Abstract
Study design:
To prospectively evaluate major complications associated with the application of dynamic ABC plates (Aesculap, Tuttlingen, Germany) to multilevel Anterior Corpectomy/Fusion (ACF) followed by posterior fusion (C2–C7 PF).
Objectives:
To determine whether dynamic ABC (Aesculap, Tuttlingen, Germany) plates would minimize major complications (plate/graft extrusion, pseudarthrosis) while maximizing neurological outcomes in 40 consecutive patients undergoing simultaneous multilevel ACF/PF with halo application.
Setting:
USA.
Methods:
Patients averaged 53 years of age and preoperatively exhibited severe myeloradiculopathy (Nurick Grade 3.9). MR/CT studies documented marked ossification of the posterior longitudinal ligament/spondylostenosis. Surgery included two to four level ACF utilizing fibula strut allograft and ABC plates. Posterior spinous process wiring/fusions utilized braided titanium cables. The average operative time was 8.9 h. Fusion was confirmed on dynamic X-rays/CTs (3–12 months postoperatively). The average follow-up interval was 2.7 years. Outcomes (3 months–2 years postoperatively) were assessed utilizing Odom's Criteria, Nurick Grades, and SF-36 questionnaires.
Results:
Major complications included one pseudarthrosis requiring secondary PWF. Minor complications in six patients included two pulmonary emboli (PE), two tracheostomies, and five superficial wound infections. At 1 year postoperatively, marked improvement was observed in all patients utilizing Odom's criteria (38 excellent/good), Nurick Grades (mild radiculopathy 0.4), and the SF-36 (3 Health Scales; Role Physical (12.5–38.6), Bodily Pain (39.9–65.5), and Role Emotional (53.8–75.8)]. The 2-year postoperative data showed minimal additional improvement. The average time to fusion was 6.3 months.
Conclusion:
Patients undergoing multilevel ACF/PF demonstrated marked neurological improvement (SF-36), and only one of 40 developed a delayed pseudarthrosis.
Similar content being viewed by others
Introduction
Multilevel anterior corpectomy with fusion (ACF) performed with fixed-plates has been associated with a high incidence of major complications (graft/plate extrusion, pseudarthrosis).1 Vaccaro et al2 documented plate/graft-related failures for 9% of two level ACF and 50% of three level ACF. To avoid these failures, dynamic ABC plates (Aesculap, Tuttlingen, Germany) were prospectively applied for multilevel ACF (two to four level total corpectomies with additional partial cephalad/caudad corpectomy) with simultaneous posterior wiring and fusion (PWF) in 40 consecutive patients. All patients exhibited severe myeloradiculopathy attributed to ossification of the posterior longitudinal ligament (OPLL) and spondylostenosis. Major and minor complications along with surgeon-based (Odom's Criteria, Nurick Grades), and patient-based (Short-Form 36) outcomes were assessed.
Methods
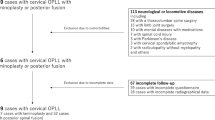
Forty consecutive patients undergoing circumferential cervical surgery for OPLL and spondylostenosis were prospectively evaluated (Figures 1, 2, 3, 4 and 5). Total corpectomies included the removal of 2–4 (average 2.3) complete vertebral bodies (Table 1). Note that by definition, a C3–C7 ACF was called a three level corpectomy; three total vertebrae were removed (C4–C6) and the partial cephalad (C3) and caudad (C7) corpectomies were omitted from this notation. All patients received fresh frozen fibula strut allografts and dynamic anterior cervical ABC plates (Aesculap, Tuttlingen, Germany) utilizing variable angle screws. Under the same anesthetic, patients had simultaneous C2–T1 PWF performed. These utilized individual spinous process braided titanium cable wiring to fibula strut allografts (33 patients) or a rod/eyelet construct (Vertex, Sofamor Danek, Memphis, TN) (7 patients) (Figures 6 and 7). Based on surgeon preference, halo braces were utilized in all patients until fusion occurred rather than cervico-thoracic orthoses (CTO). All posterior fusions were performed utilizing iliac crest autograft supplemented with demineralized bone matrix (ICM, Inductive Conductive Matrix, Sofamor Danek, Memphis, TN). Patients averaged 53 years of age (27–74), and included 27 males and 13 females. In all, 16 patients were smokers and were strongly advised to stop postoperatively. Preoperatively, patients typically exhibited severe myeloradiculopathy (average Nurick Grade 3.9). The average operative time was 8.9 h (range 6.5–11). The average transfusion requirement was 2.0 units (range 0–4). Fiberoptic postoperative extubation was performed on average 1.3 days postoperatively (range 1–7 days). Postoperative fusion was evaluated with dynamic X-rays and 2D–CT examinations performed at 3, 4.5, and 6 months postoperatively, and up to 12 months where indicated. The average follow-up interval was 2.7 years. Surgeon-based outcomes were assessed utilizing Odom's Criteria and preoperative and postoperative Nurick Grades. Patient-based outcomes were determined with SF-36 questionnaires administered preoperatively, and at 3 months, 6 months, 1 year, and up to 2 years postoperatively.
MR in patient also shown in Figure 1 with C2–C4 Klippel-Feil anomaly showing early OPLL characterized by hypertrophied posterior longitudinal ligament contributing to marked cord compression from C4 to C7. At surgery, the compression was due to early OPLL with an added disc herniation at the C4–C5 level. Dorsal intrusion from buckled yellow ligament was relieved following the anterior corpectomy and did not warrant laminectomy
The anterior corpectomy and fusion from C3 to C7 was performed with a fibula strut allograft and dynamic ABC plate. Posteriorly, a fibula strut was affixed to each of the C2–T1 spinous processes utilizing braided titanitum cable. The fusion was supplemented with iliac crest autograft and demineralized bone matrix (ICM: Sofamor Danek, Memphis, TN)
Anterior corpectomy and fusion performed from C4 to C7 with fibula strut allograft and ABC plate. Note, that the posterior spinous process wiring/fusion from C2 to T1 was performed utilizing titanium rods, eyelets (Vertex System (Sofamor, Danek, Memphis, TN)), and braided titanium cable without lateral mass screws. The posterior construct also included iliac crest autograft and demineralized bone matrix (ICM: Sofamor Danek, Memphis, TN)
Results
The average time to fusion documented on dynamic X-rays and 2D–CT studies postoperatively was 6.3months (range 4–9 months) (Table 1). Only one patient developed both a major (defined as requiring secondary surgery directly related to graft/plate failure, pseudarthrosis) and a minor (medical management/warranting no secondary spinal surgery) complication (Table 2). He was an obese 48-year-old male (6′4″, 280 lbs) who developed pseduarthrosis 6 months postoperatively and required a second posterior fusion; he fused 6 months later. He also developed halo pin-site cellulitis 4 months following the second surgery, which was treated with halo removal followed by the application of a hard cervico-thoracic orthosis, and 10 days of intravenous antibiotics.
The remaining six patients developed overlapping minor complications (Table 2). A 44-year-old male substance abuser, developed a posterior cervical wound infection and DVT 10 days postoperatively; treatment included 6 weeks of intravenous antibiotics and an inferior vena cava filter (IVC); DVT resolved and required no heparin-based therapy. A 51-year-old male developed DVT 6 days postoperatively. An attempt at placement of a removable filter (Bard) resulted in embolization of this device to the right ventricle; a permanent filter was placed on the 7th postoperative day (Greenfield), and the embolized filter was removed via thoracotomy on the 13th postoperative day without incident. A moderately obese (5′2″, 180 lbs) 60-year-old female, developed a posterior cervical wound infection 6 days postoperatively and DVT with pulmonary emboli (PE) 10 days postoperatively; the former was treated with 6 weeks of intravenous antibiotics and the latter with IVC filter placement and Heparin followed by Warfarin. A 68-year-old obese male (5′10″, 240 lbs) with severe diabetes, hypertension, myocardial infarctions, chronic obstructive pulmonary disease and past pneumonias, developed DVT and PE on postoperative day 14 requiring a tracheostomy and intravenous Heparin followed by Warfarin. A 44-year-old morbidly obese (5′2″, 300 lbs) female with asthma, required a tracheostomy on postoperative day 7, and developed a posterior cervical wound infection on postoperative day 14 requiring wound debridement plus 6 weeks of intravenous antibiotics. A 59-year-old obese male (5′9″, 260 lbs) developed a halo-pin site cerebritis 6 months postoperatively managed with halo removal and 6 weeks of intravenous antibiotics.
Outcomes
Based on Odom's criteria, patients exhibited 35 excellent, three good, and two fair outcomes 1 year postoperatively. They also improved from showing severe preoperative myelopathy (average Nurick Grade 3.9) to demonstrating mild residual postoperative radiculopathy (average Nurick Grade 0.4).
Postoperative SF-36 scores demonstrated gradual improvement over the first postoperative year. Quantitative (Table 3a) data were placed into four qualitative categories to simplify data analysis (Table 3b); patients were graded as worse (negative numbers), or showing minimal (1–4 Points), mild (5–10 Points), moderate (11–20 Points), or marked (>20 Points) improvement. Three months postoperatively, worsening was noted on 3 (General Health (GH), Social Function (SF), Mental Health (MH)), minimal improvement was seen on five (Physical Function (PF), GH, SF, Role Emotional (RE), MH), minimal improvement on one (Role Physical (RP)), and mild improvement on two (PF), and Vitality (V) Health Scales. At 6 months following surgery, one demonstrated worsening (PF), one showed minimal (GH), three demonstrated mild (V, SF, MH), two showed moderate (BP, RE), and one showed marked improvement (RP). One year following surgery, one was worse (GH) one showed minimal (PF), two showed mild (V, MH), one showed moderate (SF), while three showed marked improvement (RP, BP, RE).
Conclusion
Outcome data
Surgeon-based Odom's criteria have typically been utilized to evaluate the results of anterior cervical surgery performed with and without fixed plates.2, 3, 4, 5, 6 Odom's criteria yielded 90% good/excellent results for one level anterior diskectomy/fusion (ACDF) performed with fixed plates and 88% without plates in Wang, McDonough, Endow et al7 series. Comparable rates of fusion and similar clinical outcomes (Odom's criteria) followed fixed-plated two level ACDF (32 patients) when compared with one level plated ACF (20 patients).8 In another series, utilizing Odom's criteria, 36 of 39-plated two level ACDF (allograft) exhibited excellent to good outcomes compared with 23 of 25 nonplated patients (allograft).9 Epstein utilized both Odom's criteria and Nurick Grades to evaluate outcomes of anterior cervical procedures varying from nonplated single level anterior diskectomy/fusion to plated multilevel circumferential operations.10, 11, 12, 13, 14, 15, 16, 17
Anterior cervical surgical series have increasingly utilized the patient-based SF-36. In Klein, Vaccaro and Albert's series of two level ACDF (28 patients), patients demonstrated significant postoperative improvement on five Health Scales: Bodily Pain (P<0.001) V (P=0.003), PF (P=0.01) RP (P=0.003) and SF (P=0.0004).18 Epstein utilized Nurick Grades, Odom's criteria, and/or SF-36 to evaluate single level ACF procedures performed with fixed or dynamic-plate systems, with or without iliac crest reconstruction.19, 20, 21, 22
Other studies focus on integrating surgeon and patient-based outcome data. One spinal series utilized the SF-36, the Oswestry questionnaire, and the Low Back Pain Disability Scale.23 Another study, evaluating neck pain for patients undergoing ACDF (87 patients), employed the Visual Analog Scale, North American Spine Society Satisfaction Questionnaire, the Modified Roland and Morris Disability Index, and the modified Oswestry Disability Questionnaire.24 Evaluating 80 patients with cervical myelopathy, King and Roberts determined that the SF-36 proved ‘valid’ when compared with surgeon-based Nurick, Cooper Harsh, and a Western modification of the Japanese Orthopedic Association Scores.25 Hacker et al26 found that results following single-level ACDF utilizing cervical fusion cages versus noninstrumented procedures yielded similar results on both the Visual Analog Pain Scale and the SF-36.
Few have applied Odom's Criteria, Nurick Grades, and the SF-36 to evaluate the results of circumferential cervical surgery.27 In a prior partially overlapping series of patients undergoing fixed-plated (28 patients) and dynamic-plated (19 patients) multilevel ACF accompanied by simultaneous PWF, 1 and 2 year postoperative data utilizing these three techniques was collected. For both the first and second postoperative years, Odom's Criteria demonstrated 31/47 good/excellent results. Over the same period, Nurick Grades demonstrated mild radiculopathy/myelopathy, with mild improvement noted between the 1st and 2nd years with respective Nurick Grades of 0.8 to 0.4. In comparison, the 40 patients undergoing dynamic-plated multilevel ACF with PWF, Nurick Grades and Odom's criteria demonstrated maximal improvement 1 year postoperatively with 38 of 40 demonstrating excellent/good outcomes (Odom's Criteria) and all patients exhibited only mild residual radiculopathy/myelopathy (average Nurick Grade 0.4) (Table 1).
In both, a prior overlapping series27 and the present study, SF-36 data demonstrated maximal improvement by the first postoperative year (Table 3a and b). In the previous series employing fixed plates (23 patients) and dynamic-plates (19 patients) to perform 47 multilevel ACF accompanied by PWF, SF-36 data demonstrated little difference in the degree of improvement occurring between the first and second postoperative years. At 1 year postoperatively, patients exhibited moderate improvement on five Health Scales (SF, BP, RP, PF, RE), with two showing mild (MH, V), and one demonstrating minimal improvement (GH). By the second postoperative year, marked improvement was noted on one (RP), moderate improvement on three (SF, BP, PF), mild improvement on three (RE, MH, V), and minimal improvement on one (GH) Health Scale. In the present study, utilizing only dynamic ABC plates for all 40 patients undergoing multilevel ACF with PWF, progressive improvement from 3 to 6 month postoperative data were observed 1 year postoperatively on 3 of 8 Health Scales: RP, and Bodily Pain, with RE. RP and Bodily Pain seem to consistently reflect maximal improvement in these two series, while GH, V, and MH appear to show the smallest changes before and following operative intervention; the remaining 3 Health Scales fall somewhere in between. Note that the degree of neurological improvement documented on the SF-36 was not attributed to either the utilization of fixed or dynamic-plating devices, as both fixed and dynamic-plates had been utilized in the series cited.
Dynamic-plate versus fixed plate considerations
The dynamic-plate was developed secondary to failures encountered utilizing fixed-plated systems particularly for multilevel anterior cervical constructs, typically corpectomies (Figure 8). Vaccaro et al2 observed a 9% failure rate following fixed-plated two level ACF and a 50% failure rate with three level ACF performed without simultaneous posterior fusions. Schultz et al28 later observed a 100% fusion rate for 64 patients undergoing fixed-plated two and three level ACF accompanied by simultaneous lateral mass plating; 2 years postoperatively, 1 plate dislodged while 15 of 516 lateral mass screws partially ‘backed out’ (none required secondary surgery). For multilevel ACF performed with simultaneous posterior fusion, the author previously determined that three of 22 nonplated patients experienced failures, and successively that five of 38 fixed-plated patients required secondary surgery attributed to fixed-plate failures (major complications: graft/plate extrusion, pseudarthrosis).10, 16, 27 In this study, the safety and efficacy of dynamic ABC plates for multilevel anterior cervical constructs accompanied by simultaneous posterior fusion were demonstrated, as here, only one (2.5%) of 40 patients developed pseudarthrosis warranting secondary posterior fusion 6 months postoperatively.
At 6 weeks following a fixed-plated (Orion: Sofamor Danek, Memphis, TN) C3–C7 ACF with C2–T1 PWF, the patient complained of dysphagia. Although the lateral X-ray and CT showed anterior/inferior plate extrusion, the graft remained in place. The patient was maintained in the halo device until fusion occurred 6 months postoperatively as shown on this mildine sagittal 3D–CT study, and then underwent anterior plate removal for persistent dysphagia
Other considerations
The choice for spinous process wiring for posterior fusion over lateral mass screw/plate placement was based on surgeon preference (ease, rapidity and safety of application) and on its FDA approval status. Certainly, lateral mass plates as utilized by Schultz et al28 constitute part of the ‘standard of care’ for posterior fusion, and are preferred by many surgeons, although not FDA approved in the US.
Additionally, surgeon preference led to the choice of halo bracing postoperatively rather than utilization of cervico-thoracic orthoses. Of note, in Vaccaro et al's study, the 9% extrusion rate for two level plated ACF, and 50% failure rate for three level plated ACF (both without posterior fusions) were comparable whether patients wore halo devices or CTO orthoses.2
Conclusions
One of the 40 patients undergoing complex circumferential cervical surgery developed a major postoperative complication, pseudarthrosis, warranting secondary posterior fusion; no other graft or plated-related complications, no cerebrospinal fluid fistulas, no cord or root deficits, and no deaths were encountered. Six other patients developed overlapping minor complications. Furthermore, patients exhibited marked neurological improvement based on Odom's Criteria (38 good/excellent), Nurick Grades (average+3.5), and the SF-36 outcomes questionnaire (+22 to +26.1 on three Health Scales). Multilevel ACF performed utilizing dynamic-plates, accompanied by PWF, proved to be safe and effective while promoting excellent outcomes.
References
Ware JE . Scoring the SF-36. In: SF-36 Health Survey: Manual and Interpretation Guide. Nimrod Press: Boston Mass 1993, pp 6:1–6:22.
Vaccaro AR et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord (US) 1998; 11: 410–415.
Saunders RL, Pikus HJ, Ball P . Four-level cervical corpectomy. Spine 1998; 23: 2455–2461.
Fessler RG, Steck JC, Giovanini MA . Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery (US) 1998; 43: 257–265.
Eleraky MA, Llanos C, Sonntag VK . Cervical corpectomy: report of 185 cases and a review of the literature. J Neurosurg (US) 1999; 90 (Suppl): 35–41.
Macdonald RL et al. Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg (US) 1997; 86: 990–997.
Wang JC et al. The effect of cervical plating on single-level cervical diskectomy and fusion. J Spinal Disord 1999; 12: 467–471.
Wang JC et al. A comparison of fusion rates between single-level cervical corpectomy and two-level diskectomy and fusion. J Spinal Disord (US) 2001; 14: 222–225.
McLaughlin MR, Purighalla Y, Pizzi FJ . Cost advantages of two-level anterior cervical fusion with rigid internal fixation for radiculopathy and degenerative disease. Surg Neurol (US) 1997; 48: 560–565.
Epstein NE . Circumferential surgery for the management of cervical ossification of the posterior longitudinal ligament. J Spinal Disord 1998; 11: 200–207.
Epstein NE . The surgical management of ossification of the posterior longitudinal ligament in 51 patients. J Spinal Disord (US) 1993; 6: 432–454.
Epstein NE . The surgical management of ossification of the posterior longitudinal ligament in 43 North Americans. Spine 1994; 19: 664–672.
Epstein NE . Advanced cervical spondylosis with ossification into the posterior longitudinal ligament and resultant neurologic sequelae. J Spinal Disord 1996; 9: 477–484.
Epstein NE . The value of anterior cervical plating in preventing vertebral fracture and graft extrusion following multilevel anterior cervical corpectomy with posterior wiring/fusion: indications, results, and complications. J Spinal Disord 2000; 13: 9–15.
Epstein NE . Anterior cervical diskectomy and fusion without plate instrumentation in 178 patients. J Spinal Disord 2000; 13: 1–8.
Epstein NE . Anterior approaches to cervical spondylosis and OPLL: review of operative techniques and assessment of 65 multilevel circumferential procedures. Surgical Neurology 2001; 55: 313–324.
Epstein NE . Reoperation rates for acute graft extrusion and pseudarthrosis following one level anterior corpectomy and fusion with and without plate instrumentation: etiology and corrective management. Surg Neurol 2001; 56: 73–81.
Klein GR, Vaccaro AR, Albert TJ . Health outcome assessment before and after anterior cervical diskectomy and fusion for radiculopathy: a prospective analysis. Spine (US) 2000; 25: 801–803.
Epstein NE . The management of 1 level anterior cervical corpectomy with fusion employing Atlantis hybrid plates: preliminary experience. J Spinal Disord 2000; 13: 324–328.
Epstein NE . The efficacy of anterior dynamic plates in complex cervical surgery. J Spinal Disord Tech 2002; 15: 221–227.
Epstein NE . Anterior cervical dynamic ABC plating with single level corpectomy and fusion in 42 patients. Spinal Cord 2003; 41: 153–158.
Epstein NE . Does iliac crest reconstruction affect postoperative pain following single level anterior corpectomy with fusion? J Spinal Disord Tech 2004; 29: 1340–1345.
Grevitt M et al. The short form-36 health survey questionnaire in spine surgery. J Bone Joint Surg Br (England) 1997; 79: 48–52.
Garvey TA et al. Outcome of anterior cervical diskectomy and fusion as perceived by patients treated for dominant axial-mechanical cervical spine pain. Spine (US) 2002; 27: 1887–1895.
King JT, Roberts MS . Validity and reliability of the Short Form-36 in cervical spondylotic myelopathy. J Neurosurg (US) 2002; 97 (Suppl): 180–185.
Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL . A prospective randomized mulitcenter clinical evaluation of an anterior cervical fusion cages. Spine (US) 2000; 25: 2646–2654.
Epstein NE . Circumferential cervical surgery for cervical ossification of the posterior longitudinal ligament: a multianalytic outcome study. Spine 2004; 29: 1340–1345.
Schultz KD, McLaughlin MR, Hasid RW, Comedy CH, Rots GE, Alexander J . Single-stage anterior – posterior decompression and stabilization for complex cervical spine disorders. J Neurosurgery (US) 2000; 93 (Supply): 214–221.
Acknowledgements
I thank the Joseph A Epstein Neurosurgical Education Foundation, Aesculap (Tuttlingen Germany) for their support, and Joseph E Epstein MD and Ms Sherry Grimm (Administrator, Long Island Neurosurgical Assoc. PC) for their editorial assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Epstein, N. Dynamic anterior cervical plates for multilevel anterior corpectomy and fusion with simultaneous posterior wiring and fusion: efficacy and outcomes. Spinal Cord 44, 432–439 (2006). https://doi.org/10.1038/sj.sc.3101874
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101874
Keywords
This article is cited by
-
Long-term follow-up results of the Cloward procedure for cervical spondylotic myelopathy
European Spine Journal (2013)
-
The biomechanics of spinal fusion
ArgoSpine News & Journal (2010)