Abstract
Study design: Report of a case of subarachnoid hematoma associated with neurofibromatosis type 2 (NF2) in a 10-year-old girl.
Objective: To report a rare case of subarachnoid spontaneous hematoma associated with NF2, with no evidence of trauma.
Setting: Gifu, Japan.
Methods: The patient presented with severe leg pain. MRI revealed a subarachnoid hematoma at the level of L2 and a spinal cord tumor at the level of T6. The subarachnoid hematoma had low and high heterogeneous signal intensity on the T1-weighted image and low signal intensity on the T2-weighted image, indicating the presence of extracellular methemoglobin. The tumor and hematoma were resected.
Results: Pathological analysis demonstrated that the surgical specimen removed from the area of L2 was a hematoma and the specimen from T6 was a neurinoma. At follow-up 1 year after surgery, the girl remained neurologically asymptomatic.
Conclusions: This rare case of spinal subarachnoid hematoma was associated with NF2. MRI was useful in establishing the diagnosis.
Similar content being viewed by others
Introduction
Spinal subarachnoid hematomas are relatively rare in clinical practice, although several cases have been reported in the literature.1,2,3,4 We report a case of subarachnoid hematoma associated with neurofibromatosis type 2 (NF2) in a 10-year-old girl. To our knowledge, this combination has not been reported previously.
Case report
In December 2000, a 10-year-old girl with a 3-month history of severe pain in the right leg was admitted to our department. When she first experienced the pain in the right leg, it was mild, but within a few days, it suddenly became severe. She had no history of trauma to the spine nor of excessive exertion. Her relevant medical history began in 1995, when she noticed hearing loss in her right ear, found to be due to an acoustic tumor, which was successfully resected. In 1997, at the age of 7 years, multiple tumors were detected in her mediastinum, brain, and spinal cord. She was diagnosed with NF2. In 1998, at the age of 8 years she underwent gamma knife radiosurgery for the brain tumor and resection of the mediastinal tumor.
On admission, the patient had no motor weakness or loss of sensation in her lower extremities and her bowel and bladder functions were intact. She had no coagulation defects and was not on anticoagulant therapy. She had neurofibromas on her trunk and extremities. Her only complaint was of severe pain in her right leg.
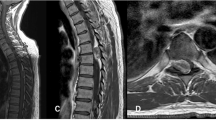
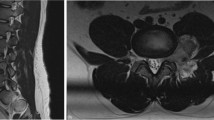
An MRI scan showed a dumbbell-shaped tumor at the level of T6 (Figure 1a) with low signal intensity on the T1-weighted image (Figure 1b) and high signal intensity on the T2-weighted image (Figure 1c). Gadolinium enhancement of the tumor was positive. Furthermore, in the spinal canal, there were masses at the L2 and L4–5 levels (Figure 2a). The mass at the level of L2 had a combination of low and high signal intensity on the T1-weighted image (Figure 2b) and low signal intensity on the T2-weighted image (Figure 2c). Gadolinium enhancement was positive. The mass at the level of L4–5 appeared to be a neurinoma associated with the NF2. We performed myelography by lumbar puncture at the level of L5–S1 with 5 ml of Iohexol. As a total block was noted at the L2 level, suboccipital puncture was added (Figure 3). The myelogram showed not only the hematoma at the level of L2 and the tumor at the level of L4–5, but also numerous small masses in the dural sac, presumably small tumors. The patient complained of urinary retention and weakness in her lower extremities, 6 h after the myelography. We performed a double surgical decompression of T6 and L2. As the cauda equina was unlikely to be suffering severe compression from the tumor at the level of L4–5, we did not plan to resect this tumor at the time of surgery.
(a–c) Preoperative MRI of the lumbar spine (a: T2-weighted sagittal section; b: T1-weighted axial section; c: T2-weighted axial section). An intradural subarachnoidal hematoma at the level of L2 (a: white arrow) and a spinal cord tumor (a: black arrow) are visible. The hematoma appeared as a heterogeneous mass on the T1-weighted image, and as low signal intensity on the T2-weighted image, indicating that the contents were extracellular methemoglobin, ferritin, and hemosiderin
Surgical procedures
At surgery, we first resected the dumbbell-shaped tumor at the level of T6, which appeared to be a neurinoma. Second, we performed a laminectomy, preserving two-thirds of intervertebral facet joint, between L1 and L2 vertebrae. The dura was incised, and a dark-blue arachnoidea was revealed. When it was opened, a hematoma was exposed in the subarachnoid space (Figure 4). Around the hematoma there was no evidence of AVM or of ruptured major vessels. However, as is usually the case with NF2, numerous small tumors, probably neurofibromas, were present in the area of the cauda equina. Considering the frequent recurrence of such tumors in the natural course of NF2, we did not perform extensive excision of these small tumors.
On histological examination, the surgical specimen from T6 was determined to be a neurinoma. The specimen from L2 showed only evidence of clotted blood and no evidence of neoplasia or AVM. The patient's postoperative course was uneventful. At 2 years follow-up, she remains neurologically asymptomatic.
Discussion
Intraspinal hematomas are relatively rarely encountered in clinical practice.1,2,3,4 Depending on their location, they are classified as epidural, subdural,5,6,7,8 subarachnoid,1,2,3,4 or intramedullary. Spinal subarachnoid hematoma is rare. It has been stated that hemorrhage may originate solely within the subarachnoid space.3,8 One reason for the rarity of spinal subarachnoid hematoma is that usually the diluting and redistributing effect of cerebrospinal fluid (CSF) prevents subarachnoid blood from clotting and from forming a solid hematoma in this space.1,4,8 With most bleeding into the CSF, the composition of the fluid and the pulsatility of the vessels make it difficult for the blood to coagulate. However, if the bleeding is sufficiently massive or rapid to cause blockage of normal CSF flow, then stasis will occur and a clot will form.3,5,9 The question arises as to what is the cause of spinal hematoma formation. Russell et al,4 stated that spinal subarachnoidal hematoma may arise without obvious course,1,2 or it may be caused by a ruptured vascular malformation, a blood dyscrasia, or anticoagulant therapy.3 These hematomas have been reported to follow both major and minor10 spinal trauma. Swann8 reported that spinal tumors, especially in the region of the cauda equina and conus medullaris, can cause spontaneous spinal subarachnoid hemorrhage, although this occurrence is uncommon. Ependymoma,9 neurofibroma,9,11 meningioma, cavernous hemangioma, hemangioblastoma, astrocytoma, schwannoma, and meningiosarcoma have been reported.8,9 The mechanism of hematoma formation is believed to be related to the vulnerability to trauma of the blood vessels surrounding these tumors.7 A combination of spontaneous hematoma in the spinal canal, neurinoma, and NF2 was reported by Smith as a case of subdural hematoma with intact arachnoidea. However, in a search of the literature (in English), we found only one record of spinal subarachnoid hematoma associated with NF2. In our patient there was no evidence of bleeding from the neurinoma in the thoracic area. Therefore, one possible cause of the subarachnoid hematoma would have been spontaneous bleeding from the multiple small tumors associated with NF2 and located around the cauda equina.
On MRI, the signal intensity of hematomas changes with the biochemical status of the heme iron. Several days after the formation of a hematoma, extracellular methemoglobin appears as an extremely high signal intensity on the T1-weighted image and an extremely low signal on T2.6 At the same time, ferritin and hemosiderin appear as moderate or low signals on the T1-weighted image and extremely low signals on T2.1,6 In our patient, the outline of the hematoma showed high signal intensity on the T1-weighted image and low signal intensity on T2. Theoretically, this indicated the presence of extracellular methemoglobin. However, the center of the hematoma was low on both the T1- and T2-weighted images, indicating the presence of ferritin and hemosiderin. Therefore, we considered that the hematoma was old, not fresh. Thus, preoperative MRI provided us with useful information for making a correct diagnosis and establishing an appropriate surgical plan.
Conclusion
We report a rare case of spinal subarachnoid hematoma associated with NF2.
References
Cabrera MA . Follow up of a spontaneous ventral subarachnoid spinal haematoma by means of magnetic resonance. Rev Neurol 2001; 32: 1137–1140.
Owaki K . Spontaneous spinal subarachnoidal hematoma – case report (author's transl). No Shinkei Geka 1975; 7: 593–597 (in Japanese).
Rengachary SS . Subarachnoid hematoma following lumbar puncture causing compression of the cauda equina: case report. J Neurosurg 1974; 41: 252–254.
Russell NA . Acute spinal cord compression by subarachnoid and subdural hematomas occurring in association with brachial plexus avulsion. J Neurosurg 1980; 52: 410–413.
Calhoun JM . Spontanous spinal subdural hematoma: case report and review of the literature. Neurosurgery 1991; 29: 133–134.
Kullarni AV . Serial magnetic resonance imaging findings for a spontaneously resolving spinal hematoma: case report. Neurosurgery 1998; 42: 398–400.
Smith RA . Spinal subdural hematoma, neurilemmoma, and acute transverse myelopathy. Surg Neurol 1985; 23: 367–370.
Swann KW . Spontaneous spinal subarachnoid hemorrhage and subdural hematoma: report of two case. J Neurosurg 1984; 61: 975–980.
Djindjian M . Subarachnoid hemorrhage due to intraspinal tumors. Surg Neurol 1978; 9: 223–229.
Bouzarth WF . Delayed traumatic spinal subarachnoid hemmorrhage. JAMA 1968; 205: 880–881.
Prieto Jr A . Spinal subarachnoid hemorrhage associated with neurofibroma of the cauda equina. J Neurosurg 1967; 27: 63–69.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Inoue, T., Miyamoto, K., Kushima, Y. et al. Spinal subarachnoid hematoma compressing the conus medullaris and associated with neurofibromatosis type 2. Spinal Cord 41, 649–652 (2003). https://doi.org/10.1038/sj.sc.3101496
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101496