Abstract
Study design: Out of a population of 456 patients with spinal cord injuries (SCI), 130 having pain were selected after matching, based on gender, age, American Spinal Injury Association (ASIA) impairment grade and level of lesion.
Objective: To investigate whether gender differences with regard to pain perception and prevalence exist in a population of patients following spinal cord injury.
Setting: Spinalis SCI Unit (out-patient clinic), Stockholm, Sweden.
Method: 130 patients suffering from pain were assessed over a 12-month period in a yearly health control.
Results: SCI women had a higher prevalence of nociceptive pain than men and their use of analgesics was greater. However, no differences between the sexes could be seen regarding pain and localization, onset, distribution, factors affecting pain, number of painful body regions, pain descriptors, ratings of pain intensities or in pain and life satisfaction.
Conclusion: This study showed that SCI men and women describe their pain very similarly. However, SCI women had a higher prevalence of nociceptive pain than men and their use of opiates and non-steroid anti-inflammatory drugs (NSAIDs) was greater.
Similar content being viewed by others
Introduction
Pain is described by spinal cord injured (SCI) patients as the worst problem,1 far more disabling than the loss of motor and sensory function. Reports of pain prevalence differ between 34 and 94%,2,3,4,5,6 but it is most often described as present in around 60–65% of the SCI populations.2,7,8,9,10,11 This variability may depend on the population assessed, the type of survey12 but also on the definition of pain.12 Several studies have described pain prevalence, risk-factors, pain and medical variables and psychosocial scores in SCI populations,2,3,4,5,6,8,9,10,11,12 but since results vary from study to study there is no consensus. Pain seems to have an early onset after the injury,2,3,4,6,10 is reported mainly from below or at the level of the lesion,2,5,6,10 and is mostly classified as neurogenic/neuropathic.1,10,13 (The term neurogenic will be used throughout this paper). According to Ravenscroft and colleagues4 a higher incidence of pain is seen in patients with complete injuries. However, others have reported a higher incidence in those with incomplete lesions6,8,10 and this has been supported by autopsy findings,14 further supported by the finding that patients with incomplete lesions have more severe pain than those with complete lesions.13
Age has previously been reported to influence the vulnerability to pain.15,16 Störmer2 found a significant difference between age at injury and the presence of pain in SCI patients. Patients who had sustained their injury when young were less at risk of developing chronic pain. Demirel8 also found that SCI patients with continuing pain were older than those who were pain free.
In the non-spinal cord injured population, gender differences in pain perception and pain prevalence are often discussed. Several nociceptive pain conditions, for example migraine headaches, orofacial pain, fibromyalgia, abdominal pain and pelvic pain, are more common in women,17 as are some neurogenic pain conditions, such as reflex sympathetic dystrophy and post-herpetic neuralgia.17 Women also report greater severity and frequency of perceived pain than do men. Furthermore, women's pain is reported as longer lasting and present in a greater number of body regions compared to men's.18,19,20
Often, epidemiological studies of spinal cord injured patients do not address gender differences.4,5,8 In a study by Störmer and colleagues2 a tendency towards a higher prevalence of pain could be seen in women, even though this was not significant. However, Finnerup and colleagues6 reported significantly higher pain prevalence in men.
Objective
The aim of this study was to investigate whether gender differences regarding pain prevalence, the number of painful body regions, pain intensities, localization, onset, distribution, factors influencing pain, pain descriptors, pain quality, use of analgesics and pain and life satisfaction exist in a population of patients with SCI.
Methods and patients
Within the Spinalis SCI unit, an out-patient clinic, yearly health examinations are offered to all patients registered, ie those with a sustained spinal cord injury or with myelomeningocele. All patients are assessed by a physician, a physiotherapist, an occupational therapist, a nurse and a social worker, according to a standardized manual, The Spinal Injury Registry of Sweden (RYSS)21. These assessments are made in an out-patient setting and take 3–4 h. At the time of the study, the RYSS instrument was used in all Spinal Cord Injury Units in Sweden (n=6) in co-operation with regional hospitals with SCI care. Today this instrument is used nationwide in both Norway and Sweden and therefore has been re-named as the Nordic Spinal Cord Injury Registry. In addition to the assessment by the RYSS instrument, an additional pain questionnaire was filled in by the patient, in the presence of the assessing physician. This questionnaire included drawing a pain chart, describing pain character/s (including dysesthesia), the localization of pain, the number of painful body regions and the scoring of pain intensities. The scoring consisted of rating the ‘mildest’, the ‘general’ and the ‘worst’ intensity of all identified pain areas on a visual analogue scale (VAS), reading from 0 to 100 and marked at the ends with ‘no pain’ and ‘unbearable pain’.
The condition was defined as pain, ache or unpleasantness present at least for the last two weeks or recurrent during at least four 2-week periods during the last year.21 The grading of the severity of the spinal cord injury was based on the American Spinal Injury Association's (ASIA) impairment scale, grading the injury from ASIA A (no motor or sensory function in the sacral segments S4–S5) to ASIA E (motor and sensory function are normal).22
The study was approved by the ethical committee of the Karolinska Institutet in Stockholm, Sweden.
Subjects
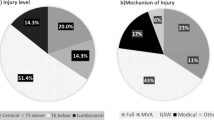
During a 12 month period, all patients with a spinal cord injury who came for a yearly check-up were asked to participate in the study. Out of the population of 603 patients, 456 accepted the offer of a health control during this period of time and also agreed to participate in the study. Of the 456 patients, 340 (74.6%) had a traumatic injury and 116 (25.4%) a non-traumatic injury, 120 (26.3%) were females and 336 (73.7%) males. Mean age overall was 47.04 years, range 11–84. Mean age for females was 48.7 years, and for males 46.5 years.
Since gender, age and completeness of lesion can influence the perception of pain, we aimed at matching all females (n=89) with pain from the original sample of 456 patients, to males for age (±3 years), ASIA grade and level of lesion (cervical, thoracic, lumbar/sacral) in order to detect gender differences. Sixty-five of these 89 women were successfully matched to a corresponding male, resulting in two groups of 65 patients each, with a mean age of 49.88 years (women 49.73 and men 50.04 years).
Statistics
Age at injury was demonstrated as mean values±standard deviation and tested with T-test for independent samples to evaluate differences between patients who developed lasting pain and those who did not. The different distribution of number of pain-locations between the sexes was evaluated with Fisher two-tailed exact test. The distribution of observed frequencies of nominal data was analyzed with the non-parametric Chi-square test with 1 degree of freedom throughout except for life satisfaction and sex differences in number of consumed pharmacological interventions where the non-parametric two-sample test Mann–Whitney U-test was used. The level of significance was set to 0.05.
Results
Prevalence of pain in the non-matched population consisting of 456 individuals
In this study10 456 patients were assessed regarding perception of pain and its prevalence. Gender differences were found significant in the analysis of pain prevalence. Of the women 74.2% (n=89) reported pain compared to 60.1% of the men (n=202), P=0.007. When split into age categories, pain was seen to increase with age, and was most prevalent in women in the age group 50–59 years (P=0.028), after which it declined. Men's pain prevalence showed the same pattern but without the peak in the middle aged group (Figure 1). Patients with pain were of a significantly higher mean age (35.1 years, SD±16.24) at injury than those without (31.4 years, SD±18.05), P=0.027. In our study we also found a higher prevalence of pain in ASIA D classified patients, P=0.044.
No correlations were found in this study regarding pain and etiology of injury (traumatic/nontraumatic), pain and time since injury, pain and level of lesion, pain and spasticity or in pain and contractures.
Results in the group consisting of 130 matched individuals
Onset of pain
Most patients experienced pain within 3 months of their spinal cord injury. In 15 women and 25 men pain commenced more than 12 months after the injury, P=0.057 (Table 1).
Localization of pain
Pain was experienced at the lesion level by 17 women and 21 men, and below it by 46 women and 47 men, ie in areas with decreased or no sensitivity. In 17 women and 21 men, pain was localized to areas above the level of injury, ie in areas with normal sensation (Table 1).
Pain distribution
The patients were classified as having a diffuse distribution of pain (37 women and men), pain localized to a smaller area (22 women and 26 men) and segmental pain in one or more dermatomes (17 women and 20 men) (Table 1).
Factors affecting the perception of pain
Around half of the women and men reported that mechanical factors influenced their pain. The same number of persons reported pain being unaffected by any observed factors (Table 1).
Number of painful body regions
All patients were asked to describe how many different body areas (1–5) they could identify as painful (Table 2). On average women had 1.60 painful sites and men 1.72.
Scoring of pain intensities
To assess the pain intensity, the ‘mildest’ pain, ‘general’ pain and ‘worst’ pain was rated for each located area on a VAS score. The median value for the mildest pain was 25 for both sexes, the general pain 48 in women and 46 in men, and the worst pain was rated 78 in women and 76 in men.
Pain descriptors
Pain descriptors could be chosen from a given list with possibilities to use one's own expressions as well. Aching pain was the most commonly used descriptor in both men (47.4%, n=31) and women (43.1%, n=28). In women burning pain was reported by 22 (33.8%) compared with 16 men (24.6%). Seventeen men (26.1%) reported pricking pain compared to 12 women (18.5%) (Table 1).
Disturbance of daily life
Employing the RYSS instrument, patients were asked the extent to which pain disturbed their daily life, using the categories,21 not at all; to some extent; a lot. Most patients were disturbed by their pain to some extent (30 women and 30 men) or a lot (19 women and 24 men) (Table 1).
Life satisfaction
Life satisfaction was assessed with the Fugl–Meyer Life Satisfaction instrument.23 The instrument contains nine questions and is self-rated, scoring from 1 (very dissatisfying) to 6 (very satisfying). One-third of the women (n=22) and half of the men (n=36) completed this questionnaire (Figure 2). There were no significant differences between the sexes but a tendency by women to rate family life higher than men could be identified, P=0.056.
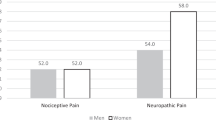
Pain quality
The types of pain were classified by the assessing physician into one of three different pain categories; neurogenic pain, nociceptive pain or mixed pain (ie presence of both neurogenic and nociceptive pain).21,24 Women were classified as suffering more often than men from nociceptive pain, P=0.041 (Table 1).
Use of pain relieving medication
Fifty-three of the 130 patients (40.8%) used one or more pain relieving drugs. Mean value for the number of drugs used was 0.82 in women and 0.37 in men, P=0.0025. Significantly more women (53.8%) than men used pain medication (27.7%), P=0.0024. Major gender differences were also seen when looking at the varied choice of drugs (Table 2). Women used opiates (P=0.0187) and non-steroid anti-inflammatory drugs (NSAIDs) and other peripherally acting drugs (P=0.0002) to a much larger extent than men. Their consumption of NSAIDs was five times more common (32.3%) than men's (6.2%) and their use of opiates twice as common (36.9%) compared to men (18.5%). The use of anti-epileptic medication was very low in both sexes with only five men and one woman using this type of drug. Similarly only seven women and four men used anti-depressives as analgesics (Table 1).
Discussion
In this study we found a higher prevalence of nociceptive pain in SCI women than in SCI men. SCI women also had higher consumption of opiates and NSAIDs. However, there were no differences with regard to onset of pain, pain descriptors, number of affected body regions, factors influencing pain, rating of pain intensities and life satisfaction in this age-, gender-, level of lesion- and completeness of lesion matched population of SCI patients.
We were unable to detect any gender differences regarding pain and life satisfaction, but the amount of responders was very low, only one-third of the women and half of the men had completed the questionnaire, making it difficult to draw conclusions from this material. In our study ‘aching pain’ was the most commonly used word descriptor, the same as in two studies by Turner and colleagues.5,9 This contrasts with others who have reported burning pain,2 pricking and tingling pain6 as the most frequently used words. The descriptor ‘aching pain’ was in our study used by more men than women and ‘burning pain’ by more women than men, even though these differences were not significant. However, a recent study has investigated the use of pain descriptors when classifying SCI pain and concluded that verbal descriptors alone are not sufficient for pain classification.25
In non-SCI populations, women often report more numerous pain locations than men17,19 and more severe pain.18 This was not the case in our study, where no differences were found. But the greater prevalence of pain in women in our population of 456 individuals is supported by epidemiological studies of gender differences in general.17,20 The underlying reasons are largely unknown. Several studies emphasize that no difference in sensitivity is apparent sex-wise in pain thresholds tested pre-pubertally, while a significant increase is noted in women post-pubertally.26,27 This could come about through increased levels of gonadal hormones3,19,28,29,30 The increased pain prevalence seen in this study amongst women aged between 50 and 59 years could possibly be explained by fluctuating menopausal hormone levels. Differences in body composition (women have a higher percent of body fat and smaller muscle mass) could be a contributing factor, and could have importance in eg musculo-skeletal conditions.28 Size, eg height and body surface, is less likely to contribute.27,31 Another reason why women appear to exhibit greater and more frequent pain could be that it is habitually more socially acceptable. It is possible that men and women differ in their acknowledgement of pain as well as in evaluating and interpreting bodily discomfort.20,32 This is supported by Canli and colleagues33 showing that women have better emotional memory than men.
In other patient groups women and men describe symptoms and signs of various pain disorders in different ways, eg in coronary diseases.32 This has led to differences in aggressiveness in treating the disease. Different ways of expressing pain might have an impact on the choice of pharmacologial treatment, but in our study the differences in choice of analgesics cannot be explained thus, since men and women described their pain very similarly. In the extensive review by Unruh in 199618 she declares that no evidence for gender differences in the amounts of analgesics used has been found in non-SCI populations, but our findings were in contrast to this. 53.8% of the women used one or more pain relieving drug compared to 27.7% of the men. NSAIDs and other peripherally acting drugs were more commonly used by women (32.3 vs 6.2%), as were opiates (36.9 vs 18.5%). The small use of anti-depressive and anti-epileptic drugs was surprising, although this was also noted in a recent Danish study.6 10.8% of the women used anti-depressive medication for analgesia compared to 6.25 of the men, and only 1.5% of the women and 7.7% of the men used antiepileptic drugs. In our study neurogenic pain was the most frequently diagnosed type of pain in both men and women. But as many as 20 women and 10 men were being classified as suffering from nociceptive pain, mixed pain unregarded. In this respect women seem to be classified as suffering more often from nociceptive pain than men. But why this increased prevalence of pain in SCI women is restricted to nociceptive pain alone and does not include neurogenic pain we are unable to explain. No gender differences could be detected in the classification of mixed or neurogenic pain or in onset, distribution, localization, pain descriptors and factors influencing pain. Still the use of opiates and NSAIDs differed significantly between the sexes and we found this hard to explain simply by the greater incidence of nociceptive pain in women alone. The reason behind the women's greater use of analgesics could not be explained either by age, level of lesion or completeness of lesion since the patients in this study were matched in these.
Pain in patients with SCI can be of both neurogenic and nociceptive quality. The ‘golden standard’ in treating pain is by use of NSAIDs and opiates for nociceptive pain and anti-depressive or anti-epileptic drugs for neurogenic pain. Some study results, however, show effects from opiates given intrathecally or in i.v. infusions.34 According to a review in Pain Clinical updates34 effectiveness in treating neurogenic pain orally has been achieved in the use of anti-depressants, anti-convulsants and NMDA (N-methyl-D-aspartate)-receptor antagonists. Unfortunately, there are few studies that have assessed, in a randomized controlled way, the effect of both pharmacological and non-pharmacological treatments of neurogenic pain.
Nothing in this study can totally explain the gender differences found in the diverse use of analgesics. There are studies showing gender differences in the responses to both physical and pharmacological treatment, especially to opiates but also to transcutaneous electric nerve stimulation (TENS). Women seem to respond better to κ-mediated and men to μ-mediated treatment.14,35,36,37,38 Since most traditional opiates used today work mainly on the μ-receptors, opiates are likely to be less effective in women and therefore less used in their treatment. No studies (to our knowledge) have assessed possible gender differences in the effects of treatment with anti-epileptic or anti-depressive drugs, but it would be interesting to investigate if this partly accounts for the differences found in this study.
Conclusion
In our study population we found that: (1) SCI women have a higher prevalence of nociceptive pain than men; (2) SCI men and women perceive and describe their pain similarly regarding the number of painful body regions, pain intensitities, localization, onset, distribution, factors influencing pain and life satisfaction; and (3) SCI women use more analgesics than men, i.e. opiates and NSAIDs.
Differences shown in this study and many others are of interest, not only for identifying the patients at risk of developing chronic pain but also for choosing the optimal treatment. The assessment of the patients' clinical pain is of great importance since this may lead to different treatment strategies. Gender differences in the perception of different drugs' effect raise another important issue that needs further addressing.
References
Levi R, Hultling C & Seiger Å . The Stockholm spinal cord injury study: 1. Medical problems in a regional SCI population. Paraplegia 1995; 33: 308–315.
Störmer S et al. Chronic pain/dysethesiae in spinal cord injury patients: results of a multicenter study. Spinal Cord 1997; 35: 446–455.
Siddall PJ et al. Pain report and the relationship of pain to physical factors in the first 6 months following spinal cord injury. Pain 1999; 81: 187–197.
Ravenscroft A, Ahmed YS & Burnside IG . Chronic pain after SCI. A patient survey. Spinal Cord 2000; 38: 611–614.
Turner JA, Cardenas DD, Warms CA & McClellan CB . Chronic pain associated with spinal cord injuries: a community survey. Arch Phys Med Rehabil 2001; 82: 501–508.
Finnerup NB et al. Pain and dysesthesia in patients with spinal cord injury: A postal survey. Spinal Cord 2001; 39: 256–262.
Siddall PJ & Loeser JD . Pain following spinal cord injury. Spinal Cord 2001; 38: 63–73.
Demirel G, Yllmaz H, Gencosmanoglu B & Kesiktas N . Pain following spinal cord injury. Spinal Cord 1998; 36: 25–28.
Turner JA & Cardenas DD . Chronic pain problems in individuals with spinal cord injuries. Semin Clin Neuropsychiatry 1999; 4: 186–194.
Norrbrink Budh C et al. Pain in a Swedish Spinal Cord Injury Population. Clinical Rehabilitation 2002; in press
Rintala DH et al. Chronic pain in a community-based sample of men with spinal cord injury: prevalence, severity, and relationship with impairment, disability, handicap, and subjective well-being. Arch Phys Med Rehabil 1998; 79: 604–614.
Siddall PJ, Yezierski RP & Loeser JD . Taxonomy and epidemiology of spinal cord injury pain. In: Yezierski RP, Burchiel KJ (eds). Spinal Cord Injury Pain: assessment, mechanisms, management. Progress in Pain research and Management. Vol 23; Seattle: IASP Press, 2002; pp 9–24.
Cohen MJ et al. Comparing chronic pain from spinal cord injury to chronic pain of other origins. Pain 1988; 35: 57–63.
Kakulas BA et al. The neuropathology of pain and abnormal sensations in human spinal cord injury derived from the cliniopathological data base at the Royal Perth Hospital. In: Dimitrijevic MR, Wall PD, Lindblom U (eds). Altered Sensation and Pain, Recent Achievements in Restorative Neurology. Vol 3: Basel: Karger, 1990; pp 37–41.
Andersson HI, Ejlertsson G, Leden I & Rosenberg C . Chronic pain in a geographically defined general population: studies of differences in age, gender, social class, and pain localization. Clinical J Pain 1993; 9: 174–182.
Greenberger P . Women, men, and pain. J Womens Health 2001; 4: 309–310.
Meisler JG et al. Chronic pain conditions in women. J Womens Health 1999; 3: 313–320.
Unruh A . Review article – Gender variations in clinical pain experience. Pain 1996; 65: 123–167.
Berkley KJ . Sex differences in pain. Behav Brain SCI 1997; 20: 371–380.
Barsky AJ, Peekna HM & Borus JF . Somatic symptom reporting in women and men. J Gen Intern Med 2001; 16: 266–275.
Levi R & Ertzgaard P . Quality indicators in spinal cord injury care: a Swedish collaborative project. The Swedish Spinal Cord Injury Council 1998. Scand J Rehabil Med Suppl 1998; 38: 1–80.
Manual for the International Standards for Neurological and Functional Classification of Spinal Cord Injury. Illinois: American Spinal Injury Association, Chicago,, 1996;
Fugl-Meyer AR, Brännholm IB & Fugl-Meyer KS . Happiness and domain specific life satisfaction in adult northern Swedes. Clin Rehabil 1991; 5: 25–33.
Siddall PJ, Yezierski RP & Loeser JD . Pain following spinal cord injury: clinical features, prevalence and taxonomy. International Association for the Study of Pain; Newsletter 2000; 3: 3–7.
Putzke JD et al. Pain classification following spinal cord injury: The utility of verbal descriptors. Spinal Cord 2002; 40: 118–127.
Aloisi AM . Sensory effects of gonadal hormones. In: Fillingim RB (ed). Sex, gender and pain. Progress in Pain Research and Management. Vol 17. Seattle: IASP Press, 2000; pp 7–24.
Rollman GB, Lautenbacher S & Jones KS . Sex and gender differences in responses to experimentally induced pain in humans. In: Fillingim RB (ed). Sex, gender and pain. Progress in Pain Research and Management. Vol 17. Seattle: IASP Press, 2000; pp 165–190.
Berkley KJ & Holdcroft A . Sex and gender differences in pain. In: Wall PD, Melzack R (ed). Textbook of Pain. 4th edn. London: Churchill Livingstone, 1999; pp 951–965.
Fillingim RB . Sex, gender and pain: a biopsychosocial framework. In: Fillingim RB (ed). Sex, gender and pain. Progress in Pain Research and Management. Vol 17. Seattle: IASP Press, 2000; pp 1–6.
Fillingim RB, Edwards RR & Powell T . The relationship of sex and clinical pain to experimental pain responses. Pain 1999; 83: 419–425.
Lautenbacher S & Rollman GB . Sex differences in responsiveness to painful and non-painful stimuli are dependent upon the stimulation method. Pain 1993; 53: 255–264.
Dao TTT & LeReseche L . Gender differences in pain. J Orofacial Pain 2000; 3: 169–184.
Canli T, Desmond JE, Zhao Z & Gabrielli Jde . Sex differences in the neural basis of emotional memories. Proc Natl Acad Sci USA 2002; 99: 10789–10794.
Finnerup NB et al. Treatment of spinal cord injury pain. Pain Clinical Updates 2001; Vol IX: no 2
Gear RW et al. Kappa-opioids produce significantly greater analgesia in women than in men. Nat Med 1996a; 11: 1248–1250.
Gear RW et al. Gender difference in analgesic response to the kappa-opioid pentazocine. Neurosci Lett 1996b; 205: 207–209.
Gear RW et al. The kappa opioid nalbuphine produces gender- and dose-dependent analgesia and antianalgesia in patients with postoperative pain. Pain 1999; 83: 339–345.
Cook CD et al. Sex-related differences in the antinociceptive effects of opioids: importance of rat genotype, nociceptive stimulus intensity and efficacy at the myopioid receptor. Psychopharmacology 2000; 150: 430–442.
Acknowledgements
The study has been made possible with grants from The Swedish Association of Traffic and Polio Victims (RTP), The Association for Cancer and Traffic Victims (CTRF) and The Swedish Association for the Neurologically Disabled (NHR).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Norrbrink Budh, C., Lund, I., Hultling, C. et al. Gender related differences in pain in spinal cord injured individuals. Spinal Cord 41, 122–128 (2003). https://doi.org/10.1038/sj.sc.3101407
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101407
Keywords
This article is cited by
-
Acute inflammatory profiles differ with sex and age after spinal cord injury
Journal of Neuroinflammation (2021)
-
The short-term effects of head-mounted virtual-reality on neuropathic pain intensity in people with spinal cord injury pain: a randomised cross-over pilot study
Spinal Cord (2021)
-
Neuropathic Pain After Spinal Cord Injury: Challenges and Research Perspectives
Neurotherapeutics (2018)
-
Association of pain, social support and socioeconomic indicators in patients with spinal cord injury in Iran
Spinal Cord (2017)
-
Psychosocial aspects of spinal cord injury pain: a meta-analysis
Spinal Cord (2016)