Abstract
Study Design:
Case report.
Settings:
Department of Neurosurgery, Imam Hospital, Faculty of Medicine, Tabriz University of Medical Sciences, Daneshgah Street, Tabriz, East Azerbayjan, Iran.
Report:
A 21-year-old man presented with progressive paraesthesia and weakness in the four limbs, with disturbances in the vibration and positional senses. Magnetic resonance imaging revealed a cervical intramedullary tumour from the cervicomedullary junction to C3. Radical resection of the tumour was performed and histology revealed a meningioma. His clinical outcome after a 3-year follow-up is relatively good.
Conclusion:
Intramedullary cervical meningiomas are very rare and have been reported only five times before. Because of its tendency to recur after surgery and because of a possible aggressive behaviour, meticulous histopathological examination is mandatory to predict the evolution and plan the follow-up. Outcome is mainly related to the type of tumour and the complete removal.
Similar content being viewed by others
Introduction
Meningiomas are among the most common benign tumours of the spinal canal in adults,1 found predominantly in the thoracic segments (80%). Clear cell meningioma is an aggressive variant with a predilection for the cauda equina.2 Magnetic resonance imaging (MRI) can show an intradural-extramedullary location.1 Gadolinium enhancement helps in the diagnosis.
According to the literature, the occurrence of an intramedullary cervical meningioma is very rare, with only five cases reported in the literature so far.1, 2, 3 We present the sixth case and review the previous reports.
Case report
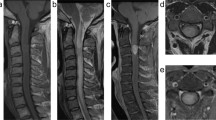
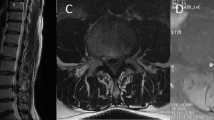
A 21-year-old man presented with gradual numbness and parenthesis in the four limbs, particularly in the left leg and progressive difficulty in walking over a 2-year period. Physical examination detected spastic paraparesis, hyper-reflexia, impaired position and vibration senses, clonus, extensor plantar reflexes, and spastic gait MRI showed an intramedullary mass in the cervical cord with perifocal oedema, extending from the cervicomedullary junction to C2 (Figure 1). The tumour was isointense on T1 and iso- to hyperintense onT2-weighted images (Figure 1). Homogeneous enhancement with gadolinium on T1-weighted images was evident (Figure 2).
Sagittal T2-weighted (a) and T1-weighted (b) MRI of the cervical cord reveals isointense and iso- to hyperintense intramedullary tumour at the level of C1 and C2. Tumour-related expansion of the cord and a developed syringomyelia are also evident. Note oedema of the cord at the distance between the tumour and the syrinx, which is apparent on T2-weighted MRI (a). Sagittal T2-weighted MRI (c) of the cervicomedullary showing tumour extension up to the cervicomedullary junction and associated oedema. MRI, magnetic resonance imaging.
The tumour was subtotally resected through suboccipital craniotomy and C1–C2 laminectomy, applying a Cavitron ultrasound surgical aspirator under operating microscopy.
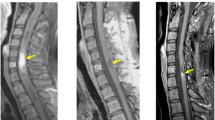
Histopathological examination confirmed a syncytial-type meningioma (World Health Organization Grade I). Immunohistochemical staining was positive for epithelial membrane antigen and S-100 protein (Figure 3).
Discussion
To date, only five documented intramedullary spinal meningioma in the cervical cord have been described in the literature (Table 1). An age range from 22 months to 67 years has been reported (Table 1). Possible risk factors may be trauma, viral infections, irradiation or genetic mutations.
Three of the five previously described patients were female. With this patient, sex ratio will become equal but with a predilection for female gender during the fifth to seventh decades of life (Table 1).
The insidious onset with neck pain, dysesthesia, motor deficits and urinary retention has been described. Our patient suffered from simultaneous sensory and motor deficits.
The tumour is more common in the upper cervical levels (Table 1). Moriuchi et al.3 reported a case of intramedullary meningioma with extension beyond the cervicomedullary junction into the medulla oblongata. This makes total resection less probable.
The subtypes of intramedullary cervical meningioma included fibroblastic,1 clear cell,2 transitional,3 angioblastic4 and papillary meningioma.5 Our case is the first meningothelial intramedullary meningioma in the cervical cord.
Clear cell and angioblastic subtypes have been associated with a less favourable outcome (Table 1). Jallo et al.2 recommend treating these tumours aggressively with MRI follow-up every 3–6 months during the first years and annually, thereafter. Concurrent involvement of the medulla oblongata contributes to a less favourable outcome.
After 3 years, our patient shows no recurrence, but long-term follow-up has to be awaited. Imaging characteristics of intramedullary meningioma have not been well described and only two previous patients had spinal MRI. Salvati et al.1 do not mention MRI specifications in their two cases. Moriuchi et al.3 showed spinal cord expansion and homogeneously enhanced intramedullary tumour extending up to the medulla oblongata. Our case provides additional data on imaging of these rare tumours in the cervical region (Figures 1, 2 and 3).
Conclusion
Intramedullary cervical meningioma is a very rare clinical entity. When confronting a homogenously enhanced intramedullary tumour of the cervical cord on post-contrast MRI, meningioma should be included in the differential diagnoses. Because of high recurrence after surgery and aggressive behaviour of some variants, meticulous histopathological examination is mandatory to predict evolution and plan follow-up. Total resection of the tumour is the treatment of choice.
References
Salvati M, Artico M, Lunardi P, Gagliardi FM . Intramedullary meningioma: case report and review of the literature. Surg Neurol 1992; 7: 42–45.
Jallo GI, Kothbauer KF, Silvera VM, Epstein FJ . Intraspinal clear cell meningioma: diagnosis and management: report of two cases. Neurosurgery 2001; 8: 218–221.
Moriuchi S, Nakagawa H, Yamada M, Kadota T . Intramedullary spinal cord meningioma—a case report. Neurol Med Chir (Tokyo) 1996; 36: 888–892.
Pansini A, Conti P . On some rare spreading cervical lesions. J Neurosurg Sci 1981; 25: 255–257.
Pagni CA . I Meningioma Spinali. CIC Edizioni Internazionali: Roma, 1989, 1–249.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salehpour, F., Zeinali, A., Vahedi, P. et al. A rare case of intramedullary cervical spinal cord meningioma and review of the literature. Spinal Cord 46, 648–650 (2008). https://doi.org/10.1038/sj.sc.3102175
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102175
Keywords
This article is cited by
-
A rare case of intramedullary ‘whorling-sclerosing’ variant meningioma
SpringerPlus (2015)