Abstract
Study design:
Postal survey from August 2004 to May 2006.
Objective:
To ascertain the morbidity trends in individuals with paraplegia in India and to find its association with demographic characteristics.
Settings:
India.
Methods:
The questionnaire was mailed to the identified individuals (n=600) whose addresses were obtained from the medical records section of our hospital and by contacting non-government organizations (NGOs), working for individuals with paraplegia in various cities. The causes of morbidities surveyed were respiratory complications, use of catheter, pressure sores, spasticity, postural hypotension, pain and fractures. Data were analysed using nonparametric test of association (Goodman Kruskal Tau).
Results:
A total of 276 (46%) individuals responded. Of all the morbidities studied, pain was the leading cause (57.2%) followed by spasticity (39.1%), pressure sore (28.3%), postural hypotension (10.1%), respiratory complications, and fractures (5.8%). We found significant associations between various morbidities and demographics and between morbidities themselves.
Conclusion:
The most common cause for morbidity was pain. Ambulation reduced the incidence of secondary complications.
Sponsorship:
This study was funded in part by Indian Association of Physiotherapists.
Similar content being viewed by others
Introduction
By conservative estimates, approximately 200 000 individuals with spinal cord injury (SCI) live in India. Every year, 10 000 new individuals are added to this number. The majority of these clients seek repeated medical treatment lifelong owing to various morbidities.1
Despite new technology and rehabilitative strategies, the quality of life of this population is not on par with global standards. This is partly owing to the fact that the majority of subjects with SCI in India are rural-based, living below the poverty line and are unable to afford the cost of rehabilitation. In addition, >50% of the patients get adequate rehabilitation during initial hospitalization, 81.82% of institutions have no facilities for a pre-discharge home visit by staff to understand specific requirements of the patients, and 73.9% of institutions have no facilities for follow-up home care services.2
Retrospective data from our hospital, which is a tertiary referral centre catering to an approximate population of 25 million in southwestern India; showed that many of the SCI victims sought rehospitalization for preventable complications. These included respiratory, urinary, pressure sores, postural hypotension, spasticity, pain and fractures.These findings could not be compared to the national status as no reliable statistics exist.
Causes of morbidities reported in literature in recent years are urinary tract infections (57%)3 pressure sores (6.1–63.9%),4 postural hypotension,5 pulmonary complications (50–67%),6 problematic spasticity (12–37%),7 pain (34–94%),8 and fractures (1.5–6%).9 There is no reported literature on the incidence of these morbidities in India or in fact of other nations in the region. Hence, the magnitude of the problem in this part of the world is unclear. It is intuitive to assume that repetitive occurrence of morbidities would affect the overall quality of life of the individual. This is especially so when the cost of hospitalization causes iatrogenic poverty.10
Many of the morbidities of SCI are mediated by socio–cultural factors and thus may vary from country to country. Many factors are preventable with ongoing education and public health measures. To initiate these strategies, it is necessary to establish trends of morbidities and the magnitude of each in our country.
This study aims to ascertain the morbidity trends in individuals with paraplegia in India and to evaluate associations with demographic characteristics. The morbidities studied were respiratory complications, continuous use of catheter, pressure sores, postural hypotension, pain, spasticity and fractures. Use of catheter was considered as morbidity because it is well established that long-term use of catheter predisposes to urinary infections.
Methods
Study design
Postal survey.
Subjects
Individuals with paraplegia of any cause, either gender with evidence of complete cord lesion who were 18 years or older were selected. Subjects included were community dwelling as well as institutionalized individuals.
Study period
1 August 2004 to 31 May 2006.
Procedure
Part I: Development of questionnaire and validation
We developed a questionnaire in English, which was constructed at the language level of third-grade education. The questionnaire was evaluated for face validity by five physiotherapists. Each of the physiotherapists had a minimum of 5 years working experience with SCI including community-based work with this population. The suggestions put forth by the evaluators were incorporated and the revised questionnaire was pilot tested on 10 SCI individuals for comprehensibility. Changes suggested were incorporated and this version was again pilot-tested on five patients who had not participated in the first pilot testing. The final version was translated into Indian languages by means of parallel back translation ensuring that the language level was maintained at the third grade level in all languages. The final versions of the questionnaire consisted of three sections. The first section included demographic and disease characteristics,namely age, gender, education, occupation, level of lesion, duration since injury and ambulation status. The expected responses to this section were open ended except ambulation status, which was dichotomous (walking/not walking).
The second section consisted of questions regarding occurrence of morbidities, namely respiratory dysfunction, continuous use of catheter, pressure sores, postural hypotension, pain, spasticity, and fractures. The responses to this section were dichotomous (present/absent) except in the case of pain and fractures. The instructions pertaining to pain consisted of presence/absence as well as site of pain. The instructions pertaining to fractures consisted of ‘have sustained fractures/never sustained fractures’; in case of the former response, information on the number of times and sites of occurrence of fractures were requested. Instructions clearly stated that questions on pain and fractures were related to those that had occurred after the initial insult and not those that may have occurred concurrently with the initial cord injury.
The third section consisted of details of employment following the SCI. The responses to this section were open-ended.
Part II: Administration of questionnaire
Owing to the absence of a national database on SCI, addresses of potential subjects were collected from hospitals, organizations and associations dedicated to the SCI population. Addresses of individuals living in 20 of 28 states in India were collected. The questionnaire in English and the relevant regional language was mailed to the identified individuals (n=600). The mail packet included a covering letter in English and the regional language, clearly outlining the purpose of the questionnaire, the subject's option to participate or not, and the expected return date; the questionnaire itself with instructions for completion and a reply paid self-addressed envelope. One reminder was sent a week after the expected date of reply had passed. Those subjects who did not respond to the reminder were not contacted again.
Data analysis
Demographic data even those that were ordinal in nature were pooled into categories for ease of analysis. However, owing to the lack of substantial number of subjects, all groups were not of equal intervals. The demographic data were analysed using descriptive statistics. Associations of morbidity factors with demographic characteristics was carried out using λ coefficient of association for categorical data.
Results
Response rate
Of the 600 individuals to whom the questionnaire was mailed, 276 responded (response rate of 46%). Of the 276 questionnaires that were received, 52% of questionnaires had one or more questions that were not completed or were completed inappropriately. Incomplete or inappropriate responses were grouped under a category as ‘not mentioned’. The questions that were not answered correctly were as follows:
Level of lesion: 14.5% of individuals did not mention the level of lesion.
Etiology: 37.7% of individuals either did not mention the etiology or answered nonspecifically. The nonspecific responses were ‘injury to spinal cord’ or ‘back injury’.
Demographic characteristics
Age of the subjects was categorized into groups for ease of analysis. Likewise, other characteristics such as education, occupation, and disease characteristics were also categorized. Demographic details are described in Table 1. The maximum number of subjects were in the groups of 18–<25 years (19.2%) and 40–<50 years of age (19.2%). In the present study, 34.8% of individuals were engaged in manual jobs with 53.6% of individuals having secondary school education.
Table 2 describes the disease characteristics of surveyed subjects. As can be seen from the table, subjects who had sustained lumbar lesions and who were 1–3 years post-injury were more likely to be ambulating. There were a significant number of ambulators who were 7 years post-injury. This factor could not be explained, as the patient characteristics of this group did not vary from the characteristics of the subjects in the other groups.
Morbidity trends
The various causes for morbidity that we surveyed are described in Table 3. Table 3 shows the trends of morbidities other than pain with respect to duration and level of injury. Spasticity was the leading cause of morbidity at all the levels except at the lower thoracic level, where pressure sore was the leading cause. All the complications were more common in the ‘<2 years and >5 years post-injury’ groups.
Table 4 shows the trends of pain distribution with respect to duration and level of injury. Pain was the leading cause of morbidity in the present study. Pain was more common among the individuals who had sustained a lesion at the lumbar level. This could be owing to the fact that 60.1% of the subjects had a lumbar lesion. Pain in the back and chest was more common in the <2-year post-injury group. Shoulder and upper limb pain was more common in the more than 2-year post-injury group.
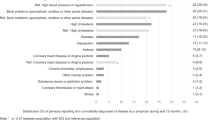
Association between morbidities and demographic characteristics
We found significant associations between morbidities and demographic characteristics. These associations and their significance are described in Table 5.
Discussion
The study was carried out by means of a questionnaire. The response rate was good considering there were no incentives offered. The majority of subjects in the study had a secondary school education. Lower educational status leads to individuals being engaged in unskilled or semiskilled high-risk activities. Safety regulations are often nonexistent or ignored by these individuals. These factors may have contributed to make these individuals more prone to sustain an injury to the spinal cord.
There were nonspecific responses to the questions pertaining to level of lesion and etiology. This could be owing to the simplistic nature of the questionnaire, which may not have been interpreted specifically by the subjects.
We found the following trend in the incidence of morbidities: pain was the leading cause followed by spasticity, pressure sores, postural hypotension, respiratory complications and fractures. All the complications were more common in the ‘<2 years and ‘>5 years post-injury’ groups. The reason for the prevalence of morbidities during the initial post-injury years could be owing to the fact that subjects were less likely to be mobile. The prevalence at 5 years post-injury was similar to the initial post-injury period. This could be attributed to aging as well as longer years of disability.
It was interesting to find the various associations between the demographics and morbidities and morbidities itself which may have implications for rehabilitation.
Pain
We found an increase in pain prevalence with increasing age. Previous studies have shown association of pain and age, with greater pain intensity being found to be associated with older age.11, 12, 13 But we did not evaluate pain intensity in our study, the subjects were asked to report its presence or absence and describe the area. The most common location for pain was back, which was similar to the study carried out by Turner et al14 in 2001.
Pain in the back and chest was seen in subjects of all the age groups, with increased incidence at 40-<50 years age group followed by 18-<25 years age group. Shoulder pain was more common in 50-<60 years age group, neck pain in 40-<50 years age group, and pain below the level of lesion in 30-<35 years, 40-<50 years and 50-<60 years age group. The incidence of pain being greater in older age groups, could be owing to the aging process and owing to the higher perception of pain. The decrease in plasticity of the central nervous system with age, as far as neurogenic pain is concerned, as well as overuse of supralesional joints leading to osteo–articular pains15 may be reasons for this finding. Psycho–social stresses16 may have been contributing factors as well.
Another important aspect in pain perception was noticed in relation to duration since injury. In the present study, pain in back was more common in 1-<7 months post-injury period. This can be owing to the fact that the subjects were in the acute phase of rehabilitation. Pain in the back and chest was more common in the <2 years post-injury group. Pain in the back in the early years may be attributed more to mechanical factors. Shoulder and upper limb pain was more common in the >2 years post-injury group, and especially in the 20-<25 years post-injury group. This could be attributed to long-term stresses associated with disability and ambulation using wheelchair or any walking aid. Education regarding these long-term stresses may be of help in the reduction of these morbidities. Ambulators experienced less pain compared to nonambulators, though the frequency of shoulder pain was more among the ambulators. This may be attributed to the long-term use of walking aids.
Frequent occurrence of pain was observed among the subjects who complained of spasticity. This is similar to the findings observed by Levi et al17 that more than 41% of subjects with excessive spasticity reporting pain.
These individuals were more likely to be wheelchair users or ambulant and the pain can be attributed to the stresses associated with wheelchair ambulation or walking with a walking aid.
Spasticity
Subjects with thoracic level of lesion, nonambulators and those subjects with respiratory complications complained of more spasticity. Reasons for this finding could be owing to spasticity of the thoracic cage, causing respiratory impairment, which in turn, may have led to their inability to ambulate. Contrarily, it may be that the higher the lesion, higher the dependency and the patients may have been forced to be less physically active leading to increased spasticity as well as pulmonary complications. The survey was not sensitive enough to pick up these cause and effect relationships. We acknowledge that this is a limitation of this study.
Pressure sore
Pressure sores were more common in individuals with thoracic level of lesion, nonambulators and those subjects with respiratory complications. This could be explained by the fact that these subjects were more immobile.
Another observation was related to ambulation. In the present study, 41% of the subjects were ambulators and we found an association of ambulation with pain, spasticity and pressure sores. Ambulators had less frequency of pressure sores and spasticity and experienced less pain compared to nonambulators. Thus, it can be hypothesized that ambulation reduces the frequency of secondary complications in individuals with paraplegia. In India, owing to social and health-care constraints ambulation is often deferred in favour of wheelchair. Thus, emphasis on ambulation as a primary goal in SCI rehabilitation may be of help in the reduction of these secondary complications.
Postural hypotension
We found an association between postural hypotension and level of lesion, with increase in the incidence of postural hypotension with higher level of lesion. This is as expected and well documented. Postural hypotension was also associated with the respiratory complications and spasticity. We hypothesize the reasons for this to be similar to those discussed under spasticity.
Respiratory
We did not find an association of respiratory impairment with ambulation and level of lesion. The reason for this is unclear, as respiratory impairment would have been expected to be more common in nonambulators and individuals with thoracic level of lesion. Possible causes may be underreporting or lack of comprehension of the questions.
Fracture
Fractures were more common in 1-<2 years, 5-<10 years, 20-<25 years, and more than 25 years post-injury period, that revealed that the rate of fracture increased with the increase in duration since injury. This is similar to the findings of Mckinley et al18 that as individual with SCI age, they experience an increased fracture rate, which may be the result of immobility related to years after injury. We agree with this theory especially as most individuals in our study were nonambulators.
Conclusion
The population most at risk for SCI were those in the working age groups who were engaged in unskilled work. The most common cause for morbidity in individuals with SCI was pain. Prevalence of pain was the greatest in the initial post-injury period. Ambulation reduced the incidence of many secondary complications.
Limitations of the study
The understandability of the questionnaire may have been a limitation as some answers were ambiguous. The questionnaire was constructed in a simple and short manner, keeping in mind the minimum education of the population targeted. So, it may have been too simplistic and may not have been sensitive enough.
The regional languages in India have a large number of dialects where word meanings often change. This may have contributed to nonspecific responses. These could have been overcome if interviews were conducted. However, this was beyond our scope considering the vast area surveyed.
Implication
To educate individuals of SCI in India regarding various causes of morbidities, their prevention and treatment measures. It becomes essential to have regular follow-up home care services in India. Ambulation as an exercise must be emphasized. The study, although, carried out in India, may have an import on other resource poor countries in Asia and Africa as well.
Future research
In future studies, it would be worthwhile to add more questions on initial management strategies, functional aspects, quality of life, and psychosocial aspects in the questionnaire. Questions should be constructed to glean information about cause and effects. Attempts to increase the sample size must be made. One of the possible ways to minimize patients being lost to follow-up may be to evaluate longitudinally at the same centres that the patients are followed up at – this would necessitate a multicentre study.
References
Awareness and Prevention. [http://www.isiconline.org/aware.htm.]
Chhabra HS . Life after SCI in India – Results of a survey of 53 centres. [http://www.iscos.org.uk/abstract13.html.]
Morton SC et al. Anti-microbial prophylaxis for urinary tract infection in persons with spinal cord dysfunction. Arch Phys Med Rehabil 2002; 83: 129–138.
Chen D, Apple DF, Hudson LM, Bode RK . Medical complications during acute rehabilitation following spinal cord injury – current experience of the model systems. Arch Phys Med Rehabil 1999; 80: 1397–1401.
Illman A, Stiller K, Williams M . The prevalence of orthostatic hypotension during physiotherapy treatment in patients with an acute spinal cord injury. Spinal Cord 2000; 38: 741–747.
Winslow C, Rozovsky J . Effect of spinal cord injury on the respiratory system. Am J Phys Med Rehabil 2003; 82: 803–814.
Skold C, Levi R, Seiger A . Spasticity after traumatic spinal cord injury: nature, severity, and location. Arch Phys Med Rehabil 1999; 80: 1548–1557.
Siddall PJ, Taylor DA, Cousins MJ . Classification of pain following spinal cord injury. Spinal Cord 1997; 35: 69–75.
Raina D . Osteoporosis in spinal injured–prevention and management. In: Proceedings of the 2nd International Spine and Spinal injuries Conference. New Delhi, India 2004 Mar 12–14, pp 115–117.
Devadasan N . Health financing protecting the poor. In: Proceedings of the IAPSM Conference. Chandigarh, India 2004 Mar.
Weitzenkamp DA, Jones RH, Whiteneck GG, Young DA . Ageing with spinal cord injury:cross-sectional and longitudinal effects. Spinal Cord 2001; 39: 301–309.
Rintala DH, Loubser PG, Castro J, Hart KA, Fuhrer MJ . Chronic pain in a community based sample of men with spinal cord injury: Prevalence, severity and relationship with impairment, disability, handicap and subjective well-being. Arch Phys Med Rehabil 1998; 79: 604–614.
Anke WAG, Stenehjem AE, Stanghelle KJ . Pain and life quality within 2 years of spinal cord injury. Paraplegia 1995; 33: 555–559.
Turner JA, Cardenas DD, Warms CA, McClellan CB . Chronic pain associated with spinal cord injuries: a community survey. Arch Phys Med Rehabil 2001; 82: 501–508.
Klotz R, Joseph PA, Ravaud JF, Wiart L, Barat M, The Tetrafigap Group. Tetrafigap survey on the long-term outcome of tetraplegic spinal cord injured persons: Part III. Medical complications and associated factors. Spinal Cord 2002; 40: 457–467.
Stormer S et al. Chronic pain/dysaesthesia in spinal cord injury patients:results of a multicentre study. Spinal Cord 1997; 35: 446–455.
Levi R, Hutling C, Nash MS, Seiger A . The Stockholm spinal cord injury study: 1. Medical problems in a regional SCI population. Paraplegia 1995; 33: 308–315.
McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ . Long term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil 1999; 80: 1402–1410.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gupta, N., Solomon, J. & Raja, K. Paraplegia: a postal survey of morbidity trends in India. Spinal Cord 45, 664–670 (2007). https://doi.org/10.1038/sj.sc.3102037
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102037
Keywords
This article is cited by
-
Lack of adequate care post spinal cord injury - a case report
Spinal Cord Series and Cases (2019)
-
Against all odds: a qualitative study of rehabilitation of persons with spinal cord injury in Afghanistan
Spinal Cord (2012)
-
Paraplegia pangs
Nature India (2007)