Abstract
Study Design:
Secure, web-based survey.
Objectives:
Obtain information from the spinal cord injured (SCI) population regarding sexual dysfunctions, with the aim of developing new basic science and clinical research and eventual therapies targeting these issues.
Setting:
Worldwide web.
Methods:
Individuals 18 years or older living with SCI. Participants obtained a pass-code to enter a secure website and answered survey questions. A total of 286 subjects completed the survey.
Results:
The majority of participants stated that their SCI altered their sexual sense of self and that improving their sexual function would improve their quality of life (QoL). The primary reason for pursuing sexual activity was for intimacy need, not fertility. Bladder and bowel concerns during sexual activity were not strong enough to deter the majority of the population from engaging in sexual activity. However, in the subset of individuals concerned about bladder and/or bowel incontinence during sexual activity, this was a highly significant issue. In addition, the occurrence of autonomic dysreflexia (AD) during typical bladder or bowel care was a significant variable predicting the occurrence and distress of AD during sexual activity.
Conclusion:
Sexual function and its resultant impact on QoL is a major issue to an overwhelming majority of people living with SCI. This certainly constitutes the need for expanding research in multiple aspects to develop future therapeutic interventions for sexual health and SCI.
Sponsorship:
Christopher Reeve Foundation (#36708, KDA); Reeve-Irvine Research Center.
Similar content being viewed by others
Introduction
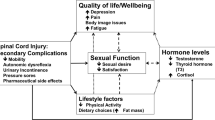
Spinal cord injury (SCI) causes many deficits that often restrict the lives of the individuals as well as their contributions to society. The worldwide impact is dramatic.1 The many impairments resulting from the neurologic damage not only limit physical function, but also influence an individuals' psychological well-being, social integration, financial status, and life aspirations, to varying degrees.2, 3 Extensive research has focused on recovery of motor function, both in animals and in humans.4, 5, 6, 7 Although ‘curing’ all functional deficits associated with SCI is the ultimate end goal of our research, such an endeavor involves much more than repairing, protecting, or regenerating motor tracts – the traditional focus of most SCI-related research. The autonomic nervous system and the sensory systems are equally important, yet relatively understudied. Thus, research efforts should equally reflect autonomic, sensory, and motor contributions to SCI. In addition, it is probable that discoveries leading to incremental improvements in specific functions will occur well before a single, all encompassing ‘cure’. An incremental improvement in neurologic function could translate into a significant improvement in the quality of life (QoL) of a person living with SCI. Therefore, we contend that SCI research emphasis should be broadened to develop therapies that contribute directly to QoL.
The SCI community understands and indeed embraces the idea of incremental functional recovery.8 They have also indicated that walking is not the most important function to recover in order to improve QoL. Regaining bladder and bowel function, eliminating autonomic dysreflexia (AD), and improving arm/hand function are among the top priorities of individuals with SCI,8 all of which require more extensive research at the basic science and clinical level. And, driving the focus of the current study, regaining sexual function is the combined number one or number two priority to a significant proportion of all individuals living with SCI, regardless of injury level.8
The anatomy and physiology of SCI-induced sexual deficits are fairly well understood.9, 10 Certain aspects of SCI-associated sexual impairments have been studied extensively, such as male fertility.11 However, fertility and reproduction should not be the only reason for studying sexual problems resulting from SCI. Past attitudes that people with SCI should be ‘happy to be alive’ and should ‘learn to live without sexual pleasure’ are outdated. Throughout the last decade, a variety of studies have clarified the association of sexual function after SCI with QoL.12, 13, 14, 15, 16 Recognizing how important sexual function remains to individuals living with SCI, it is clear that targeting various research efforts in this area could result in incremental improvements. In this study, we sought to identify more specific details about sexual issues that are important to both men and women in the general SCI community and relate them to contributing physiological factors. More extensive investigations of male-specific and female-specific aspects of sexual function (which are subparts of the survey presented here) are presented in the accompanying articles.17, 18
Methods
Survey design
A questionnaire covering a wide variety of sexual components was developed to acquire more detailed information related to sexual function and SCI. This questionnaire was not designed to be used as a sexual function outcome measure. Rather, it was designed to query the general SCI population beyond those individuals that actively seek out laboratory research studies or fertility clinics.
The questionnaire was divided into three sections. The first section was answered by both males and females (35 questions) and those results are presented in this manuscript. It contained questions addressing general demographic information, injury characteristics, bladder and bowel management, AD, secondary conditions, medications, and sexual activity. The second section was answered only by males (26 questions). It contained specific questions regarding arousal, erection, ejaculation, and orgasm. The third section was completed by females only (39 questions). This section contained questions about arousal, orgasm, intercourse, and birth control/fertility. Owing to the large volume of data generated by the survey, the results from the male- and female-specific questions are presented in adjoining manuscripts.17, 18
Wherever possible, lists of answers were provided for each question (eg yes/no/sometimes, Likert-style scales, and check boxes for multiple choice questions with the option of filling in unlisted choices). This was performed to assist in standardization of responses. Few questions required descriptive answers from the subjects. For example, subjects were asked to list their secondary medical conditions. They could choose any or all of the following: AD, continuous chronic pain, constant spasticity, current pressure sore(s), depression, diabetes, hypertension, hypotension, syringomyelia, other, or none. Under current medications used, subjects could choose from the following categories: bladder, cholesterol/lipid, heart/blood pressure, pain, recreational drugs (alcohol, marijuana, other), spasticity, other, or none. Under physical conditions occurring during sexual activity, subjects could choose all that applied from the following list: headache, pain, shortness of breath, spasm, tingling sensations, other, or none, Subjects could choose one of the following for their primary reason for pursuing sexual activity: fertility, intimacy need, self-esteem, sexual need, to keep my partner, or other.
The study was approved by the University of California Irvine Institutional Review Board. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. Attached to the survey was an introductory statement explaining the purpose of the survey, directions for participating, the right to privacy, what the results were to be used for, and that three of the five investigators conducting the survey also had spinal cord injuries. This information served as the informed consent statement, as required by the Institutional Review Board.
Participant recruitment
The eligibility requirements for the survey were simply that an individual be 18 years of age or older and be living with a permanent SCI. Advertisements were placed on multiple SCI websites, online support groups, SCI bulletin boards, etc. (including the National Spinal Cord Injury Association, Project Walk, Reeve-Irvine Research Center, NeuroFitness Foundation, SCI Zone, 360mag, Paralysis Resource Center, MobileWomen, Paralysis Project of America, United Spinal/Orbit magazine, Florida SCI Resource Center, Miami Project E-News, and Canadian Paraplegic Association). Print advertisements were also placed in Paraplegia News, New Mobility, and the California Paralyzed Veterans Association monthly newsletter.
Eligible subjects who were willing to participate received a randomly generated pass code in order to enter the secure website. Upon completion of the survey, the pass code used by an individual to enter the website was not linked to his/her answers, thereby preserving anonymity. Individuals interested in participating whom did not have access to the Internet could receive a paper version of the questionnaire in the mail and then send it back to the lead investigator, who then entered the information into the secure database. The study was open for enrollment for a 6-month time period.
Statistical analyses
Statistical assessments were performed using the JMP 6.0.0 Statistical Discovery™ software package from SAS, with guidance from the UCI Center for Statistical Consulting. Descriptive analyses of the data were performed first. After which, a series of bivariate analyses were performed to determine whether any of the following variables (X) influenced any of the following responses (Y):
X factor
-
1
Current age group (under 30, 30–50, over 50)
-
2
Years postinjury group (0–5, 6–10, >10)
-
3
Gender (m/f)
-
4
Injury group (cervical, upper thoracic, lower thoracic, lumbosacral)
-
5
Can you feel touch in the anal area? (yes/no)
-
6
Can you lift your legs against gravity? (yes/no)
-
7
Number of medical conditions (0, 1, 2, 3 or more)
-
8
Reported pain (yes/no)
-
9
Reported depression (yes/no)
-
10
Reported spasticity (yes/no)
-
11
Number of medication types using (0, 1, 2 or more)
-
12
Using pain medication (yes/no)
-
13
Using bladder medication (yes/no)
-
14
Current bladder management (controlled voiding, manual crede or spontaneous voiding, indwelling catheter, intermittent catheterization, condom catheter, suprapubic catheter, other)
-
15
Current bowel management (voluntary control, digital stimulation alone, enema +/− digital stimulation, suppository +/− digital stimulation, other)
-
16
Do you experience AD during bladder care? (yes/no/sometimes)
-
17
Do you experience AD during bowel care? (yes/no/sometimes)
-
18
Do you have any genital sensation? (yes/no)
-
19
Were you ever involved in any type of sexual relationship preinjury? (yes/no)
Y response
-
1
Are you concerned about bladder incontinence during sexual activity? (not concerned, undecided, concerned)
-
2
Are you concerned about bowel incontinence during sexual activity? (not concerned, undecided, concerned)
-
3
Do bladder and bowel issues prevent you from seeking sexual activity with partners? (yes/no/sometimes)
-
4
Have you ever been involved in any type of sexual relationship postinjury? (yes/no)
-
5
Are you currently involved in any type of sexual relationship? (yes/no)
-
6
Do you experience AD during any type of sexual activity (alone or with a partner)? (yes/no)
-
7
How much does AD interfere with your sexual activity? (none/some)
-
8
Do you experience the symptoms of AD as pleasurable/arousing? (yes/no/not applicable)
-
9
Number of physical conditions experienced during sexual activity (0, 1, 2 or more)
-
10
Tingling sensations during sexual activity (yes/no)
-
11
Spasms during sexual activity (yes/no)
-
12
What is the primary reason you are interested in pursuing sexual activity? (sexual need, intimacy need, self-esteem, fertility, to keep my partner, other)
-
13
Do you agree that you injury has altered you sexual sense of self? (disagree, undecided, agree)
-
14
Is improving your sexual function important to improving your QoL? (yes/no)
The resulting contingency tables were reviewed and factors accounting for <5% of the variability of responses (r2<0.05) were discarded. Factors accounting for >5% of the variability of responses are reported in the text along with the r2 value. In addition, χ2 analyses were performed for those factors and the P-values are reported in the text.
Results
Demographics
There were a total of 286 participants, of which 199 were males (69.6%) and 87 were females (30.4%). The mean age at time of injury was 27.7±12.7 years. The mean current age at time of study participation was 42.2±11.1 years. There were 11.9% of the participants between ages 18 and 29, 64.7% between ages 30 and 50, and 23.4% over 50 years old. The mean number of years postinjury was 14.5±11.8 years. There were 28.7% of the subjects that were 0–5 years postinjury (0 year accounting for those individuals who were less than 1 year postinjury), 17.1% who were 6–10 years postinjury, and 54.2% who were more than 10 years postinjury. Approximately 47.2% of all subjects had a cervical SCI, 45.8% had a thoracic lesion, and 7% had injuries in the lumbosacral area. The same cause of injury classification groupings used by the Model SCI Systems (National SCI Statistical Center, Birmingham, Alabama) was used in this study (vehicular, fall, violence, sports, other). The most common cause of injury was related to vehicular incidents (48.6%), followed by sports (15.7%), falls (12.9%), violence (4.5%), and other miscellaneous events (18.2%).
With regard to completeness of injury, 50.7% of participants reported being able to feel touch below the level of lesion, but only 41.3% could feel touch in the anal area. This indicated that more than half of the subjects (58.7%) had self-described ‘complete’ SCIs (ASIA grade A). Only 29.4% of all subjects could tell the difference between sharp and dull sensation below their level of lesion, 22.7% could voluntarily tighten the anal sphincter, and 9.4% could walk without assistance (people or equipment).
Secondary conditions and medications
There were multiple medical conditions that subjects reported experiencing in conjunction with their SCI (some subjects reported multiple conditions). Figure 1 illustrates that the two most common secondary conditions were chronic pain (32.9%) and spasticity severe enough to require medication (28.7%). Other common problems were depression (23.1%), AD (22%), hypotension (12.6%), hypertension (9.4%), and current skin sores (10.1%). Less commonly cited conditions were syringomyelia (4.5%) and diabetes (3.8%), however, these two conditions often go undiagnosed until serious symptoms begin to appear.
The most common medications used by participants were for bladder maintenance (49%) and pain management (34.6%). Figure 2 also shows that spasticity medications (23.4%) and recreational drugs (22%) were frequently used by subjects, followed to a lesser extent by cardiovascular (10.1%) and cholesterol/lipid medications (7.3%). A combination of various ‘other’ prescription and over-the-counter drugs were reported by 28.7% of subjects. Only 16.1% of the participants reported not using any type of medication. More than half of the subjects (52.1%) reported using two or more categories of drugs and only 31.8% used a single category of medication.
Bladder and bowel management
Several questions were asked regarding bladder and bowel management as these could potentially influence sexual activity. The primary method of bladder management was intermittent catheterization (46.5%), followed by suprapubic catheters (12.2%), condom catheters (10.8%), indwelling catheters (8.4%), controlled voiding (8%), and manual crede or spontaneous voiding (9.4%). The majority of people reported experiencing zero (46.5%) or 1 to 5 (32.5%) bladder accidents per month, with only 8.7% reporting 6–10 accidents and 12.2% reporting >10 accidents each month. There were 59.1% of subjects who reported having 1–5 urinary tract infections per year that required medication. The two primary methods of bowel management were by digital stimulation alone (36.1%) or using a suppository with or without digital stimulation (35.3%). This was followed by voluntary control (12.6%), using an enema with or without digital stimulation (8%), or by other means (8%).
General sexual activity
Background information regarding sexual activity was obtained for all subjects. The overwhelming majority (89.9%) had been involved in some type of sexual relationship preinjury. Additionally, the majority (87.4%) had been involved in some type of sexual relationship postinjury. Not surprisingly, involvement in a sexual relationship postinjury was slightly influenced by years postinjury (r2=0.06 (r=0.24); χ2=12.06, P=0.0024), in that the greater the number of years postinjury the greater the likelihood of a subject having been in a sexual relationship. However, although still a majority, fewer subjects reported current involvement in a sexual relationship (59.4%). Importantly, 82.9% of subjects stated that improving sexual function was important to improving their QoL. When asked about whether their SCI had altered their sexual sense of self (defined as each participant's own perception of his/her self), 83.2% of individuals agreed with that statement, while only 12.6% disagreed, and 4.2% were undecided. The responses to the above two questions regarding QoL and sexual sense of self were independent of all the X factors listed in the statistical analyses portion of the methods section.
When asked what the primary reason for pursuing sexual activity was, more than half of the people (57.7%) listed intimacy need (Figure 3). This was followed by sexual need (18.9%), self-esteem (9.8%), and to keep a partner (8.4%). Fertility was the least commonly reported reason for pursuing sexual activity (1%). We further asked whether subjects experienced certain physical conditions while engaged in sexual activity. Figure 4 illustrates that tingling sensations (35.3%) and spasms (35%) were the most commonly reported, followed to a much lesser extent by pain (10.8%), headache (8.7%), shortness of breath (8.7%), and ‘other’ (8%). Many participants, however, chose ‘none’ (38.8%) in response to this question. There were 29.4% who reported only experiencing one of the conditions, while 31.8% reported experiencing two or more conditions during sexual activity. Here too, the responses reported above were independent of all the X factors listed in the statistical analyses portion of the methods section.
Bladder and bowel concerns during sexual activity
The impaired or lost ability to control the bladder and bowel after SCI automatically puts individuals at risk of having bladder and/or bowel incontinence during typical daily activities.9, 19 Depending upon the person, sexual activity may increase the risk of experiencing incontinent episodes (during or after sexual activity) and, thus, may influence that person's willingness to engage in sexual activity. In an effort to obtain generalizable information for the SCI population as a whole, we queried multiple aspects of this topic. First, 46.9% of the subjects reported having some type of genital sensation while 53.1% did not have any genital sensation. However, the presence or absence of genital sensation had no significant influence on the responses to any questions regarding bladder or bowel concerns (or any of the other Y responses listed in the statistical analyses portion of the methods section).
Second, 64.7% of all participants stated that bladder/bowel issues did not prevent them from seeking sexual activity with a partner, although 19.6% reported that sometimes these issues did interfere, and 15.7% reported yes to these issues preventing them from seeking sexual activity. Of those 15.7% of individuals stating that bladder/bowel issues did in fact prevent them from seeking sexual activity with a partner, 37.8% were females and 62.2% were males. Of those females, 100% were concerned about bladder incontinence during sexual activity and 70.6% were concerned about bowel incontinence during sexual activity. Of those males, 71.4% were concerned about bladder incontinence during sexual activity and only 35.7% were concerned about bowel incontinence during sexual activity. When analyzing the entire study population, however, the majority of subjects were not concerned about bladder (61.5%) or bowel (71.7%) incontinence during sexual activity (Figure 5). Hence, bladder or bowel issues may not prevent the majority of the study population from seeking sexual activity, but for those individuals concerned about experiencing bladder or bowel incontinence during sexual activity this is a significant deterrent from pursuing sexual engagements.
Third, concern about bladder incidents during sexual activity was correlated with current bladder management methods (r2=0.09 (r=0.30); χ2=35.47, P=0.0004). Approximately 52% of subjects who used manual crede/spontaneous voiding, 55% who used condom catheters, 37% who used intermittent catheterization, 33% who used indwelling catheters, and 14% who used suprapubic catheters were concerned, to some extent, about bladder incontinence during sexual activity. In contrast, only one of the 22 subjects who could perform controlled voiding was concerned about bladder incontinence during sexual activity.
Finally, whether or not bladder and bowel issues prevented participants from seeking sexual activity (either alone or with a partner) was influenced by current bladder management techniques (r2=0.06 (r=0.24); χ2=26.71, P=0.0085), but not bowel management. The most significant deterrent here was the use of manual crede/spontaneous voiding or condom catheters in which 54% (combined) of these subjects stated that bladder and bowel issues prevented them from seeking sexual activity. Of those that used intermittent catheterization, suprapubic catheters, or indwelling catheters, a combined 43% reported letting those concerns prevent them from seeking sexual activity. In contrast, only one of the 22 subjects who reported using controlled voiding for bladder management reported that sometimes those concerns interfered with seeking sexual activity.
AD during sexual activity
To assess AD during sexual activity, we began by asking about the occurrence of AD during bladder and bowel care. Figure 6 demonstrates that 10.8 and 30.1% of the study population reported experiencing some level of AD (answered ‘yes’ or ‘sometimes’, respectively) during bladder care. To a lesser extent, only seven and 22.7% reported experiencing AD during bowel care.
The occurrence of AD during sexual activity was more complex. On the simplest level, 31.8% of the participants reported experiencing AD during sexual activity (alone or with a partner). However, this was significantly influenced by injury level, current bladder management routine, and the occurrence of AD during bladder or bowel care. Not unexpectedly, more people with cervical injuries reported experiencing AD during sexual activity (48.9%; r2=0.11 (r=0.33); χ2=37.67, P<0.0001). People using indwelling catheters, suprapubic catheters, or manual crede/spontaneous voiding were the greatest percentage, in comparison to the other bladder management routines, to report experiencing AD during sexual activity (54, 57, 52%, respectively; r2=0.09 (r=0.30); χ2=33.35, P<0.0001). Additionally, the likelihood of experiencing AD during any type of sexual activity was positively correlated with the occurrence of AD during bladder care (r2=0.16 (r=0.40); χ2=56.47, P<0.0001) and/or bowel care (r2=0.14 (r=0.37); χ2=50.36, P<0.0001).
Similar patterns and correlations were revealed for how much AD was stated, in this study, to interfere with sexual activity. Individuals with cervical injuries were more likely to report that AD interfered with their sexual activity (r2=0.07 (r=0.26); χ2=19.36, P=0.0002). Also, people using indwelling catheters, suprapubic catheters, or manual crede/spontaneous voiding were the greatest to report the interference of AD during sexual activity (33, 34, 37%, respectively; r2=0.07 (r=0.26); χ2=19.50, P=0.0034). Whether or not people reported that their AD was significant enough to interfere with their sexual activity was significantly correlated with their experiencing AD during bladder care (r2=0.14 (r=0.37); χ2=40.28, P<0.0001) and/or bowel care (r2=0.14 (r=0.37); χ2=42.25, P<0.0001).
Knowing that autonomic stimulation is a natural part of sexual activity, it is possible that some people may consider the symptoms of AD during sexual activity as pleasurable or arousing. In this study, however, only 6.3% of all the participants reported that indeed this was true for them (see Conclusions). However, whether or not people experienced the symptoms of AD during sexual activity as pleasurable/arousing was associated with whether or not they experienced AD during bladder (r2=0.05 (r=0.22); χ2=26.37, P<0.0001) or bowel care (r2=0.07 (r=0.26); χ2=39.30, P<0.0001).
Conclusions
The general demographics of participants in the current study were similar to those reported in the National Spinal Cord Injury Database.20 The data from this survey revealed that the vast majority of participants (more than 80%) stated that their SCI altered their sexual sense of self and that improving their sexual function would improve their QoL. Overwhelmingly, the primary reason for pursuing sexual activity was for intimacy need, not fertility. The most common physical conditions experienced during sexual activity were tingling sensations and spasms. Bladder and bowel concerns during sexual activity were not strong enough to deter the majority of the population from engaging in sexual acts. However, in the subset of individuals concerned about bladder and/or bowel incontinence during sexual activity, this was a significant issue. In addition, the occurrence of AD during typical bladder or bowel care was a significant variable predicting the occurrence of AD during sexual activity.
Caveats of the study population
As with any survey, or any kind of study involving humans, only those individuals that are interested will volunteer to participate. Thus, there is the possibility that the data obtained from the study participants may not be a representative sample of the entire population with the disease of interest. Regardless, important information can still be gained from such surveys.
Using a web-based survey as a mode of data collection is a recent innovation that offers many advantages in accessing potential research subjects. In regard to SCI, individuals who may be interested in participating in a research study at a clinical site may not be able to secure transportation to/from the location or, if they are employed, may not be able to afford the lost wages associated with time away from work, thus precluding them from participating even though they may meet specified inclusion criteria. Additionally, some individuals may not be motivated to participate in a study that is time consuming, demanding, or disruptive of their daily routine. Hence, there are some situations where extensive information can be obtained by simply taking the research to the subjects. One method of doing that is via the Internet, as was carried out here. The Internet has become the most prominent means of gathering resource information and has removed multiple barriers for many people with SCI, worldwide, who in the past may have had limited access to information and who may have experienced social isolation, among other things. Obviously caution must be taken as there are both good and bad things about the Internet, which is why the security measures described in the methods section were employed in this study. However, previous studies show that people with SCI prefer to receive research information over the Internet21 and important scientific information can be gained from Internet-based research surveys.8 In an effort to not exclude individuals who did not have access to the Internet, we placed recruitment advertisements in multiple disability magazines providing the option of completing the survey via the postal mail.
The mean age at the time of study participation was 42 years old (64% of subjects were between ages 30 and 50), with an average of 15 years postinjury. It is possible that the predominance of people in that age group and length of time postinjury electing to participate in the study was because they had multiple years to adjust to their SCI and with increasing age were more willing to address their sexual function. However, across the three age groups (18–29, 30–50, and over 50) and across the three groups of time postinjury (0–5, 6–10, and >10 years) their was no difference in the primary reason for pursuing sexual activity, in feeling that their SCI had altered their sexual sense of self, or that improving sexual function would improve their QoL.
Finally, the authors do not know how many people saw advertisements for the survey and decided not to participate. There is the possibility that some individuals who had not engaged in sexual activity postinjury decided not to participate because they may have felt they had nothing to contribute. Additionally, some individuals may have been too embarrassed to answer questions about their sexual activity, despite the anonymity built into the survey. Religious beliefs and cultural customs may also have deterred some people from participating. Furthermore, answering survey questions may remind some people of the multitude of tests they are inundated with during rehabilitation and/or doctor's visits, thus deterring them from participating. Or, some people may want to simply ‘move on with their lives’ and not answer research questions. However, because the demographic characteristics of the study population were very similar to those reported in the National SCI Database and a large number of subjects participated (n=286), the authors are confident that meaningful data have been obtained.
Improving sexual function is important, irrespective of multiple factors
The finding that more than 80% of participants stated that their SCI had altered their sexual sense of self and that improving sexual function would improve their QoL demonstrates how critically important this topic is and that this area of research needs to be greatly expanded. These responses did not co-vary with gender, injury level or severity, age, years postinjury, secondary conditions, medications, bladder or bowel management, experiencing AD during bladder or bowel care, absence or presence of genital sensation, or participation in any type of sexual relationship preinjury. The single fact of having an SCI and its' subsequent impact on sexual function was enough to significantly lower perceived QoL. Thus, addressing sexual function in research and possibly making incremental gains in functional recovery would benefit the entire population of individuals living with SCI.
The primary reason stated for pursuing sexual activity was for intimacy need (57.7%), which was followed to a lesser extent by sexual need (18.9%), self-esteem (9.8%), to keep a partner (8.4%), and ‘other’ various reasons (4.2%). One question not fully answered in regard to intimacy need is whether respondents were seeking to give to others through the interaction, receive intimate contact from others, or both. Fertility, however, was the least commonly reported reason for pursuing sexual activity (1%). Here too, the responses were independent of all the factors listed above. This latter finding is not surprising, actually, if one were to considered how life altering it is to experience a spinal injury. Everything changes. The physiologic impairments induced by spinal paralysis influence every other aspect of life. It is human nature to seek comfort and intimacy, especially in difficult situations. There are some reports of decreased frequency of sexual activity due to decreased desire in individuals with SCI.22, 23, 24, 25 However, one must take into account the strong likelihood of people with SCI experiencing decreased opportunities to engage in sexual activity, increased frustration levels (both with biologic dysfunctions and social attitudes), altered body image, and variable psychological mindsets. These are just a few among many potential factors that could impact the frequency of engaging in sexual activity. The results presented here indicate that, despite all of those possible problems, sexual function is extremely important to people living with SCI and they have a high desire for intimacy.
It should also be noted that in the US, Canada, and several countries in western Europe adequate governmental dollars have been invested in the care aspects of SCI such that most people who have an SCI and live in those countries will have multiple options for mobility and independence, are likely to have any fertility issues addressed, and have access to improved methods of bladder and bowel care. Moreover, significant research dollars have been poured into improving medical care and developing regenerative ‘cure’ strategies over the past three decades. However, relatively few options and even fewer research dollars have been directed towards improving other QoL issues, especially in regards to nonreproductive issues such as sexual intimacy and pleasure. The current reality that people with SCI face is the fact that they are living longer lives, but that there are not yet available therapeutic treatments that will induce regeneration in their chronically injured spinal cord. Hence, improving QoL, by enhancing a variety of functions, is a necessity and research funding should target the priorities of the population being studied.
AD – a broad avenue for basic science research
Autonomic dysregulation is associated with physical impairments of sexual function in individuals with SCI. Of course, bladder and bowel function is significantly impacted by loss of central nervous system (CNS) control of the autonomic nervous system (ANS) and AD can develop in individuals with spinal injuries at or above thoracic level six. Until recently, research regarding autonomic dysregulation did not receive much recognition, despite the life-threatening potential ever-present during each AD episode an individual experiences. However, Weaver and Polosa recently published a comprehensive, research-based collection of autonomic dysfunctions that occur after SCI,26 including anatomical changes, and bladder, bowel, cardiovascular, and sexual dysfunctions.
The finding that the presence of AD during typical bladder or bowel care positively correlates with the occurrence of AD during sexual activity is expected, because the pelvic organs share many autonomic tracts,26 but still important. There was a 2:1 ratio of people who experienced AD during bladder care who also reported experiencing AD during sexual activity and a 3:1 ratio for people who experienced AD during bowel care. One caveat to these findings is that it is possible that those individuals who reported experiencing AD during bladder or bowel care as well as during sexual activity may have more severe AD episodes and, thus, are more likely to report experiencing AD. Alternatively, those individuals may be more in tune with their bodies in regard to recognizing the subtle symptoms of AD and, thus, more likely to report experiencing AD during different situations. We also do not know the prevalence of ‘silent’ AD. This is a condition where, in certain individual's, the blood pressure increases in response to AD-inducing stimuli, but without the occurrence of outwardly recognizable AD symptoms. This is commonly found in response to bladder or bowel stimuli,27, 28, 29, 30 but has also been shown to occur in response to sexual stimulation.31
Nonetheless, this finding supports expanding the field of basic science animal research regarding SCI-induced AD. It has recently been demonstrated in animals that the development and severity of AD can be significantly attenuated by administering neuroprotective strategies acutely after spinal injury.32, 33 Additionally, it is known that sprouting of primary afferent fibers after SCI is part of the mechanism underlying the development of AD in rodents34, 35, 36, 37, 38 and that administering anti-nerve growth factor (NGF) intraspinally can block AD.39 Very recently, it was further demonstrated that adenoviral-overexpression of NGF (growth-promoting) or semaphorin 3A (Sema3a, growth-inhibiting), intraspinally, increased or decreased the postinjury sprouting of primary afferent fibers caudal to the lesion, respectively.40 Furthermore, there was a direct correlation between the extent of fiber sprouting and the severity of AD. This knowledge warrants extensive investigation into developing therapeutic treatments targeted toward ameliorating AD, either acutely or chronically.
Reducing or eliminating the development of AD in humans with injuries at or above thoracic level six, which constitute more than 50% of the SCI population, could have a wide reaching effect on improving QoL. Not only could bladder or bowel induced AD be ameliorated, but also AD that occurs during sexual activity and in response to other stimuli. The animal models for testing AD already exist, thus may provide the potential for developing treatments that could influence sexual function without the inherent difficulties of assessing sexual behaviors in animals with SCI.
A counter argument to developing treatments that could eliminate AD may be that some individuals reported that they interpreted the AD symptoms they experienced during sexual activity as pleasurable or arousing. It is possible that these individuals have learned to associate their AD symptoms, which some individuals would interpret as painful or uncomfortable, with those of sexual satisfaction. Some level of aberrant autonomic stimulation may in fact be beneficial during sexual activity following SCI. However, if therapeutic treatments can be developed that reduce the development of severe AD symptoms without completely eliminating AD, a balance may be achieved allowing people to take advantage of mild AD that may be useful in a variety of situations, yet avoid life threatening AD situations. A more detailed analysis and discussion of AD in humans in regard to male-specific and female-specific sexual function is presented in the accompanying manuscripts.17, 18
Overall, however, one must consider the positive and negative aspects of AD in both the acute episode situation and when chronically exposed to repeated episodes. Does the potential for harm outweigh the potential for good? Advances in medicine have led to a near normal lifespan for people living with SCI, which is resulting in an expanding aged population. Thus, maintaining health and independence in people aging with a spinal injury is increasingly important.41 What are the risks associated with experiencing repeated AD episodes for 20, 30, or 40 (or more) years?
Summary
The findings presented here indicate that improving sexual function remains a priority for people living with SCI and that the current means of enhancing sexual ability are still deemed unsatisfactory in regard to improving QoL. Expanding both basic science and clinical research regarding autonomic dysregulation is not only warranted, but imperative for the future development of therapeutic treatments that can significantly impact the QoL of the worldwide SCI population.
References
Ackery A, Tator C, Krassioukov A . A global perspective on spinal cord injury epidemiology. J Neurotrauma 2004; 21: 1355–1370.
Stiens SA, Bergman SB, Formal CS . Spinal cord injury rehabilitation. 4. Individual experience, personal adaptation, and social perspectives. Arch Phys Med Rehabil 1997; 78: S65–S72.
Stiens SA, Kirshblum SC, Groah SL, McKinley WO, Gittler MS . Spinal cord injury medicine. 4. Optimal participation in life after spinal cord injury: physical, psychosocial, and economic reintegration into the environment. Arch Phys Med Rehabil 2002; 83: S72–S81.
Edgerton VE, Roy RR . Paralysis recovery in humans and model systems. Curr Opin Neurobiol 2002; 12: 658–667.
Batchelor PE, Howells DW . CNS regeneration: clinical possibility or basic science fantasy? J Clin Neurosci 2003; 10: 523–534.
Fouad K, Pearson K . Restoring walking after spinal cord injury. Prog Neurobiol 2004; 73: 107–126.
Ramer LM, Ramer MS, Steeves JD . Setting the stage for functional repair of spinal cord injuries: a cast of thousands. Spinal Cord 2005; 43: 134–161.
Anderson KD . Targeting recovery: priorities of the spinal cord injured population. J Neurotrauma 2004; 21: 1371–1383.
Burns AS, Rivas DA, Ditunno JD . The management of neurogenic bladder and sexual dysfunction after spinal cord injury. Spine 2001; 26: S129–S136.
Benevento BT, Sipski ML . Neurogenic bladder, neurogenic bowel, and sexual dysfunction in people with spinal cord injury. Phy Ther 2002; 82: 601–612.
DeForge D et al. Fertility following spinal cord injury: a systematic review. Spinal Cord 2005; 43: 693–703.
Kreuter M, Sullivan M, Siösteen A . Sexual adjustment and quality of relationships in spinal paraplegia: a controlled study. Arch Phys Med Rehabil 1996; 77: 541–548.
Kreuter M, Sullivan M, Dahllöf AG, Siösteen A . Partner relationships, functioning, mood and global quality of life in persons with spinal cord injury and traumatic brain injury. Spinal Cord 1998; 36: 252–261.
Ide M, Fugl-Meyer AR . Life satisfaction in persons with spinal cord injury: a comparative investigation between Sweden and Japan. Spinal Cord 2001; 39: 387–393.
Fisher TL, Laud PW, Byfield MG, Brown TT, Hayat MJ, Fiedler IG . Sexual health after spinal cord injury: a longitudinal study. Arch Phys Med Rehabil 2002; 83: 1043–1051.
Reitz A, Tobe V, Knapp PA, Schurch B . Impact of spinal cord injury on sexual health and quality of life. Int J Impot Res 2004; 16: 167–174.
Anderson KD, Borisoff JF, Johnson RD, Stiens SA, Elliott SL . Long-term effects of spinal cord injury on sexual function in men: Implications for neuroplasticity. Spinal Cord 2007; 45: 338–348 (this issue).
Anderson KD, Borisoff JF, Johnson RD, Stiens SA, Elliott SL . Spinal cord injury influences psychogenic as well as physical components of female sexual ability. Spinal Cord 2007; 45: 349–359 (this issue).
Stiens SA, Bergman SB, Goetz LL . Neurogenic bowel dysfunction after spinal cord injury: clinical evaluation and rehabilitative management. Arch Phys Med Rehabil 1997; 78: S86–S102.
National Spinal Cord Injury Statistical Center. Annual Report for the Model Spinal Cord Injury Care Systems. University of Alabama: Birmingham, AL 2005.
Edwards L, Krassioukov A, Fehlings M . Importance of access to research information among individuals with spinal cord injury: results of an evidence-based questionnaire. Spinal Cord 2002; 40: 529–535.
Phelps G et al. Sexual experience and plasma testosterone levels in male veterans after spinal cord injury. Arch Phys Med Rehabil 1983; 64: 47–52.
Charlifue SW, Gerhart KA, Menter RR, Whiteneck GG, Manley MS . Sexual issues of women with spinal cord injuries. Paraplegia 1992; 30: 192–199.
Alexander CJ, Sipski ML, Findley TW . Sexual activities, desire, and satisfaction in males pre- and post-spinal cord injury. Arch Sex Behav 1993; 22: 217–228.
Sipski ML, Alexander CJ . Sexual activities, response and satisfaction in women pre- and post-spinal cord injury. Arch Phys Med Rehabil 1993; 74: 1025–1029.
Weaver LC, Polosa C (eds) Autonomic dysfunction after spinal cord injury. Prog Brain Res. Elsevier: Amsterdam 2006; 152: 1–453.
Giannantoni A et al. Autonomic dysreflexia during urodynamics. Spinal Cord 1998; 36: 756–760.
Linsenmeyer TA, Campagnolo DI, Chou IH . Silent autonomic dysreflexia during voiding in men with spinal cord injuries. J Urol 1996; 155: 519–522.
Curt A, Nitsche B, Rodic B, Schurch B, Dietz V . Assessment of autonomic dysreflexia in patients with spinal cord injury. J Neurol Neurosurg Psychiatry 1997; 62: 473–477.
Kirshblum SC, House JG, O'Connor KC . Silent autonomic dysreflexia during a routine bowel program in persons with traumatic spinal cord injury: a preliminary study. Arch Phys Med Rehabil 2002; 83: 1774–1776.
Elliott SL, McBride K, Ekland M, Krassioukov A . Characteristics of autonomic dysreflexia in men with SCI undergoing 296 procedures of vibrostimulation for sperm retrieval. J Spinal Cord Med 2005; 28: abstract #52, ASIA 31st Annual Meeting.
Gris D et al. Transient blockade of the CD11d/CD18 integrin reduces secondary damage after spinal cord injury, improving sensory, autonomic, and motor function. J Neurosci 2004; 24: 4043–4051.
Gris D, Marsh DR, Dekaban GA, Weaver LC . Comparison of effects of methylprednisolone and anti-CD11d antibody treatments on autonomic dysreflexia after spinal cord injury. Exp Neurol 2005; 194: 541–549.
Wong ST, Atkinson BA, Weaver LC . Confocal microscopic analysis reveals sprouting of primary afferent fibres in rat dorsal horn after spinal cord injury. Neurosci Lett 2000; 296: 65–68.
Jacob JE, Pniak A, Weaver LC, Brown A . Autonomic dysreflexia in a mouse model of spinal cord injury. Neuroscience 2001; 108: 687–693.
Weaver L, Verghese P, Bruce J, Fehlings M, Krenz NR, Marsh D . Autonomic dysreflexia and primary afferent sprouting after clip-compression injury of the rat spinal cord. J Neurotrauma 2001; 18: 1107–1119.
Jacob JE, Gris P, Fehlings MG, Weaver LC, Brown A . Autonomic dysreflexia after spinal cord transection or compression in 129Sv, C57BL, and Wallerian degeneration slow mutant mice. Exp Neurol 2003; 183: 136–146.
Marsh DR, Weaver LC . Autonomic dysreflexia, induced by noxious or innocuous stimulation, does not depend on changes in dorsal horn Substance P. J Neurotrauma 2004; 21: 817–828.
Marsh DR, Wong ST, Meakin SO, MacDonald JIS, Hamilton EF, Weaver LC . Neutralizing intraspinal Nerve Growth Factor with a trkA-IgG fusion protein blocks the development of autonomic dysreflexia in a clip-compression model of spinal cord injury. J Neurotrauma 2002; 19: 1531–1541.
Cameron AA, Smith GM, Randall DC, Brown DR, Rabchevsky AG . Genetic manipulation of intraspinal plasticity after spinal cord injury alters the severity of autonomic dysreflexia. J Neurosci 2006; 26: 2923–2932.
Groah SL, Stiens SA, Gittler MS, Kirshblum SC, McKinley WO . Spinal cord injury medicine. 5. Preserving wellness and independence of the aging patient with spinal cord injury: a primary care approach for the rehabilitation medicine specialist. Arch Phys Med Rehabil 2002; 83: S82–S98.
Acknowledgements
We thank Dave Pataky for technical assistance related to setting up the survey software and website. Additionally, we thank the Vancouver-based GF Strong Sexual Health Rehabilitation team for their input in the development of the questionnaire. Above all else, sincere gratitude is expressed to the community living with spinal cord injury for their continued willingness to provide input about important and real issues related to SCI to better enable researchers to ask and answer clinically relevant questions through experimental means.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Anderson, K., Borisoff, J., Johnson, R. et al. The impact of spinal cord injury on sexual function: concerns of the general population. Spinal Cord 45, 328–337 (2007). https://doi.org/10.1038/sj.sc.3101977
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101977
Keywords
This article is cited by
-
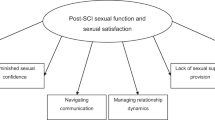
“You feel a bit unsexy sometimes”: The psychosocial impact of a spinal cord injury on sexual function and sexual satisfaction
Spinal Cord (2023)
-
Optimized multi-echo gradient-echo magnetic resonance imaging for gray and white matter segmentation in the lumbosacral cord at 3 T
Scientific Reports (2022)
-
Australian arm of the International Spinal Cord Injury (Aus-InSCI) Community Survey: 2. Understanding the lived experience in people with spinal cord injury
Spinal Cord (2022)
-
Sexual and Reproductive Health Experiences, Knowledge and Associations: A Neglected Issue Among Adults with Spinal Cord Injury in Sri Lanka
Sexuality and Disability (2022)
-
Evaluation of sexual reproductive health needs of women with spinal cord injury in Tehran, Iran
Sexuality and Disability (2022)