Abstract
Study design:
A case report.
Objective:
To raise awareness among spinal cord clinicians of the possible carcinogenic effect of phenoxybenzamine and of the rare occurrence of small cell carcinoma in the neuropathic bladder.
Setting:
Regional Spinal Injuries Centre and District General Hospital, Southport, Merseyside, United Kingdom.
Case report:
A 28-year-old man sustained a fracture dislocation of L-1 with consequent paraplegia (ASIA impairment scale A). Phenoxybenzamine treatment enabled his indwelling catheter to be discarded in favour of a penile sheath, but it caused unacceptable dizziness and was stopped after 7 years. After 20 years, he developed chronic lymphocytic leukaemia, which was treated with chlorambucil and fludarabine. After 2 years, investigation of bilateral hydronephrosis revealed a primary small cell carcinoma of the bladder with coexistent squamous dysplasia. Uraemia supervened and, declining active treatment, the patient died 3 weeks after diagnosis.
Conclusion:
Phenoxybenzamine, a known carcinogen in rodents, is likely also to be carcinogenic in humans, and patients with spinal cord injury who have received the drug for any significant period of time, need close follow-up to allow early detection of cancer. Phenoxybenzamine should not be prescribed on a long-term basis, and should instead be replaced with a selective alpha-blocker.
Similar content being viewed by others
Introduction
Phenoxybenzamine hydrochloride was originally prescribed to selected patients with spinal cord injury (SCI) to facilitate bladder emptying, but its use declined with the advent of selective alpha-1 adrenergic blockers.1 The drug is carcinogenic and mutagenic in rodents, causing peritoneal sarcomas when administered intraperitoneally, and tumours of the gastro-intestinal tract (including squamous cell carcinoma of the stomach) after 2 years' oral dosing.2 According to the National Institute of Occupational Health and Safety, phenoxybenzamine can be ‘reasonably anticipated’ to be a human carcinogen.3 Nettesheim and associates reported the case of a squamous cell carcinoma of the oesophagus in a 20-year-old woman, who had been treated with phenoxybenzamine for over 12 years for bladder dysfunction caused by tethered cord syndrome. The German Admission Board recommends phenoxybenzamine only for short-term therapy, and the authors recommend that it should only be used on a long-term basis with particular care.4 The British National Formulary (BNF) lists ‘short-term management of hypertensive episodes in phaeochromocytoma’ as the only indication for the use of phenoxybenzamine. The BNF recommends the use of selective alpha-blockers (such as alfuzosin, doxazosin, indoramin, prazosin, tamsulosin or terazosin) for the long-term treatment of chronic retention of urine or benign prostatic hyperplasia.5
Here we report the case of a SCI patient, who was prescribed phenoxybenzamine for 7 years to facilitate emptying of the urinary bladder and who, 20 years later, developed chronic lymphocytic leukaemia and both small cell carcinoma and squamous neoplasia of the urinary bladder. In doing so, we highlight the possible association between long-term phenoxybenzamine therapy and late onset malignancy in SCI patients.
Case report
In 1975, a 28-year-old man was working in a lift when the cable broke, causing the lift to fall 40 feet. He suffered a fracture–dislocation of the body of the first lumbar vertebra with paraplegia below that level (ASIA impairment scale A). The fracture was treated conservatively, and his neuropathic bladder was managed initially by using an indwelling catheter. At 5 months after the injury, he was started on oral phenoxybenzamine (at a dose of 10 mg in the morning and 20 mg at night), which allowed him to empty his bladder effectively with little residual urine. He was therefore, able to discard the indwelling catheter in favour of a penile sheath. The patient took phenoxybenzamine for 7 years, from 1975 to 1982, until dizzy spells became unacceptable. He was still able to use a penile sheath and managed to pass urine by straining.
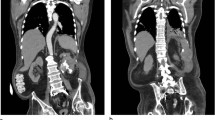
Intravenous urography (IVU) in 1985 showed bladder trabeculation with diverticulae; the kidneys and ureters were normal. IVU in 1989 confirmed that both kidneys were functioning with no evidence of obstruction. In 2002, he passed blood clots in his urine. Investigations showed a lymphocytosis of 158.20 × 109/l, with a haemoglobin concentration of 10.1 g/dl. Lymphocyte markers were typical of chronic lymphocytic leukaemia, and treatment with chlorambucil and fludarabine was instituted. Repeat IVU in June 2002 confirmed preserved function in both kidneys, with caliectasis in the upper pole of the left kidney. Computed tomography of the abdomen at this time revealed marked splenomegaly, with several small para-aortic and mesenteric lymph nodes. Ultrasound scanning performed in January 2004 showed bilateral hydronephrosis with marked thickening (up to 4.3 cm) of the lateral and posterior bladder walls. Colour Doppler scan showed increased vascularity and the appearances were highly suspicious of malignant infiltration. Magnetic resonance imaging of the pelvis confirmed gross, almost circumferential thickening of the bladder wall, most marked anteriorly where the wall was over 5 cm thick, but without infiltration of the perivesical fat (Figure 1). In addition, there were bilateral iliac lymph node masses (measuring up to 3 cm in diameter), para-aortic lymphadenopathy and splenomegaly. Bilateral hydronephrosis and ureteric dilatation were confirmed. The radiological appearances were consistent with leukaemic infiltration of the bladder.
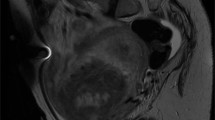
Urine cytology (using the Cytospin method) showed atypical keratinising and nonkeratinising squamous cells, in an acute inflammatory background, the appearances being highly suspicious of squamous cell carcinoma. In addition, a further population of atypical small cells with enlarged irregular nuclei and no visible cytoplasm was interpreted as being of lymphoid origin, suggestive of coexistent leukaemic infiltration (Figure 2).
Cystoscopy showed tumour covering the entire bladder mucosa. Histological examination of bladder biopsy showed infiltration by a solid, nonpapillary malignant tumour composed of small dark cells with inconspicuous cytoplasm, invading the muscularis propria (Figure 3). The surface urothelium was fairly well preserved with no evidence of transitional cell dysplasia or carcinoma – in situ. There was extensive nonkeratinising squamous metaplasia, together with a single strip of atypical squamous epithelium showing moderate dysplasia (Figure 4). Invasive squamous cell carcinoma was not identified in the material available for examination.
Immunohistochemical staining of the invasive tumour showed negative staining for CD45 (leukocyte common antigen) (Figure 5), and HMB45 (melanoma marker). There was patchy, dot-like paranuclear positivity for cytokeratin MNF116, and strong positivity with CD56 (a neural cell adhesion molecule) (Figure 6), and with synaptophysin. This immunophenotype is characteristic of small cell carcinoma, and excludes leukaemic infiltration. Immunostaining for TTF-1 (thyroid transcription factor) was generally negative but with areas of weak-to-moderate positivity; this raised the possibility of metastasis from a primary bronchial carcinoma, but a normal chest X-ray excluded this. The final diagnosis was therefore primary small cell carcinoma of the urinary bladder with possible, coexistent squamous cell carcinoma.
The patient developed uraemia secondary to bilateral hydronephrosis and, declining active treatment, died 3 weeks after diagnosis. An autopsy was not carried out.
Discussion
Small cell carcinoma of the urinary bladder is rare, accounting for less than 1% of primary bladder tumours.6 It is considered to be at the malignant end of the spectrum of neuroendocrine tumours, and is assumed to arise from multipotent undifferentiated stem cells in the bladder urothelium.7 Histologically, the tumour is identical to its more common counterpart in the bronchus. The main differential diagnosis is lymphoma, and immunohistochemistry is often used to confirm the diagnosis. The tumour is negative for leucocyte common antigen (which is usually positive in lymphoma), and exhibits typical paranuclear dot-like staining with the anticytokeratin antibody MNF116. It stains variably with antichromogranin (which recognises a membrane component of the dense-core vesicles of neuroendocrine cells), but stains more consistently and strongly with other neuroendocrine markers including CD56 and synaptophysin.
Small cell carcinoma is more aggressive than transitional cell carcinoma, with an increased tendency to infiltrate the muscle layer and to metastasise.6 Cassidy and Kaye8 reported a case of small cell carcinoma of the bladder in a 40-year-old man with tetraplegia, who was treated with chemotherapy consisting of ifosfamide, mesna, carboplatin and etoposide. Our patient developed progressively increasing serum creatinine levels. We planned to treat this patient with chemotherapy after bilateral nephrostomy, but he declined any active intervention. We respected his wishes and he died peacefully of renal failure 3 weeks after trans-urethral resection.
Conclusion
Phenoxybenzamine, a known carcinogen in rodents, may reasonably be supposed to be carcinogenic in humans also. SCI patients treated with phenoxbenzamine on a long-term basis need close follow-up to allow early detection of any malignancy that should develop. Patients currently taking phenoxybenzamine should be switched to an appropriate selective alpha-blocker instead.
References
Vaidyanathan S, Rao MS, Sharma PL, Chary KS, Swamy RP . Possible use of indoramin in patients with chronic neurogenic bladder dysfunction. J Urol 1983; 129: 96–101.
Department of Health & Human Services, Public Health Service, Food and Drug Administration, USA. 15 January 2003. http://www.fda.gov/cder/foi/appletter/2003/08708slr022ltr.pdf.
The Registry of Toxic Effects of Chemical Substances, National Institute of Occupational Health and Safety, USA. June 2000. http://www.cdc.gov/niosh/rtecs/dp393870.html.
Nettesheim O, Hoffken G, Gahr M, Breidert M . Haematemesis and dysphagia in a 20-year-old woman with congenital spine malformation and situs inversus partialis. Z Gastroenterol 2003; 41: 319–324.
British National Formulary. Vol 49, British Medical Association and Royal Pharmaceutical Society of Great Britain, London, March 2005, p 96.
Munoz VD, Garcia-Miralles GR, Amengual AI, Benejam GJM . Small cell carcinoma of the bladder. Report of a new case and review of the literature. Actas Urol Esp 2002; 26: 811–815.
Porcaro AB et al. Small cell carcinoma of the bladder. Report of 3 cases and review of the literature. Arch Ital Urol Androl 2002; 74: 142–145.
Cassidy J, Kaye SB . An unusual case of haematuria. Eur J Cancer 1993; 29A: 906–907.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Vaidyanathan, S., Mansour, P., Soni, B. et al. Chronic lymphocytic leukaemia, synchronous small cell carcinoma and squamous neoplasia of the urinary bladder in a paraplegic man following long-term phenoxybenzamine therapy. Spinal Cord 44, 188–191 (2006). https://doi.org/10.1038/sj.sc.3101789
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101789