Abstract
Objective: To raise awareness of pseudo-tumours of urinary tract, as pseudo-tumours represent benign mass lesions simulating malignant neoplasms. Accurate diagnosis helps to avoid unnecessary surgery in spinal cord injury patients.
Setting: Regional Spinal Injuries Centre, Southport, UK
Case reports: Pseudo-tumour of kidney: A 58-year-old man with tetraplegia developed a right perirenal haematoma while taking warfarin; ultrasound and CT scanning showed no evidence of tumour in the right kidney. The haematoma was drained percutaneously. After 8 months, during investigation of a urine infection, ultrasound and CT scan revealed a space-occupying lesion in the mid-pole of the right kidney. CT-guided biopsy showed features suggestive of an organising haematoma; the lesion decreased in size over the next 13 months, thus supporting the diagnosis. Pseudo-tumour of urinary bladder: A frail, 34-year-old woman, who had spina bifida, marked spinal curvature and pelvic tilt, had been managing her neuropathic bladder with pads. She had recurrent vesical calculi and renal calculi. CT scan was performed, as CT would be the better means of evaluating the urinary tract in this patient with severe spinal deformity. CT scan showed a filling defect in the base of the bladder, and ultrasound revealed a sessile space-occupying lesion arising from the left bladder wall posteriorly. Flexible and, later, rigid cystoscopy and biopsy demonstrated necrotic slough and debris but no tumour. Ultrasound scan after 2 weeks showed a similar lesion, but ultrasound-guided biopsy was normal with nothing to explain the ultrasound appearances. A follow-up ultrasound scan about 7 weeks later again showed an echogenic mass, but the echogenic mass was seen to move from the left to the right side of the bladder on turning the patient, always maintaining a dependent position. The echogenic bladder mass thus represented a collection of debris, which had accumulated as a result of chronic retention of urine and physical immobility.
Conclusion: Recognising the true, non-neoplastic nature of these lesions enabled us to avoid unnecessary surgical procedures in these patients, who were at high risk of surgical complications because of severely compromised cardiac and respiratory function.
Similar content being viewed by others
Background
Pseudo-tumours are non-neoplastic space-occupying lesions, which mimic neoplasms. We describe pseudo-tumours of the urinary tract in two patients with neuropathic bladder.
-
A spinal cord injury (SCI) patient developed a perirenal haematoma while taking warfarin and, subsequently, resolving haematoma mimicked a neoplastic lesion of the kidney.
-
A female patient with spina bifida underwent investigations when she developed urinary infection. Ultrasound scan of the urinary bladder showed a sessile space-occupying lesion, which tested our ingenuity in clinical diagnosis.
It is crucial that we diagnose neoplastic lesions of the urinary tract in patients with neuropathic bladder without delay, as classic symptoms of vesical malignancy may be absent in these patients.1 The cases, which we present here, illustrate that it is equally important that we recognise pseudo-tumours of the urinary tract when they occur, so that unnecessary surgery is avoided in this group of patients, who often have compromised cardiac and respiratory function.
Case presentation
Case 1: pseudo-tumour of kidney
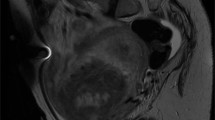
A 58-year-old man with C-4 tetraplegia developed a right perirenal haematoma, related to warfarin therapy, which was drained percutaneously. 2 After 8 months, the patient developed a fever, and urine culture grew Pseudomonas species resistant to gentamicin, ciprofloxacin, cefotaxime and ceftazidime; he was treated with colistin 1.5 million units, administered intravenously, every 8 h. Ultrasound examination of the kidneys revealed a space-occupying lesion of 5.7 cm diameter arising from the mid-pole of the right kidney (Figure 1), with no perinephric fluid collection. The left kidney was normal. CT scanning showed a 5 cm solid mass lesion involving the upper and mid-pole of the right kidney. The fat planes anterior, lateral and medial to the right kidney were well preserved, but there was a marked irregular thickening of the posterior renal fascia; it was difficult to say whether this was due to residual thickening from previous infection or due to local tumour infiltration.
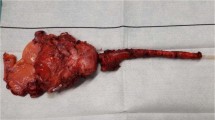
CT-guided biopsy was performed using an 18 gauge Trucut needle under local anaesthesia, with the patient lying on his left side (Figure 2); the lateral approach was preferred as a patient with C-4 tetraplegia would not be able to maintain adequate oxygenation by breathing spontaneously if lying prone.
CT scan of the upper abdomen performed during CT-guided biopsy of the mass lesion in the right kidney (04122002): the tip of the Trucut needle was located within the space-occupying lesion. The patient was lying on his left side for the biopsy. The lateral approach was preferable to the prone position for CT-guided biopsy, as this patient with C-4 tetraplegia would not be able to maintain adequate oxygenation on spontaneous breathing, if he were to lie on his stomach
Histology showed variably cellular connective tissue with focally prominent haemosiderin deposition. Some fibroblast nuclei were rather plump, resembling those seen in granulation tissue, but there was no mitotic activity or true nuclear atypia. The cellular areas alternated with thickened, hyaline collagen bundles. There was mild to moderate chronic inflammation, including a population of plasma cells. There was no evidence of neoplasia (Figure 3). The histological differential diagnosis was of organising granulation tissue or an organising haematoma.
This patient has been doing well. Ultrasound scan was performed 3 months later and the scan showed some decrease in size of the space-occupying lesion since the last examination. The lesion now measured 3.4 × 3.3 × 2.9 cm3 (Figure 4). A follow-up scan was performed 10 months later. This ultrasound scan showed a normal left kidney. The right kidney was smaller in size, with some loss of cortical thickness at the upper and lower poles. Infolded cortex in the mid-pole of the right kidney was giving the effect of a space-occupying lesion. This measured 2 cm in diameter and was smaller than the previous examination. The final diagnosis was a pseudo-tumour of the right kidney. There was no evidence of malignancy in the right kidney.
Follow-up ultrasound scans of the right kidney (18022003): a decrease in the size of the space-occupying lesion can be appreciated when compared with the ultrasound scan performed 3 months ago (Figure 1)
Case 2: pseudo-tumour of urinary bladder
This female patient (born in 1968) with spina bifida, paraplegia and marked spinal and pelvic curvature had been managing her neuropathic bladder with an indwelling urethral catheter and pads. In 1995, she underwent suprapubic cystolithotomy. In 1996, she developed urinary infection. CT confirmed a large right pyonephrosis with obstruction at the pelviureteric junction by a large calculus. CT-guided nephrostomy was done. Subsequently, right pyelolithotomy was performed. In 1998, stones were detected in the urinary bladder. The stones were crushed and removed endoscopically. There was recurrence of vesical calculi a year later and electrohydraulic lithotripsy of bladder stones was carried out. In January 2002, there was recurrence of bladder stones. Cystoscopy was performed; stones were crushed and removed fully. In November 2002, ultrasound of the abdomen was performed because she had been getting recurrent urinary infections. It showed staghorn calculus in the left kidney and there was moderate hydronephrosis. The urine looked clear. The right kidney was not seen due to scoliosis. The radiologist recommended CT scan, as CT would be the better means of evaluating the urinary tract in this patient with severe spinal deformity.
A CT scan of the abdomen was carried out in December 2002 before and after injection of intravenous contrast. The right kidney was small and hydronephrotic with staghorn-type calculi in the renal pelvis and lower pole calyces. The left kidney was large and mildly hydronephrotic with calculi in the renal pelvis and lower pole. There was marked distortion of anatomy by the patient's severe scoliosis. Both kidneys were functioning, with contrast opacifying the pelvicalyceal systems. Bladder calculi were not present, but there was a filling defect in the bottom of the bladder (Figure 5), which raised the possibility of a bladder neoplasm. Ultrasound of the bladder was therefore performed, which showed a sessile space-occupying lesion measuring 5.2 × 3.6 × 1.2 cm3 in the left bladder wall posteriorly. There was no evidence of extravesical invasion (Figure 6).
Because of the ultrasound appearances, flexible cystoscopy was performed on the same day. Cystoscopy showed necrotic slough and debris in the bladder, but no tumour was visible. Biopsies were taken, and histology revealed nonkeratinising squamous epithelium with moderately inflamed underlying stroma and pieces of inflammatory slough (Figure 7).
Since flexible cystoscopy and biopsy did not reveal any neoplastic lesion, cystoscopy was performed under anaesthesia about 3 weeks later. No tumour was found. Biopsies of bladder mucosa were taken from the dome, right and left lateral walls, posterior wall and bladder base and all showed only mildly inflamed mucosa with no evidence of dysplasia or malignancy. The patient was catheterised for 48 h after the cystoscopy, but subsequently reverted to the regime of using pads. After 2 weeks, a follow-up ultrasound scan of urinary bladder revealed a space-occupying lesion in the left side of the bladder, with no significant interval change since the last scan. Ultrasound-guided biopsy of the lesion was therefore performed using a 20 gauge Trucut needle; neither anaesthesia nor sedation were needed. This biopsy showed a normal full thickness bladder wall, lined by glycogenated, nonkeratinising, squamous, epithelium; there was no evidence of keratinising squamous metaplasia, dysplasia or malignancy (Figure 8). There was nothing histologically to explain the ultrasound appearances of a bladder mass.
A follow-up bladder ultrasound scan was performed about 7 weeks later with the patient lying supine, and yet again showed a space-occupying lesion in the left side of the bladder. However, on turning the patient onto her right side, the echogenic mass moved from the left side of the bladder to the right, the lesion maintaining the most dependent position in the bladder (Figure 9). Colour flow Doppler showed no blood flow within the lesion. These findings confirmed that the mass identified on ultrasound merely represented a collection of debris in the most dependent part of the bladder.
Discussion
Pseudo-tumours of the kidney can be due to a surprising variety of underlying conditions, including:
-
Infolding of the columns of Bertin.3
-
Specific infections such as uro-genital tuberculosis.4
-
Renal involvement in primary Sjogren's syndrome.5
-
Migration of an accessory spleen into the site of the cuneiform nephrectomy.6
-
Packing of an operative renal defect with retroperitoneal fat.7
-
Haematomas arising in the context of severe haemophilia A or B or von Willebrand disease.8
-
Local hypertrophy secondary to infectious, vascular, or traumatic lesions.9
In patient number 1, organised haematoma and infolded cortex in the mid-pole of the kidney simulated a space-occupying lesion.
In patient number 2, intravesical urinary debris resembled closely a bladder neoplasm. During real-time ultrasound scanning of the urinary bladder in this patient with spina bifida and marked pelvic tilt, changes in the position of the echogenic mass were observed as the patient was turned from one side to the other. This provided a vital clue that the mass in the bladder represented debris, which had accumulated in the most dependent part of the bladder. This patient was very frail, and during the daytime was confined to her reclining wheelchair in which she would be propped up with her legs straight, as she could not bend her knees. She was unable to perform transfers from the chair or from the bed, and could not turn herself. By wearing pads and allowing spontaneous passage of urine, she was not emptying her bladder completely. A combination of three predisposing factors, namely chronic retention of urine, physical immobility and urinary infection, led to a quite and rapid build-up of debris in the bladder.
We learned from this patient that spinal cord injury patients, who are at high risk for developing debris in the bladder, should undergo ultrasound scans of the bladder in different positions to detect the movement of any echogenic mass. Performing ultrasound scans of the bladder in both supine and lateral positions is analogous to the dictum that kidney scans should be performed in supine and sitting positions if milk of calcium is suspected. Repeating the scan after a thorough bladder washout would also help to distinguish between bladder neoplasms and mere debris.
Conclusion
Patients with neuropathic bladder may develop unusual lesions in the kidneys or bladder, and these patients require detailed investigations to distinguish between true neoplasms and pseudo-tumours, as observed in the two patients described in this report. Recognising the true, non-neoplastic nature of these lesions enabled us to avoid unnecessary surgical procedures in these patients, who were at high risk of surgical complications because of severely compromised cardiac and respiratory function.
References
Vaidyanathan S et al. Problems in early diagnosis of bladder cancer in a spinal cord injury patient: Report of a case of simultaneous production of granulocyte colony stimulating factor and parathyroid hormone-related protein by squamous cell carcinoma of urinary bladder. BMC Urol 2002; 2(1): 8.
Vaidyanathan S et al. How should an infected perinephric haematoma be drained in a tetraplegic patient with baclofen pump implanted in the abdominal wall? – A case report. BMC Urol 2002; 2: 9.
Carty AT, Short MD, O'Connell ME . The diagnosis of renal pseudotumours. Br J Urol 1975; 47: 495–498.
Verswijvel G et al. Renal macronodular tuberculoma: CT and MR findings in an asymptomatic patient. http://www.rbrs.org/journal/volume85_4/verswij.html.
Oyen RH, Vandercruysse D, Baert A . Case report: renal involvement in primary Sjogren syndrome – a rare cause of renal pseudotumour. Clin Radiol 1995; 50: 271–273.
Sy M et al. Case report: renal pseudotumours mimicking tumour recurrence after partial nephrectomy. Br J Radiol 1996; 69: 359–362.
Millward SF, Lanctin HP, Lewandowski BJ, Lum PA . Fat-filled postoperative renal pseudotumour: variable appearance in ultrasonography images. Can Assoc Radiol J 1992; 43: 116–119.
Eby CS, Caracioni AA, Badar S, Joist JH . Massive retroperitoneal pseudotumour in a patient with type 3 von Willebrand disease. Haemophilia 2002; 8: 136–141.
Zeman RK et al. Computed tomography of renal masses: pitfalls and anatomic variants. Radiographics 1986; 6: 351–372.
Author information
Authors and Affiliations
Additional information
This article is dedicated to the memory of Mr John Ashcroft, who was a patient of Regional Spinal Injuries Centre, Southport.
Rights and permissions
About this article
Cite this article
Vaidyanathan, S., Hughes, P., Mansour, P. et al. Pseudo-tumours of the urinary tract in patients with spinal cord injury/spina bifida. Spinal Cord 42, 308–312 (2004). https://doi.org/10.1038/sj.sc.3101594
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101594