (RLU).
Statistics
Each experiment was repeated at least three times and all data were analyzed in GraphPad InStat version 1.14 (San Diego, CA, USA). The ANOVA was used with Bonferroni correction to determine statistical significance (P≤0.01) between groups.
Results
Iron Catalyzed Activation of LTGF-β1 in a Cell Free System
Barcellos-Hoff and Dix demonstrated efficient activation of TGF-β1 through ROS induced by either gamma-radiation or iron catalysis.21 Iron in the presence of ascorbic acid produces the hydroxyl radical (OH·-), superoxide (O2·-) and hydrogen peroxide (H2O2). Lund and Aust28 demonstrated that iron is mobilized from both crocidolite and chrysotile asbestos through the use of different chelators.28 Therefore, we asked if asbestos-associated iron participates in the production of ROS and activation of TGF-β. We incubated the asbestos fibers (1 mg/ml) 24 h with citrate (10 mM), a weak iron chelator in normal saline, under constant agitation. The iron containing supernatant was then reacted with ascorbic acid (500 μg/ml) and recombinant latent TGF-β1 for 2 h. Active TGF-β1 was assessed using the mink lung cell PAI-luciferase assay as previously described. The results in Figure 1a show that iron disassociated from both forms of asbestos produce significant levels of TGF-β1 activation. Crocidolite activated more TGF-β1 than chrysotile in the presence of citrate+ascorbate (P<0.05), which is expected based on the increased iron content of crocidolite asbestos. Although saline may contain iron contamination, none of the control groups (citrate, ascorbate or citrate+ascorbate) showed any activation of TGF-β (data not shown).
In vitro activation of latent TGF-β1 by iron-mediated reactive oxygen species. (a) Chrysotile and crocidolite were incubated overnight in the presence of citrate (10 mM) or ascorbate (500 μg/ml) or both citrate and ascorbate. Iron mobilized from both forms of asbestos catalyzed activation of recombinant human latent TGF-β (rh-LTGF-β) in 2 h as determined by the PAI-luciferase assay, reported as relative light units (RLU) compared to asbestos alone. The combination of citrate and ascorbate activated more TGF-β in the presence of crocidolite compared to chrysotile. Values are means ±s.d. (n=3). *P<0.01 compared to untreated asbestos. #P<0.05 compared to chrysotile (b) rh-LTGF-β1 was incubated for 2 h in PBS containing chrysotile asbestos and either citrate (10 mM), ascorbate (500 μg/ml), or both citrate and ascorbate as described in (a). Supernatants were placed on MLEC cells to determine biological activity as measured by 3H-thymidine incorporation. Active TGF-β1 would decrease epithelial cell growth and 3H-thymidine incorporation. Asbestos plus citrate and ascorbate combined caused the largest effect in accordance with the luciferase assay shown in (a). Data are expressed as mean cpm (n=4) over nonasbestos-treated controls containing citrate, ascorbate and citrate or iron alone and are representative of three independent experiments.
To test the biological relevance of this activation by chrysotile, rh-LTGF-β1 was incubated for 2 h with chrysotile asbestos and citrate or ascorbate, or the combination of the two as described. After centrifugation, the supernant was removed from the asbestos, and TGF-β1 activation was measured by MLEC growth inhibition. Figure 1b shows that both citrate and ascorbate activated TGF-β1, and the combination of the two was the most efficient of the treatments. Results are reported as percent over control, with the controls being rh-LTGF-β1 incubated with the appropriate reagent with no asbestos. These results show that biologically active TGF-β1 can be produced within 2 h by asbestos-derived radicals.
ROS Oxidize Amino Acids of the LAP
Under normal circumstances, LAP associates with active TGF-β1 with high affinity to form the latent complex. To better understand how the latent complex might be altered by ROS, we investigated the components of the LAP-TGF-β1 complex in the presence of oxidative stress. Figure 2a demonstrates the induction of PAI-luciferase by active rh-TGF-b1 (1 ng/ml) in MLE cells. LAP (100 ng/ml) inhibits this activity three-fold when added to the media simultaneously with active TGF-β1. This inhibition is prevented when LAP has been incubated with FeCl3/ascorbate for 30 min prior to adding it to the media (Figure 2a). Conversely, 30 min incubation of TGF-β with FeCl3/ascorbate does not alter its luciferase activity, nor its ability to associate with LAP as shown in Figure 2b. Interestingly, oxidation of active rhTGF-β alone had nearly a two-fold increase in activity as opposed to nonoxidized. This apparently is due to contamination of the manufacturer's active TGF-β1 with latent TGF-β1 which is activated by the oxidative step (data not shown). PAI-luciferase activity has been shown to be very specific for TGF-β in this assay27 and in our hands, neither ascorbate, FeCl3 or the combination of the two induced PAI-luciferase activity above background (data not shown).
Effect of oxidation of either LAP or TGF-β on TGF-β activity. (a) Purified latency-associated peptide (LAP) associates with active TGF-β to form a latent complex, significantly neutralizing TGF-β induced luciferase activity (P<0.001) in the MLEC PAI-luciferase assay. Oxidation of LAP by FeCl3/ascorbate (LAPox) significantly reduces the LAP-TGF-β association. Values are mean±s.d. (n=4) and are representative of three separate experiments. *P<0.001 compared to simultaneous TGF-β1 and LAP treatment. (b) Oxidation of active TGF-β does not prevent the association of LAP with TGF-β1 (low luciferase activity) nor does oxidation of TGF-β protein interfere with its bioactivity. Values are mean±s.d. (n=4) and representative of three separate experiments. *P<0.001 compared to TGF-β1 treatment alone.
To understand the nature of the oxidative damage within the LAP, the oxidized peptide was derivatized with 2,4-dinitrophenylhydrazine (DNPH), which forms a stable product with protein carbonyls that are formed during oxidation of certain amino acids.29 With an antibody specific for DNPH, this oxidative damage can be demonstrated using Western blotting. Figure 3a shows that DNPH can be detected in oxidized, derivatized LAP (lane 1) but not in derivatized, nonoxidized (lane 2) and oxidized, nonderivatized (lane 3) LAP.
Oxidation of LAP causes the formation of protein carbonyl groups as demonstrated by Western blot. (a) To detect protein oxidation in the form of carbonyls, oxidized (FeCl3+ascorbate) and nonoxidized LAP were derivatized with 2,4-dinitrophenylhydrazine (DNPH) and subsequent DNPH/carbonyl complexes were detected by using an anti-DNPH antibody on Western blot. (b) Anti-LAP antibodies show that staining for LAP corresponds with DNPH staining in (a). Lane 1 (LAPox derivatized) shows heavy staining at 34 kDa as opposed to Lane 2 (LAPox nonderivatized) and lane 3 (LAP nonoxidized, derivatized).
Asbestos Induced Activation of Latent TGF-β1 in A549 Cells
To study asbestos-associated activation of latent TGF-β1 released by cells, we used the human A549 epithelial cell line as a model. Cells were maintained in 10% FCS–DMEM until treatment at a density of 5 × 105 cells/ml. At 24 h after seeding, the cells were put in 0.5% FCS–DMEM and transfected with an adenovirus expressing the full-length construct of porcine latent TGF-β1.15 Figure 4a shows that these cells expressed predominantly latent TGF-β1. At 24 h after transfection, chrysotile asbestos was added to the cells at concentrations of 5, 10 or 20 μg/cm2. Asbestos was left on the cultures until media were collected to assess activation of TGF-β1. In Figure 4b, concentration-dependent activation of TGF-β1 can be seen 3 days postchrysotile asbestos exposure.
Activation of latent porcine TGF-β1 by asbestos exposure in the human epithelial cell line A549. (a) Epithelial cells were transfected with adenovirus to express the full-length porcine TGF-β1 construct and produced predominantly latent TGF-β (hatched bar) and almost no (<0.025 ng/ml) active TGF-β (clear bar). (b) A549 cells transfected with ad-LTGF-β were exposed to chrysotile asbestos. Significant activation was measured 3 days postasbestos exposure in comparison to no treatment in a concentration-dependent manner (*P<0.001, #P<0.01). Active TGF-β1 was measured using ELISA and data are expressed as the mean (n=4)±s.d. Data shown are representative of three separate experiments.
Antioxidants Inhibit the Activation of Latent TGF-β1
To further investigate the role of ROS in TGF-β1 activation, the A549 cells producing latent TGF-β1 were incubated with the antioxidants catalase and SOD prior to asbestos exposure. When each antioxidant was used separately, there appeared to be little or no protective effect from asbestos-induced activation (data not shown). However, when both catalase and SOD were used in conjunction, there was significantly less activation of TGF-β1 (Figure 5) as measured by ELISA. TGF-β1 activation increased as the concentration of antioxidants decreased. These data further support the role of ROS as activators of TGF-β1.
Antioxidants (AO) prevent activation of TGF-β1. The antioxidants catalase and superoxide dismutase were added together to A549 cells treated with adeno-TGF-β1 prior to asbestos exposure. A dose-dependant prevention of activation can be seen here, with 400 U/ml giving the optimal protection by 3 days. Active TGF-β1 was measured by ELISA in the media at day 3 postexposure. Data are expressed as mean (n=4)±s.d. and are representative of three independent experiments. #P<0.01, *P<0.001 compared to asbestos with no antioxidant treatment.
It is well documented that ROS from chrysotile asbestos are cytotoxic in cell culture, and this cytotoxic effect is abrogated by antioxidants.30 To rule out the possibility of cell toxicity influencing TGF-β1 activation in our experiments, cells were exposed to cytotoxic agents for the same duration of time, and cell death was measured by trypan blue-exclusion staining and counting on a hemocytometer. Other cytotoxic agents such as LPS (37% viable cells) and cell lysis by H2O (0% viable cells) were more cytotoxic than asbestos at a concentration of 10 μg/cm2 (42% cell viability) at 3 days. However, this cytopathic effect did not activate TGF-β1 much above background (data not shown). This suggests that the activation seen in cell culture is due to ROS formed by the asbestos fibers rather than by release of ROS during cytotoxic events.
Deferoxamine Inhibits Chrysotile Asbestos Activation of TGF-β1 in Cell Culture
To determine if the TGF-β1 activation seen in cell culture is associated with the iron from the chrysotile, A549 cells transduced with adeno-LTGF-β1 were preincubated with deferoxamine (50 nM), and fresh deferoxamine was added at the point of chrysotile exposure (Figure 6). Incubation with deferoxamine significantly (P<0.001) diminished the capacity of chrysotile asbestos to activate the latent TGF-β1 produced by the A549 cells. This further supports the role of iron-catalyzed formation of ROS in the activation of TGF-β1.
Deferoxamine treatment decreases activation of TGF-β1. A549 cells transduced with adeno-LTGF-β1 were treated with deferoxamine (50 nM) 2 h prior to asbestos exposure and fresh deferoxamine was added at the time of asbestos exposure. Results from the ELISA show that the iron chelator significantly reduces the activation of TGF-β1 (*P<0.001). Data were collected 3 days postexposure to 10 μg/ml chrysotile asbestos. Results are representative of three experiments with a mean and s.d. of five samples.
Biological Activity of Asbestos-Activated TGF-β1 as Determined by the Mink Lung Cell Assay
Following the initial experiments with 3H-thymidine shown in Figure 1b, further studies were carried out to determine if this asbestos-induced mechanism of TGF-β1 activation is biologically relevant comparing 3H-thymidine (Figure 7a) with the PAI-Luciferase assay (Figure 7b). We performed experiments in MLEC which are well documented to exhibit reduced growth consequent to treatment with TGF-β1.27 Latent TGF-β1 transduced into these cells had little effect on cell proliferation compared to controls (Figure 7a). After chrysotile asbestos exposure, we measured a significant reduction in cell proliferation as determined by 3H incorporation. Cell proliferation was reduced significantly in cells overexpressing TGF-β1 and treated with asbestos, compared to controls, and both antioxidants and deferoxamine reversed this growth inhibition (Figure 7a).
Activation of TGF-β1 through asbestos-mediated ROS is biologically significant in mink lung cells as measured by 3H thymidine incorporation (a) and PAI-luciferase induction (b). Mink lung epithelial (MLE) cells stably transfected with PAI-luciferase were transduced with adLTGF-β1 or shuttle vector and exposed to asbestos and the antioxidants (AO) SOD+catalase or deferroxamine (DF). (a) shows significant growth inhibition, 72 h postasbestos exposure if asbestos is added to the cells producing LTGF-β compared to LTGF-β alone. This inhibition is reversed by AO or DF at 3 days. Asbestos alone produces some thymidine incorporation. Neither AO or DF increase 3H incorporation without asbestos (data not shown). Values are mean cpm (n=4)±s.d. +P<0.001 compared to adLTGF without asbestos. *P<0.001 compared to adLTGF treated with asbestos. (b) PAI-luciferase activity was significantly increased over background demonstrating activation of TGF-β1. This activity was again decreased significantly by AO or DF. Values are mean RLU (n=4)±s.d. #P<0.001 compared to AdLTGF without chrysotile treatment. *P<0.001 compared to adLTGF+chrysotile.
To determine if the decrease in cell proliferation was specific to activated TGF-β1, the same tests described above were carried out using the PAI-luciferase promoter as the measured outcome of TGF-β1 activation.27 Figure 7b shows that the time points of decreased cell growth in Figure 7a correspond with expression of luciferase, and the changes in cell growth were abrogated by treatment with antioxidants. These data support the premise that asbestos-derived ROS mediate the activation of biologically relevant TGF-β1.
Discussion
TGF-β1 is a potent inducer of extracellular matrix deposition.13 It is expressed at sites of initial lung injury in response to asbestos and other fibrogenic agents.10, 11 Our laboratory and others have demonstrated that expression of a constitutively active form of TGF-β1 through an adenovirus vector in the lungs of rats and mice induces fibrogenesis.15, 16, 31 This treatment causes scarring even in fibrogenic-resistant TNF-α double receptor KO mice.16 Similar expression of the full latent TGF-β1 complex fails to initiate this fibrogenic response.15 Because latent TGF-β1 is constitutively produced in the lung by a number of cell types, including type II epithelial cells32 and macrophages,10 it is essential that the mechanisms which free the active TGF-β1 peptide from its LAP be elucidated to understand the precise biological roles of TGF-β1. In this study, we demonstrate a mechanism of TGF-β1 activation by asbestos-derived ROS. Iron from asbestos promotes ROS formation,1 and we have shown that these molecules activate TGF-β1 in biologically relevant quantities, as demonstrated by reduced incorporation of 3H-thymidine by MLEC and a PAI-luciferase assay to demonstrate specificity of this response to active TGF-β1 (Figures 1 and 7).
Barcellos-Hoff and Dix21 first introduced the concept of oxidative activation of TGF-β1, showing that ionizing radiation or iron-derived ROS activate latent TGF-β1 both in vitro and vivo.20 Here, we offer data supporting the postulate that this mechanism of oxidative activation of latent TGF-β1 is relevant for lung cells. Asbestos is a well-documented oxidizing agent.1 The fibers can carry ferric (catalytic iron) and ferrous iron (free iron), both of which are capable of going through Fenton reactions and producing ROS in cellular and cell free systems.23 Asbestos-associated iron causes DNA strand breaks,2 increased DNA oxidation in the form of 8OH2dG,2 as well as lipid peroxidation.3 Ghio and Stonehuerner33 have shown in vitro direct oxidation and subsequent activation of complement protein (C5) by crocidolite asbestos in a concentration-dependent manner. Here, we examined the potential oxidative activation of TGF-β1 by both crocidolite and chrysotile asbestos. Although crocidolite asbestos differs significantly in its molecular structure and iron content from chrysotile (30% iron Vs 3–7%), both fibers have been implicated in ROS-induced damage and fibrosis.1 We demonstrated here that both crocidolite- and chrysotile-associated iron are capable of producing sufficient ROS to activate TGF-β1 in cell free conditions (Figure 1a). This TGF-β1 is biologically active as shown by reduced 3H-thymidine incorporation by MLEC (Figure 1b). To our knowledge, this is the first evidence that ROS generated by the iron in chrysotile or crocidolite directly activate TGF-β1, suggesting a potentially important mechanism in the development of asbestos-induced lung fibrosis or in other fibrogenic responses where ROS are being produced.
Oxidative activation of TGF-β1 is suspected because of the formation of carbonyl side chains within the protein (Figure 3). Although this form of protein oxidation is not the only type of modification which can occur, it is one of the most common.29 Carbonyls are formed through the oxidation of Lys, Arg, Pro, and Thr29 which combined make up 27% of the LAP protein. These types of modifications in amino acids are well documented to create changes in enzyme function and protein binding (for review see Shacter34). We clearly show in Figures 2 and 3 that LAP is the component which is modified by oxidation, inasmuch as the oxidized LAP is no longer able to form a complex with the TGF-β1 protein, while oxidation of TGF-β1 has no effect on its ability to complex with normal LAP. Further work is ongoing to better understand the precise nature of the amino acids of the LAP that are altered by ROS.
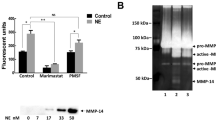
A number of agents or conditions have been demonstrated to activate TGF-β1,35 some of which (eg, pH, temperature) are not likely to be physiologically relevant. Currently, some of the most compelling work in the field centers on cellular adhesion molecules and matrix metalloproteases (MMPs). In an elegant series of experiments, Munger et al18 showed that TGF-β1 binds to the αvB6 integrin which induces a conformational change in TGF-β allowing it to be biologically active in response to injury. Further work by Mu et al19 demonstrated a mechanism of TGF-β homeostatic control of cells through αvb8 binding and subsequent cleavage of the LAP from TGF-β1 by membrane type MMP 1.19 The MMP 9 and MMP2 are also capable of LAP proteolysis and subsequent activation of TGF-β1.36
All of the established mechanisms described previously involve protein interactions or transcriptional, translational and post-translational cell-specific modifications in response to stress. In comparison, latent TGF-β1 activation by ROS is rapid and irrespective of cell type. More importantly, it is not dependent on cell surface interactions and could occur in alveolar epithelial lining fluid or in the lung interstitial vascular and lymphatic spaces. In support of this concept, patients with IPF demonstrate increased oxidant/antioxidant balance37 as well as increases of both active and latent TGF-β1 in their BAL fluids correlating with disease.38, 39 Also, in vivo models of asbestos exposure have shown excessive oxidative stress in response to the initial fiber deposition,4 and the extent of lesion formation and lung injury was ablated through the systemic administration of antioxidants.4
We showed that asbestos-derived ROS activate TGF-β1 in cell culture subsequent to growth factor transduction in A549 cells and MLE cells (Figures 4 and 7). Activation was prevented through the use of the cellular antioxidants SOD and catalase and the iron chelator deferoxamine, supporting our postulate of an oxidative pathway for TGF-β1 activation. It should be noted that asbestos also is capable of chelating intracellular iron. It is likely that the deferoxamine has chelated iron from both intra and extracellular pools and has thus prevented the formation of ROS in these experiments.
It is important to note that other TGF-β1 activating mechanisms may also be operative in culture in response to ROS. Both pro-MMP9 and pro-MMP2 are oxidatively upregulated in different cell culture systems, and it has been shown that both of these proforms can also be activated in response to ROS,40 thus offering a mechanism of TGF-β1 activation. However, in our culture system use of chelators such as EDTA failed to effectively inhibit the activation of TGF-β1 (data not shown). This is significant because EDTA is known to chelate iron but not inhibit its oxidative reactivity. At the same time, EDTA is an inhibitor of MMP activation,41 suggesting that most of the activation seen in our system is specific to an oxidative pathway.
The biological activity of ROS-activated TGF-β1 was demonstrated in two separate experiments (Figures 1 and 7). MLE cells are commonly used to quantify the amount of active TGF-β1 because proliferation of these cells is restricted in a predictable, concentration-dependant manner.27, 42 Active TGF-β1 from multiple sources has been measured in the MLE assay.42 We showed that the MLE cells were producing latent TGF-β1 through transduction by an adenovirus. Growth of these cells would not be affected unless that latent TGF-β1 was activated and consequently could bind the cognate receptors on the MLE membranes. This proved to be the case as shown in Figures 1b and 7a, where ROS derived both from a cell free system and from asbestos-induced ROS activated the TGF-β1 and blocked MLE cell growth. MLE cells also were used to test the specificity of the biological activity of the activated TGF-β1. This was accomplished through a luciferase assay which responds only to activated TGF-β1 that has bound to and transduced a signal through its membrane-bound receptors.27 Asbestos alone, and latent TGF-β1 alone induced little luciferase activity. Adding asbestos activated the TGF-β1 as measured by the luciferase assay, and this activation was blocked by the antioxidants SOD and catalase, as well as the use of deferoxamine (Figure 7). The luciferase assay tests TGF-β1 specificity through a TGF-β responsive element of the plasminogen activator inhibitor 1 (PAI-1).27 The stably transfected truncated PAI-1 TGF-β1 promoter region with a luciferase promoter (PAI/L) has been demonstrated to be very sensitive and more specific for TGF-β than other tests of biological activity such as 3H-thymidine incorporation, and is currently a widely accepted assay for active TGF-β1.
It is not known precisely how ROS activate latent TGF-β1 to its active form. It has been suggested that susceptibility to the ROS resides in the LAP molecule, which contains redox-sensitive methionines and cysteines and may have the ability to bind free iron.21 Further studies will be necessary to determine the nature of this mechanism.
We have presented evidence that asbestos-derived ROS activate TGF-β1. This could be a significant mechanism for the development of fibrogenic disease inasmuch as large amounts of latent TGF-β1 are produced by macrophages, fibroblasts and alveolar epithelial cells consequent to lung injury.10, 11, 32 Latent TGF-β1 can be recovered by lavage of patients with IPF39 and animals with fibrogenic disease,43 suggesting that latent TGF-β1 can be found in the alveolar lining layer (ALL) of the small air spaces. The ALL is known to consist of surfactant components and multiple proteins44, 45 and this is where inhaled fibers initially deposit, particularly at the alveolar duct bifurcations.46 Earlier studies showed rapid activation of the 5th component of complement by the alternative pathway as a direct result of chrysotile asbestos being deposited in the ALL.47, 48 Since latent TGF-β1 is likely to be located in this extracellular compartment, it seems likely that ROS could activate the peptide to biologically active TGF-β as we have shown here in vitro. How this active TGF-β1 could then reach the target interstitial fibroblast population is not entirely clear, but it is known that the alveolar epithelium develops abnormalities in fluid and protein exchange following lung injury,47 and the ‘fibrotic foci’ thought to be central to the development of human IPF49 are a loose meshwork of fibroblasts and matrix with little evidence of an impermeable epithelial barrier.49 Thus, it is not difficult to envision how newly activated TGF-β1 could gain access to the target mesenchymal cell population.
In summary, we have shown that latent TGF-β1 can be activated by chrysotile and crocidolite asbestos through iron-induced oxidation. Activation by this mechanism occurred in rh-TGF-β1 as well as porcine TGF-β1 transduced in both A549 and MLEC lines. The activated TGF-β1 has proven to be biologically relevant as measured by its ability to inhibit mink lung cell proliferation as well as induce the TGF-β1 specific PAI-luciferase promoter. These studies suggest that the formation of ROS consequent to exposure to an inorganic iron-containing dust plays a central role in the activation of TGF-β1 to its biologically active form. Studies are ongoing to investigate whether or not this activation mechanism is operative in vivo and plays a role in the development of interstitial fibrogenesis.
References
Kamp DW, Weitzman SA . The molecular basis of asbestos induced lung injury. Thorax 1999;54:638–652.
Kamp DW, Israbian VA, Preusen SE, et al. Asbestos causes DNA strand breaks in cultured pulmonary epithelial cells: role of iron-catalyzed free radicals. Am J Physiol 1995;268:L471–L480.
Howden PJ, Faux SP . Fibre-induced lipid peroxidation leads to DNA adduct formation in Salmonella typhimurium ta104 and rat lung fibroblasts. Carcinogenesis 1996;17:413–419.
Mossman BT, Marsh JP, Sesko A, et al. Inhibition of lung injury, inflammation, and interstitial pulmonary fibrosis by polyethylene glycol-conjugated catalase in a rapid inhalation model of asbestosis. Am Rev Respir Dis 1990;141:1266–1271.
Dai J, Churg A . Relationship of fiber surface iron and active oxygen species to expression of procollagen, PDGF-a, and TGF-beta(1) in tracheal explants exposed to amosite asbestos. Am J Respir Cell Mol Biol 2001;24:427–435.
Selikoff IJ, LD . Asbestos and Disease, Environmental Sciences. Academic Press, Inc.: New York, 1978.
Liu JY, Brass DM, Hoyle GW, et al. TNF-alpha receptor knockout mice are protected from the fibroproliferative effects of inhaled asbestos fibers. Am J Pathol 1998;153:1839–1847.
Liu J-Y, Morris GF, Lei W-H, et al. Up-regulated expression of transforming growth factor-a in the bronchiolar–alveolar duct regions of asbestos-exposed rats. Am J Pathol 1996;149:205–217.
Liu J-Y, Morris G, Lei W-H, et al. Rapid activation of PDGF-a and -b expression at sites of lung injury in asbestos-exposed rats. Am J Respir Cell Mol Biol 1997;17:129–140.
Perdue TD, Brody AR . Distribution of transforming growth factor-β1, fibronectin, and smooth muscle actin in asbestos-induced pulmonary fibrosis in rats. J Histochem Cytochem 1994;42:1061–1070.
Liu J-Y, Brody AR . Increased TGF-β1 in the lungs of asbestos-exposed rats and mice: Reduced expression in TNF-α receptor knockout mice. J Environ Pathol Toxicol Oncol 2001;20:77–87.
Chang LY, Overby LH, Brody AR, et al. Progressive lung cell reactions and extracellular matrix production after a brief exposure to asbestos. Am J Pathol 1988;131:156–170.
Massague J . TGF-beta signaling: receptors, transducers, and mad proteins. Cell 1996;85:947–950.
Bonner JC, Badgett A, Lindroos PM, et al. Transforming growth factor-beta-1 (TGF-beta-1) down-regulates the platelet-derived growth factor (PDGF) alpha-receptor subtype on human lung fibroblasts in vitro. Am J Respir Cell Mol Biol 1995;13:496.
Sime PJ, Xing Z, Graham FL, et al. Adenovector-mediated gene transfer of active transforming growth factor β1 induces prolonged severe fibrosis in rat lung. J Clin Invest 1997;100:768–776.
Liu J-Y, Sime PJ, Wu T, et al. Transforming growth factor β1 overexpression in tumor necrosis factor-α receptor knockout mice induces fibroproliferative lung disease. Am J Respir Cell Mol Biol 2001;25:3–7.
Gleizes PE, Munger JS, Nunes I, et al. TGF-beta latency: biological significance and mechanisms of activation. Stem Cells 1997;15:190–197.
Munger JS, Huang X, Kawakatsu H, et al. The integrin alpha v beta 6 binds and activates latent TGF beta 1: a mechanism for regulating pulmonary inflammation and fibrosis. Cell 1999;96:319–328.
Mu D, Cambier S, Fjellbirkeland L, et al. The integrin alpha(v)beta8 mediates epithelial homeostasis through mt1-MMP-dependent activation of TGF-beta1. J Cell Biol 2002;157:493–507.
Ehrhart EJ, Gillette EL, Barcellos-Hoff MH . Immunohistochemical evidence of rapid extracellular matrix remodeling after iron-particle irradiation of mouse mammary gland. Radiat Res 1996;145:157–162.
Barcellos-Hoff MH, Dix TA . Redox-mediated activation of latent transforming growth factor-beta 1. Mol Endocrinol 1996;10:1077–1083.
Dai J, Xie C, Churg A . Iron loading makes a nonfibrogenic model air pollutant particle fibrogenic in rat tracheal explants. Am J Respir Cell Mol Biol 2002;26:685–693.
Aust A, Lund L, Chao C-C, et al. Role of iron in the cellular effects of asbestos. Inhal Toxicol 2000;12:75–80.
Pinkerton KE, Brody AR, McLaurin DA, et al. Characterization of three types of chrysotile asbestos after aerosolization. Environ Res 1983;31:32–53.
Langer AM, Pooley FD . Electron microscopical investigation of asbestos fibers. Environ Health Perspect 1974;9:63–80.
Sullivan DE, Mondelli MU, Curiel DT, et al. Construction and characterization of an intracellular single-chain human antibody to hepatitis c virus non-structural 3 protein. J Hepatol 2002;37:660–668.
Abe M, Harpel JG, Metz CN, et al. An assay for transforming growth factor-beta using cells transfected with a plasminogen activator inhibitor-1 promoter-luciferase construct. Anal Biochem 1994;216:276–284.
Lund LG, Aust AE . Iron mobilization from asbestos by chelators and ascorbic acid. Arch Biochem Biophys 1990;278:61–64.
Shacter E . Protein oxidative damage. Methods Enzymol 2000;319:428–436.
Shatos MA, Doherty JM, Marsh JP, et al. Prevention of asbestos-induced cell death in rat lung fibroblasts and alveolar macrophages by scavengers of active oxygen species. Environ Res 1987;44:103–116.
Warshamana GS, Pociask DA, Fisher KJ, et al. Titration of non-replicating adenovirus as a vector for transducing active TGF-beta1 gene expression causing inflammation and fibrogenesis in the lungs of c57bl/6 mice. Int J Exp Pathol 2002;83:183–201.
Khalil N, O'Connor RN, Flanders KC, et al. TGF-β1, but not TGF-β2 or TGF-β3, is differentially present in epithelial cells of advanced pulmonary fibrosis: an immunohistochemical study. Am J Respir Crit Care Med 1996;14:131–138.
Ghio AJ, Stonehuerner J . Complement activation after in vitro asbestos exposure corresponds to oxidant generation by the fiber. Inhal Toxicol 1997;9:31–34.
Shacter E . Quantification and significance of protein oxidation in biological samples. Drug Metab Rev 2000;32:307–326.
Brown PD, Wakefield LM, Levinson AD, et al. Physicochemical activation of recombinant latent transforming growth factor-beta's 1, 2, and 3. Growth Factors 1990;3:35–43.
Yu Q, Stamenkovic I . Cell surface-localized matrix metalloproteinase-9 proteolytically activates TGF-beta and promotes tumor invasion and angiogenesis. Genes Dev 2000;14:163–176.
Beeh KM, Beier J, Haas IC, et al. Glutathione deficiency of the lower respiratory tract in patients with idiopathic pulmonary fibrosis. Eur Respir J 2002;19:1119–1123.
Fahy RJ, Lichtenberger F, McKeegan CB, et al. The acute respiratory distress syndrome: a role for transforming growth factor-beta 1. Am J Respir Cell Mol Biol 2003;28:499–503.
Yamauchi K, Martinet Y, Basset P, et al. High levels of transforming growth factor-beta are present in the epithelial lining fluid of the normal human lower respiratory tract. Am Rev Respir Dis 1988;137:1360–1363.
Yoon S-O, Park S-J, Yoon SY, et al. Sustained production of hydrogen peroxide activates pro-matrix metalloproteinase-2 through receptor kinase/phosphatidylinositol 3-kinase/nf-kb pathway. J Biol Chem 2002;277:30271–30282.
Johnson S, Knox A . Autocrine production of matrix metalloproteinase-2 is required for human airway smooth muscle proliferation. Am J Physiol 1999;277:L1109–L1117.
van Waarde MA, van Assen AJ, Kampinga HH, et al. Quantification of transforming growth factor-beta in biological material using cells transfected with a plasminogen activator inhibitor-1 promoter-luciferase construct. Anal Biochem 1997;247:45–51.
Maeda A, Ishioka S, Taooka Y, et al. Expression of transforming growth factor-beta1 and tumour necrosis factor-alpha in bronchoalveolar lavage cells in murine pulmonary fibrosis after intraperitoneal administration of bleomycin. Respirology 1999;4:359–363.
Kikkawa Y, Smith F . Cellular and biochemical aspects of pulmonary surfactant in health and disease. Lab Invest 1983;49:122–139.
Khan M, Gallagher J, Brody A . Effect of proteins and lipids of the alveolar lining layer on particle binding and phagocytosis. Toxicol In Vitro 1990;4:93–101.
Brody AR, Hill LH, Adkins Jr B, et al. Chrysotile asbestos inhalation in rats: deposition pattern and reaction of alveolar epithelium and pulmonary macrophages. Am Rev Respir Dis 1981;123:670–679.
Warheit DB, George G, Hill LH, et al. Inhaled asbestos activates a complement-dependent chemotactic factor for macrophages. Lab Invest 1985;52:505–514.
Warheit DB, Hill LH, George G, et al. Time course of chemotactic factor generation and the corresponding macrophage response to asbestos inhalation. Am Rev Respir Dis 1986;134:128–133.
Pardo A, Selman M . Idiopathic pulmonary fibrosis: new insights in its pathogenesis. Int J Biochem Cell Biol 2002;34:1534–1538.
Acknowledgements
We wish to thank Dr Jack Gauldie (McMaster University, Hamilton, Ontario) for the adenovirus vector AdTGF-β1. We also thank Ms Odette Marquez for secretarial assistance in preparation of the manuscript. This work was supported by NIH Grants RO1ES60766, RO1HL60532, LaBOR HEF from Louisiana, and Tulane Cancer Center Matching Funds.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pociask, D., Sime, P. & Brody, A. Asbestos-derived reactive oxygen species activate TGF-β1. Lab Invest 84, 1013–1023 (2004). https://doi.org/10.1038/labinvest.3700109
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700109
Keywords
This article is cited by
-
TGFβ signaling networks in ovarian cancer progression and plasticity
Clinical & Experimental Metastasis (2021)
-
Endothelial-to-mesenchymal transition in anticancer therapy and normal tissue damage
Experimental & Molecular Medicine (2020)
-
Metabolic rewiring and redox alterations in malignant pleural mesothelioma
British Journal of Cancer (2020)
-
Redox regulation in tumor cell epithelial–mesenchymal transition: molecular basis and therapeutic strategy
Signal Transduction and Targeted Therapy (2017)
-
Fructose-1,6-bisphosphate reverts iron-induced phenotype of hepatic stellate cells by chelating ferrous ions
BioMetals (2017)