Abstract
Objective and importance:
Involvement of cervical spinal cord by Actinomycosis and consequent cord compression is a rare presentation. As the organism is located in nose and throat, the face and jaw area is commonly affected. Involvement of cervical cord has been rarely recorded. We are reporting this case because of the rarity of area of the involvement and have reviewed literature.
Clinical presentation:
A 30-year-old male with multiple discharging sinuses on the nape of neck and upper back for 7 years which resulted in cervical cord compression and spastic paraperesis. Tissue biopsy from the site of discharging sinuses revealed Actinomycosis. Patient responded to the medical therapy with penicillin and power in lower limbs was improved. The local lesion was also reduced.
Intervention:
Medical therapy with penicillin and surgical decompression forms the mainstay of treatment.
Conclusion:
A high degree of suspicion and demonstration of organism by biopsy or culture is essential for treatment. Penicillin is highly effective and should be given for long duration for optimal results.
Similar content being viewed by others
Case report
A 30-year-old male farmer had complaints of multiple discharging sinuses over the nape of neck and upper back of 7 years duration (Figure 1). He was being treated for a differential diagnosis of Scrofuloderma and fungal mycetoma with four drug AKT, IV streptomycin, Rifampicin, steroids and Dapsone at various medical centres. However the discharging sinuses did not heal. A tissue biopsy performed did not reveal any confirmative diagnosis. He was then referred to our institute. On local examination, he had a large erythmatous indurated plaque like lesion over the nape of neck and upper back with multiple purulent discharging sinuses. There were multiple enlarged matted cervical nodes palpable. A tissue biopsy was performed, which showed epidermis with acanthosis, bridging of rete ridges and dermis showed abscess formation with blue filamentous colonies surrounded by the eosinophilic and inflammatory material in the centre confirming the diagnosis of Actinomycosis (Figure 2). Subsequently, he was put on IV penicillin (4 million units 6hourly for 3 months) after which he was shifted to penicillin V 2.4 g daily. The skin lesion reduced in extent, and patient was discharged from the hospital to be readmitted within 6 weeks with complaints of sudden onset pain in both upper and lower limbs and inability to walk or stand without support. The neck movements were restricted. Neurological examination revealed a spastic gait and grade III power (MRC grading) in the lower limbs. Power in upper limbs was grade IV (MRC grading). All deep tendon reflexes were brisk. Sensations were intact except the loss of vibration sense up to knee bilaterally. His total leukocyte count was 11 000 with 84% polymorphs. There was no serological evidence of immunosupression.
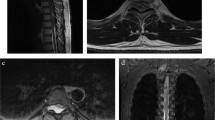
A MRI of Cervical spine showed evidence of altered signal intensity in the subcutaneous tissue and muscle planes which was isointense on T1W images and hyperintense on T2W images and showed post contrast enhancement. There was an epidural plaque like lesion from C6 to D3 level extending all around the spinal cord causing compression (Figure 3).
As the tissue biopsy was conclusive of Actinomycosis the same diagnosis was considered for the Cervicodorsal epidural lesion. As the nape of neck was involved with discharging sinuses surgical decompression was differed and the patient was started on medical line of treatment with IV Penicillin, and IV methyl prednisolone. Patient showed significant clinical improvement after 1 week of therapy and was ambulatory without support.
Discussion
Actinomycosis involving the cervico dorsal spinal cord and causing compression is rare. Oruckaptan et al1 have recorded a total of 11 cases in the world literature. Eftekhar et al2 found only 13 cases with actinomycosis related spinal neurological deficit. First reported case of an epidural spinal abscess owing to Actinomycosis, which required surgical drainage and use of IV penicillin (first since its advent) was in 1981.3 Actinomycosis is mainly caused by Actinomyces Israelii species. A naeslundii, A odontolyticus, A viscosus and A meyeri are less commonly involved. However, most of the infections are polymicrobial.4 Males are more commonly affected and the peak incidence is in middle age. The companion bacteria appear to act as copathogens that enhance the relatively low invasive power of actinomycosis. Specifically, they are responsible for the early manifestations of the infection and for treatment failures. Organisms are present in the normal flora of oral cavity, gastrointestinal and the urinary tract. The endogenous infection is caused after trauma and tissue necrosis or in presence of immune suppression.4 The infection spreads following the disruption of the mucosal barriers. Once infection is established, the host mounts an intense inflammatory (ie, suppurative, granulomatous) response. The initial acute phase is followed by a chronic indolent phase causing fibrosis, indurations and finally forming draining sinuses. The features of infection may mimic malignancy or other chronic infections.2, 5 Involvement of the spine and the central nervous system may result from direct spread of infection along connective tissue planes, through foramina at the base of the cranium, or by way of the intervertebral foramina. The spinal dura consists of a tight barrier preferring epidural abscess3, 6 and granulation tissue3, 5 formation rather than intrathecal empyema, which is a very rare clinical presentation. Such a fulminant lesion can remain localized for many years without causing any systemic effects as was seen in this patient who had the discharging sinuses for 7 years.
Confirmation of diagnosis is based on tissue biopsy and culture; however, the bacteriological isolation of organism is possible only in a minority of cases and is often precluded by prior administration of antibiotics. The smear, therefore, should be obtained before starting antibiotic therapy.1
Medical therapy with IV penicillin is very effective and should be started as first-line therapy, even in the extensive disease. Surgical decompression of the cord is recommended if there is rapid deterioration in the neurological status, patients with localized abscess a non-response to antibiotics.1, 7 In our case report, surgery was deferred as the skin was involved with purulent discharging sinuses. As the patient's neurological condition was static, only medical treatment with penicillin was continued and the patient showed gradual improvement.
Conclusion
Cervical cord Actinomycosis is a rare clinical presentation and therefore is difficult to diagnose. A high degree of suspicion and demonstration of organism by biopsy or culture is essential for treatment. Penicillin is highly effective and should be given for long duration for optimal results.
References
Oruckaptan HH, Senmevsim O, Soylemezoglu F, Ozgen T . Cervical actinomycosis causing cord compression and multi segmental root failure. Neurosurgery 1998; 43: 937–940.
Eftekhar B, Ketabachi E, Ghodsi M, Ahmadi A . Cervical epidural actinomycosis. J Neurosurgery 2001; 95 (1 Suppl): 132–134.
Kannangara DW, Tanaka T, Thadepalli H . Spinal epidural abscess due to actinomyces Israelii. Neurology 1981; 31: 202–204.
Russo T . Actinomycosis Harrison's principles of internal medicine, 15th edn. The McGraw Hills Companies, Inc., USA. International Edition ISBN 0-07118319-1, 2001, pp. 1008–1011.
Wolfe M, Israel J . Ueber reincultur des actinomyces und seine uebertragbarkeit auf thiere virchows arch. Pathol Anat 1891; 126: 11–59.
Cope VZ . Actinomycosis of the bone with special reference to the infection of the vertebral column. J Bone Joint surgery Br 1951; 33: 205–214.
Yang BC, Cheng JC, Chan TT, Loke TK, Lo J, Lau PY . Aggressive thoracic actinomycosis complicated by vertebral osteomylitis and epidural abscess leading to spinal cord compression. Spine 2000; 25: 745–748.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Vernon, V., Pranav, G. & Palande, D. Actinomycosis of the neck causing cervical epidural cord compression. ‘A case report and review of literature’. Spinal Cord 45, 787–789 (2007). https://doi.org/10.1038/sj.sc.3102048
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102048