Abstract
Study design:
Cystic dilatation of the fifth ventricle on its own is an extremely rare pathological event in adults whose pathogenesis is uncertain. The authors describe a personal case of ‘fifth ventricle’ and review the pertinent literature.
Objective:
To emphasize the importance of including the fifth ventricle in differential diagnosis of lesions of the conus medullaris to ensure proper treatment.
Setting:
Italy.
Methods:
A 30-year-old woman was referred to us for recurrent low back pain. The patient was assessed by clinical, electrophysiological (motor evoked potential, somatosensorial evoked potential and electromyography of the perineal and lower limb muscles) and urodynamic investigations as well as a magnetic resonance imaging (MRI) of the lumbar–sacral segment with and without gadolinium enhancement, subsequently extended to the entire vertebral column and brain. Follow-up consisted of periodic clinical evaluation and lumbar–sacral MRI after 1 and 2 years.
Results:
General physical examination, electrophysiological and urodynamic investigations were all negative, confirming the subjective nature of the patient's symptoms. Lumbar–sacral MRI demonstrated the presence of a cyst lesion containing cerebrospinal fluid (CSF), which did not enhance after gadolinium, compatible with the diagnosis of the terminal ventricle. By extending the MRI investigation to the entire vertebral column and brain, it was possible to exclude an association with other malformations of the central nervous system. Clinical and radiological follow-up confirmed the nonevolutive nature of the lesion 1 and 2 years later.
Conclusions:
The lack of clinical symptoms and the stability of the radiological situation at 1 and 2 years follow-up motivated our choice of conservative treatment.
Similar content being viewed by others
Introduction
The term ventriculus terminalis or fifth ventricle is used to describe a cavity containing cerebrospinal fluid (CSF) localized inside the conus medullaris, delimited by normal ependymal tissue. Described for the first time by Stilling in 1859, it was Krause in 1875 who introduced the term ‘fifth ventricle’ after having observed that the walls of the cavity were made up of normal ependymal cells. It may be present on its own or be associated with malformative pathologies of the central nervous system (Arnold–Chiari syndrome, syringohydromyelia, tethered cord, spina bifida, myelomeningocele, etc). In adults, the isolated form is extremely rare. Currently, only 17 cases are described in the literature to which we add the case reported here.
Materials and methods
A 30-year-old woman was referred to us about a year ago for mild, nonspecific symptoms, which were subjective in nature and characterized by recurrent bouts of low back pain, which did not respond to medical treatment with nonsteroid anti-inflammatory drugs and corticosteroids. Scrupulous investigation failed to bring to light any previous traumatic spinal injuries.
Lumbar–sacral magnetic resonance imaging (MRI), performed elsewhere, showed the presence of a small, roundish cavity with regular borders, not sepimented, filled with a liquid with the same intensity as CSF both in T1 (hypointensity) and T2 (hyperintensity) sequences without contrast enhancement after paramagnetic contrast medium. The nerve tissue adjacent to the lesion had been reduced to a thin layer. During hospitalization, the patient underwent careful clinical evaluation and neurophysiological tests including: motor evoked potential (MEP), somatosensorial evoked potential (SEP) and electromyography (EMG) of the muscles of the lower limbs and perineal plane, as well as urodynamic investigations and lumbar–sacral plain X-ray. Another lumbar–sacral MRI was performed, with and without contrast, and completed by extending the investigation to the cervical–thoracic segment and brain. The patient was then submitted to follow-up which consisted of periodic clinical assessment and lumbar–sacral MRI at 1 and 2 years.
Results
Neurological examination did not reveal any strength deficits, motor or sensory deficits. The negative findings of neurophysiological tests (MEP, SEP, EMG of the perineal and lower limb muscles), as well as the urodynamic tests performed, revealed the nonspecific and predominantly subjective nature of the clinical symptoms and confirmed the absence of any neurological deficits or sphincter disorders.
Plain X-ray showed a moderate facet joint ipertrophy that could explain the patient's lumbar back pain.
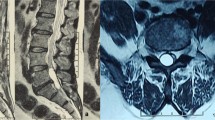
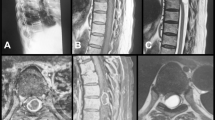
The second lumbar–sacral MRI investigation confirmed the presence of a cystic lesion localized inside the conus medullaris and epiconus (Figure 1). This area extended for about 16 mm from T12 to L1. The lesion appeared with regular borders and was not sepimented, whose contents showed a normal CSF signal in all the sequences performed (Figure 2). The perilesional nerve tissue was reduced to a layer less than 2 mm in thickness, because of the mass effect of the cyst.
The sequences obtained after gadolinium administration showed the absence of enhancement of the cyst wall (Figure 3), thus allowing a differential diagnosis with tumoral lesions of the conus medullaris. The study was extended to include the entire vertebral column and brain in order to rule out an eventual association with other malformative pathologies of the central nervous system.
Subsequent serial outpatient examinations and MRI of the lumbar–sacral spine, performed 1 and 2 years later, demonstrated the nonevolutive nature of the lesion in terms of both clinical and neuroradiological findings.
Discussion
The ventriculus terminalis or fifth ventricle can be considered as a normal step of embryonal development of the spinal cord, characterized by three phases: neurulation, canalization and regressive differentiation.1, 2, 3, 4, 5, 6, 7 The process of neurulation, which begins at 3 weeks of embryonic age, leads to the formation of the neural tube by a progressive fusion of the lateral edges of the neural plate starting from the level, of the third and fourth somite. From this level, the fusion process progresses at the same time cephalad and caudad. The craniocephalad and caudad closure, respectively, occur at around 23 and 26 gestation days. Neurulation, which is completed by about 4 weeks, is at the origin of the majority of the spinal cord. The subsequent phases of canalization and regressive differentiation give rise to development of the conus medullaris, the filum terminalis and the ventriculus terminalis by means of formation of a second distal neural tube. This structure originates from vacuolization of undifferentiated aggregated cells called ‘caudal cell mass’, formed from the fusion of the notocord and neurepithelium, caudally to the posterior neuropore. Progressive coalescence of the vacuoles leads to formation of an ependyma-lined tube that usually fuses with the more rostral central canal. The final stage is characterized by necrosis processes that result in dilatation of the portion of the ependymal canal located at the level of the conus medullaris, forming the fifth ventricle and a fibrous structure called the filum terminalis into which the ventriculus terminalis may extend.2, 3, 4, 6
During the first 5 years of life, evidence of a fifth ventricle not accompanied by other pathologies is, according to Coleman et al,3 a frequent finding that does not have pathological significance.
In adulthood, the persistence of a fifth ventricle, especially when unaccompanied by other malformative pathologies of the central nervous system, is extremely rare.2, 5
The fact that the development process of the fifth ventricle is extremely variable means that there may be either a single cavity directly communicating with the central canal of the ependyma (more frequent in pediatric age) or an isolated cystic cavity of the spinal canal. The different morphological entities observed in both adults and children could merely be variants of the normal process of canalization and could therefore be attributed to a continuum of evolution of the conus medullaris.3, 4
Today, the mechanisms involved in the formation of an isolated cystic expansion of the conus medullaris in the adult are not yet well known. Many pathogenetic hypotheses have been formulated in the past years. Aboulker's theory is based on the presence of an obstruction to the CSF circulation at the craniocervical junction level with the subsequent pathological pressure gradient between intracranial and medullary subarachnoidal spaces.
This would determine a pathological circulation of the liquor within the nervous parenchyma.
Nevertheless, validity of such theory has not been confirmed by the reduction or disappearance of the cyst as a result of a decompressive suboccipital craniectomy.8 Localization of a syringomyelic cavity at the conus medullaris is a rare event and is always associated to a cranial extension.1 A severe dorsolumbar spinal cord injury could be the ‘primum movens’ in the development of a cystic cavity (post-traumatic syringomyelia); the following increase in size of the lesion would be caused by medullary hemorrhagic necrosis phenomena. Other factors contributing to the lesion's enlargement would be fibrotic and arachnoiditic processes, secondary to post-traumatic meningeal hemorrhages, and transcystic pressure gradient modifications caused by post-traumatic stenosis and deformities of the vertebral canal.2 However, in most cases of the fifth ventricle described in the literature, there is no history of trauma.
Currently, most of the authors1, 2, 3, 4, 5, 6, 7 believe that isolated cystic dilatation of the fifth ventricle is due to the persistence of this lesion in adulthood and to the abnormal closure of the communication between the ventriculus terminalis and the central canal by ependyma (disembryogentic theory).
This lack of communication may also be found in many variants of normal embryonic development of the conus medullaris as the presence of accessory lateral and dorsolateral canals, which may or may not communicate with the central canal (forking). Lendon and Emery showed that 10% of healthy adults have major forking of the canal in the conus, and 35% have minor forking.
The scarcity of clinical symptoms and the slow evolution of the lesion observed in the cases submitted to follow-up seem to favor the disembryogenetic theory rather than the other hypotheses put forward so far (thoracolumbar traumatic injury,2 syringomyelia,8 etc.). Of the 17 cases described in the literature, 13 presented ingravescent or, at least, invalidating symptoms,1, 5, 6, 7, 8, 9, 10, 11, 12 whereas in the other 4, clinical status remained stable at follow-up.2, 6, 13 However, clinical symptoms were entirely nonspecific, even in the cases that evolved, ranging from just low back pain (as in our case) to deficits (lower limb paresis, sphincter dysfunction, etc.). It is precisely this lack of specific findings at clinical, neurophysiological and urodynamic assessment, which, at the best, makes it possible to locate the site of the lesion, which makes MRI of the lumbar–sacral spine a fundamental investigation for diagnosing cystic dilatation of the fifth ventricle. Ventricular dilatation appears on MRI as a small, roundish cavity with regular borders, which is not sepimented and is filled with a liquid of the same intensity of CSF both on T1 and T2 sequences, without enhancement after injection of paramagnetic contrast medium. This allows a differential diagnosis with tumoral lesions of the conus medullaris, which display a more or less marked enhancement of the cyst wall. Moreover, MRI makes it possible to identify the isolated forms of the fifth ventricle by ruling out any association with other malformative lesions.1, 5, 6, 9, 10, 13 An analysis of the data shows that cystic dilatation of the fifth ventricle has two possible types of clinical evolution: in the first, there is a mild clinical onset characterized by a few, nonspecific symptoms and long-term stability of both clinical and radiological parameters, as in our case; alternatively, there may be an evolution of symptoms presumably due to an increase in the size of the cystic lesion inside the conus medullaris.2 Once a diagnosis of fifth ventricle has been made, two types of treatment are possible: surgical or conservative. Of the 17 cases described, 14 underwent surgical treatment consisting of emptying of the cyst and marsupialization,5, 6, 7, 8, 9, 10, 11, 12 because they presented progressively worsening or, in any case, invalidating symptoms: regression of clinical symptoms was achieved in six of these cases1, 5, 7, 8, 10, 12 and marked clinical improvement in six.7, 11, 12 Postoperative control MRI was performed in seven cases1, 6, 8, 9, 10 and documented complete obliteration of the cystic dilatation in one case,8 partial obliteration in four1, 9, 10 and no change in the last one.6
In the other four cases,2, 6, 13 a conservative policy was adopted, with clinical and radiological follow-up (lasting over 6 years in Celli et al's report) because both the clinical and neuroradiological situation remained more or less stable. In six of the 14 cases surgically treated, the authors emphasized that the liquid that came out of the cystic lesion was clear and uncolored6, 7, 11, 12 as in normal CSF. This finding seems to support the hypothesis of a preserved turnover of the intracystic content with the CSF spaces, even though the mechanism by which this occurs remains unknown. Furthermore, the observation of a postoperative regression of the symptomatology, even when the cystic dilatation persists, adds weight to the role of a transcystic pressure gradient in the pathogenesis of dilatation of the lesion.
Conclusions
Before the advent of MRI, conus terminalis enlargement at myelography was always a reason to suspect tumor, and then surgery was performed. Now surgery is no longer mandatory to prove the diagnosis. In accordance with other reports,1, 2, 5, 6, 7, 8, 9, 13 surgical treatment of the fifth ventricle should only be taken into consideration in cases that manifest with ingravescent clinical symptoms and signs. On the other hand, if, as in the case we describe, symptoms are not only nonspecific but predominantly subjective, mild and without signs of evolution and the neuroradiological situation remains stable, the only strategy that appears correct is conservative treatment, monitoring the lesion both clinically and radiologically with periodical follow-up examinations to assess its temporal evolution.
References
Agrillo U, Tirendi MN, Nardi PV . Symptomatic cyst dilatation of V ventricle: case report and review of the literature. Eur Spine J 1997; 6: 281–283.
Celli P et al. Cyst of the medullary conus: malformative persistence of terminal ventricle or compressive dilatation? Neurosurg Rev 2002; 25: 103–106.
Coleman LT, Zimmerman RA, Rorke LB . Ventriculus terminalis of the conus medullaris: MR findings in children. Am J Neuroradiol 1995; 16: 1421–1426.
Kriss VM, Kriss TC, Babcock DS . The ventriculus terminalis of the spinal cord in the neonate: a normal variant on sonography. AJR 1995; 165: 1491–1493.
Matsubayashi R et al. Cystic dilatation of ventriculus terminalis in adults: MRI. Neuroradiology 1998; 40: 45–47.
Sigal R et al. Ventriculus terminalis of the conus medullaris: MR imaging in four patients with congenital dilatation. Am J Neuroradiol 1991; 12: 733–737.
Nassar SI, Correll JW, Housepian EM . Intramedullary cystic lesions of the conus medullaris. J Neurol Neurosurg Psychiatry 1968; 31: 106–109.
Seror P et al. Kyste syringomyélique isolé du cône terminal. La presse Médicale 1990; 19: 1590–1591.
Dullerud R, Server A, Berg-Johnsen J . MR imaging of the ventriculus terminalis of the conus medullaris. A report of two operated patients and review of the literature. Acta Radiol 2003; 44: 444–446.
Miloudi M, Olive P, Maubon A, Frerebeau Ph, Camu W . Kyste du cône médullaire simulant une maladie du motoneurone. Rev Neurol (Paris) 1998; 154: 859–861.
Korosue K et al. Cyst of the conus medullaris manifesting amyotrophic lateral sclerosis syndrome. Folya Psychiat Neurol Jpn 1981; 35: 507–510.
Stewart Jr DH, King RB, Lourie H . Surgical drainage of cyst of the conus medullaris. Report of three cases. J Neurosurg 1970; 33: 106–110.
Vazquez-Saez V, Morales-Cano MD, Torregrosa-Sala B, Flores-Ruiz JJ, Reus-Pintado M, Climent-Oltra V . Dilation of the ventriculus terminalis, an infrequent cause of lower back pain. Magnetic resonance findings. Rev Neurol 2003; 37: 641–643.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Liccardo, G., Ruggeri, F., de Cerchio, L. et al. Fifth ventricle: an unusual cystic lesion of the conus medullaris. Spinal Cord 43, 381–384 (2005). https://doi.org/10.1038/sj.sc.3101712
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101712
Keywords
This article is cited by
-
Microsurgical fenestration of idiopathic intramedullary cysts in adult patients
European Spine Journal (2015)
-
Massive cystic dilatation within a tethered filum terminale causing cauda equina compression and mimicking syringomyelia in a young adult patient
Child's Nervous System (2013)