Abstract
Study design:
Case report.
Clinical setting:
Johns Hopkins University School of Medicine, Baltimore, MD, USA.
Case report:
Sarcoidosis is a multi-system granulomatous disease of unknown etiology with worldwide distribution. The involvement of the nervous system is common—neurosarcoidosis. Immune responses play an important role in the inflammatory process and granuloma formation. We report a case of neurosarcoidosis that was refractory to two courses of intravenous steroids. Upon initiation of oral thalidomide, the patient showed dramatic improvement clinically and on magnetic resonance imaging.
Conclusion:
Thalidomide is an immunomodulatory agent that acts to inhibit production of tumor-necrosis factor-α (TNF-α), an important mediator in CNS inflammation, by enhancing TNF-α mRNA degradation. Corticosteroids have been the mainstay of treatment of neurosarcoidosis with success at halting progression of the immune process in 50% cases. Thalidomide offers unique opportunities at managing CNS inflammation due to neurosarcoidosis.
Disclosures:
None.
Similar content being viewed by others
Case report
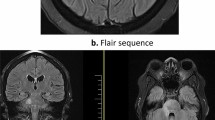
A 42-year-old African-American male, with no significant past medical history, developed acute onset numbness of his left then bilateral toes that progressed over four weeks extending to the waist. One week after the onset of symptoms, the patient noted bilateral stiffness in the thighs, feet dragging, tingling sensation in both hands, bladder urgency and Lhermitte's phenomenon. An episode of sneezing brought on acute onset of neck pain, radiating down the scapular region and posterior part of both arms. Gait imbalance and sensory symptoms in the lower extremities worsened over the next few days. Physical examination revealed 3+ reflexes in the left patella, Babinski on the left, 4+/5 strength in the left upper and lower extremity and pinprick sensation was decreased from C5–T4 and the right leg. Vibration was decreased in the entire left leg and mildly impaired in the right toes. Propioception was impaired bilaterally. Initial magnetic resonance imaging (MRI) done revealed increased T2 signal from the cervicomedullary junction to the T4 level, edematous expansion of the cord and intense nodular enhancement (Figure 1). He was treated with i.v. dexamethasone 4 mg 6 hourly with no improvement in symptoms.
A repeat MRI of the brain and the C-spine after one week revealed no change. Lumbar puncture showed clear cerebrospinal fluid with seven WBCs mostly lymphocytes and no RBCs. NMO-IgG was negative. The complete blood count, comprehensive metabolic profile, ACE, B12 and folate were normal. ANA, Lyme antibody, RPR and HIV were negative. Chest CT scan showed small mediastinal nodes, nonspecific in etiology. FDG PET/CT scan done demonstrated intense FDG uptake in multiple mediastinal and bilateral hilar lymph nodes, consistent with sarcoidosis. Mediastinoscopy with biopsy revealed non-necrotizing granulomatous lymphadenitis negative for acid-fast bacilli and fungi, confirming the diagnosis of sarcoidosis. He was started on 1 g Solumedrol i.v. daily for 5 days with no improvement. A repeat MRI 23 days later showed no change in the enhancing lesion and the physical examination showed slightly worse strength with 4-/5 MRC score in the left upper and both lower extremities.
Thalidomide was started at 400 mg orally daily for a course of 30 days. At 4 days after initiation of thalidomide, the patient reported reduced dysesthesias and 1 week after initiation, examination revealed normal strength in both lower extremities but persistent sensory changes as before. Proprioception improved beginning 1 week after initiation of thalidomide. Four weeks into thalidomide treatment, the MRI showed significant improvement with marked reduction in enhancement and edematous expansion of the cord. Vibration and pinprick sensation continued to improve steadily, 10 weeks into thalidomide treatment.
Discussion
Systemic corticosteroids and immunosuppressive therapy are the treatment of choice for neurosarcoidosis. However, this is associated with a slow response and 50% progression in disease.1 Spinal neurosarcoidosis may present as an idiopathic inflammatory demyelinating disease both clinically and radiologically.2
Thalidomide is an immunomodulatory agent that acts to inhibit production of TNF-α, an important mediator in CNS inflammation, by enhancing TNF-α mRNA degradation.3 Thalidomide inhibits the upregulation of IL-6 and downregulates nuclear factor-κB activity, both of which are elevated and important in the CNS inflammatory process seen in neurosarcoidosis.4, 5
In our patient, we cannot rule out that the improvement noted clinically and radiologically after initiation of thalidomide was simple natural course of disease, which includes spontaneous remissions and relapses, or a delayed response to steroids. However, the failure to respond clinically and radiologically to i.v. steroids over the next 23 days and the prompt response after thalidomide argues that for some patients, thalidomide may be an effective treatment for neurosarcoid exacerbations. We propose that thalidomide offers unique opportunities at resolving acute CNS inflammation due to neurosarcoidosis.
References
Zajicek JP et al. Central nervous system sarcoidosis—diagnosis and management. Q J Med 1999; 92: 103–117.
Kumar N, Frohman EM . Spinal neurosarcoidosis mimicking an idiopathic inflammatory demyelinating syndrome. Arch Neurol 2004; 61: 586–589.
Moreira AL, Sampaio EP, Zmuidzinas A, Frindt P, Smith KA, Kaplan G . Thalidomide exerts its inhibitory action on tumor necrosis factor alpha by enhancing mRNA degradation. J Exp Med 1993; 177: 1675–1680.
Mitsiades N et al. Apoptotic signaling induced by immunomodulatory thalidomide analogs in human multiple myeloma cells: therapeutic implications. Blood 2002; 99: 4525–4530.
Moreira AL et al. Effect of cytokine modulation by thalidomide on the granulomatous response in murine tuberculosis. Tuber Lung Dis 1977; 78: 47–55.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hammond, E., Kaplin, A. & Kerr, D. Thalidomide for acute treatment of neurosarcoidosis. Spinal Cord 45, 802–803 (2007). https://doi.org/10.1038/sj.sc.3102115
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102115