The discomfort of internal gastrointestinal examination may soon be a thing of the past.
Abstract
We have developed a new type of endoscopy, which for the first time allows painless endoscopic imaging of the whole of the small bowel. This procedure involves a wireless capsule endoscope and we describe here its successful testing in humans.
Similar content being viewed by others
Main
The invention of fibre-optic endoscopy1 made visualization of the whole stomach, upper small bowel and colon possible. The procedures used to examine these (gastroscopy, small-bowel endoscopy and colonoscopy, respectively) cause discomfort because they require flexible, relatively wide cables to be pushed into the bowel — these cables carry light by fibre-optic bundles, power and video signals. Small-bowel endoscopy in particular is constrained by problems of discomfort and limitations of how far enteroscopes can be advanced into the small bowel. There is a clinical need for improved methods of examining the small bowel and colon, especially in patients with recurrent gastrointestinal bleeding.
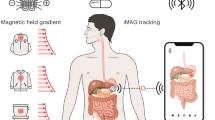
The invention of the transistor made it possible to design swallowable electronic radio-telemetry capsules for the study of gastrointestinal physiological parameters. These capsules were first reported in the 1950s and were used to measure temperature2, pressure2,3 and pH3,4. We have developed and tested a new type of videotelemetry capsule endoscope that is small enough to be swallowed (11×30 mm) and has no external wires, fibre-optic bundles or cables. By using a lens of short focal length, images are obtained as the optical window of the capsule sweeps past the gut wall, without requiring air inflation of the gut lumen. The capsule endoscope is propelled by peristalsis through the gastrointestinal tract and does not require a pushing force to propel it through the bowel.
The video images are transmitted using UHF-band radio-telemetry to aerials taped to the body which allow image capture, and the signal strength is used to calculate the position of the capsule in the body (see Supplementary Information); the images are stored on a portable recorder. This system allows more than 5 hours of continuous recording. The patient need not be confined to a hospital environment during the examination and is free to continue his or her daily routine.
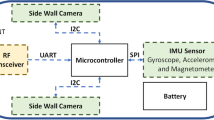
The design of the video capsule was made possible by progress in the performance of three technologies: complementary metal oxide silicon (CMOS) image sensors, application-specific integrated circuit (ASIC) devices, and white-light-emitting diode (LED) illumination. Novel optical design, better energy management and overall system design were also important in creating the capsule.
The addition of a buffer amplifier on each pixel reduced the output noise that was initially associated with CMOS image sensors and has allowed CMOS chips to achieve an image quality comparable to those of charge-coupled device image sensors5, but using much less power.
Advances in ASIC design allowed the integration of a very small video transmitter of sufficient power output, efficiency and bandwidth into the capsule. Synchronous switching of the LEDs, the CMOS sensor and the ASIC transmitter minimize power consumption. By careful design of the optics, we were able to eliminate internal reflections which are a common problem when the illumination and imager are incorporated under the same dome.
With ethical committee approval, the first studies were performed on ten normal human volunteers. The capsule was easily swallowed and caused no discomfort. Propelled by peristalsis (see Supplementary Information), it successfully transmitted video images (Fig. 1) from the stomach, small bowel and caecum (mean gastric transit time was 80 min, range 17–280 min; mean small-bowel transit time was 90 min, range 45–140 min; mouth-to-evacuation time was 24 h, range 10–48 h). High-quality images were received throughout the video transmissions, lasting up to 6 hours.
a,b, Gastric folds in the body of the stomach; c,d, villous pattern of the small bowel enhanced by the presence of a little water and an air bubble in the lumen; e,f, airless images of normal jejunum, viewed with the lumen closed in front of the optical dome of the capsule; g,h, views of the terminal ileum.
References
Hopkins, H. H. & Kapany, N. S. Nature 173, 39–41 (1954).
Zworkin, V. K. Nature 179, 898 (1957).
Mackay, R. S. & Jacobson, B. Nature 179, 1239–1240 (1957).
Noller, H. G. Deutsche Med. Wsch. 85, 1707 ( 1960).
Fossum, E. R. Proc. SPIE 1900, 2–14 ( 1993).
Author information
Authors and Affiliations
Supplementary information
Rights and permissions
About this article
Cite this article
Iddan, G., Meron, G., Glukhovsky, A. et al. Wireless capsule endoscopy. Nature 405, 417 (2000). https://doi.org/10.1038/35013140
Issue Date:
DOI: https://doi.org/10.1038/35013140
This article is cited by
-
A stress test for bioelectronics
Nature Electronics (2024)
-
Serum food specific IgG antibodies are associated with small bowel inflammation in patients with Crohn’s disease
European Journal of Clinical Nutrition (2024)
-
ViTCA-Net: a framework for disease detection in video capsule endoscopy images using a vision transformer and convolutional neural network with a specific attention mechanism
Multimedia Tools and Applications (2024)
-
Modeling and Experimental Validation of Anchoring Resistance of the Radial Expanding Capsule Robot in the Intestine
Tribology Letters (2024)
-
Evaluation of symptomatic small bowel stricture in Crohn’s disease by double-balloon endoscopy
BMC Gastroenterology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.