Abstract
Study design: Pott's paraplegic patients with severe spinal deformity were reviewed retrospectively after being treated with chemotherapy and/or decompressive surgery.
Objectives: To determine the most appropriate treatment protocol and to predict the prognosis for Pott's paraplegics with severe spinal deformity.
Setting: Catholic University of Korea Medical Center and Moon-Kim's Institute of Orthopedic Research, Seoul, Korea from 1971 to 1996.
Method: In this study, there were 33 patients (eight children and 25 adults), ranging from 13 to 56 years of age. They developed spinal tuberculosis at the age of 9 years (range, 2–29 years), and remained neurologically symptom free from an average of 16 years (range, 4–27 years). Four adults who responded well to treatment initially suffered relapses of paraplegia. Only six patients had previously received a full course of triple chemotherapy. Seven (two children, five adults) had healed disease, and 26 (six children, 20 adults) had active disease. Eleven cases had frequent drainage from the sinuses. Kyphoscoliosis was found in 11 patients: four children and seven adults. The remaining patients had kyphosis only. Among the 26 patients with active tuberculosis, 10 had triple chemotherapy itself and the rest had additional decompression surgery (10 anterior and six posterior). All seven patients with healed tuberculosis were subjected only to surgery (two anterior and five posterior).
Results: In seven patients with healed tuberculosis, surgery did not improve neurologically except in one child patient. In four patients, the severity of paralysis remained unchanged and two patients, deteriorated neurologically after surgery. In six children with active tuberculosis, there were remarkable neurological recoveries by either conservative treatment or surgical decompression. Seven adults with active tuberculosis recovered slowly, improving by one or two Frankel grades (three Frankel C, three D, one E). In 11 out of 13 surgically treated adults with active disease, paralysis that had persisted for less than 3 months gradually improved by one or two Frankel grades. One Frankel A and one Frankel B paraplegic patients who had paralysis that had lasted through 6 months did not recover after surgery.
Conclusion: The neurological recovery of Pott's paraplegics with severe spinal deformity resulted in three different outcomes: (1) severe deformity is different from moderate and mild deformities; (2) patients with healed tuberculosis had poorer prognosis than patients with active tuberculosis; (3) children had better prognosis than adults. Furthermore, patients with paralysis persisting over 6 months did not recover neurologically after surgery.
Similar content being viewed by others
Introduction
Pott's paraplegia resulting in severe spinal deformity is a disastrous complication, which is difficult to treat by chemotherapy alone and/or by surgical decompression.1,2,3,4 It is generally accepted that Pott's paraplegia in early spinal tuberculosis can be cured effectively through chemotherapy alone.5,6
Hsu et al. recommended surgical decompression of the compressed cord at the level of active tuberculous focus and kyphosis since this resulted in good neurological results.7 They also stated that in healed tuberculosis with kyphosis, paraplegia secondary to cord compression from a hard bony ridge and peridural fibrous band, responded poorly to anterior decompression surgery. Hsu et al., however, did not mention the efficacy of chemotherapy itself on the neurological recovery of patients with active disease and severe spinal deformity.7 Decompression surgeries, whether anterior or costotransversectomy, performed on patients with severe spinal deformity carries risks, and is not successful in every case. The objective of this retrospective study was to evaluate: (i) the effectiveness of surgical decompression and/or chemotherapy, and (ii) the effect of age on the neurological recovery.
Material and methods
From 1971 to 1996, 33 patients were treated at the Department of Orthopedic Surgery, Catholic University of Korea affiliated hospitals, and Dr Kim's St. Mary Orthopedic Clinic, at Ilsan. The patients were eight children and 25 adults. The mean age was 37 years (range from 13 to 56 years) (Table 1). They were examined and assessed using chart, X-rays, CT and MRI. All the patients were first treated at other hospitals. These patients developed tuberculosis at 9 years of age on average (range from 2 to 29 years), and had remained neurologically symptom free for an average of 16 years (range from 4 to 27 years). Four of the 33 patients suffered relapses of paraplegia, and were all treated initially by chemotherapy alone. Seven (two children and five adults) had healed disease and 26 had active disease (six children and 20 adults) with frequent drainage from the sinuses (11 cases–two children and nine adults). Kyphoscoliosis was found in four children (three active and one healed), and in seven adults (four active and three healed). The ratio of kyphosis to kyphoscoliosis was 2 to 1 (Table 2). All the patients had severe kyphosis over 78 degrees (ranging from 78° to 134°).
The tuberculous lesion was defined to be active when a patient had draining sinuses and/or clinically evident abscesses, supported with positive laboratory data and image findings. On initial examination, the quiescent disease was clinically regarded as a doubtfully active disease, that was also proven by surgery in the current study. A diagnosis of the healed disease was made when there was solid fusion of the involved vertebrae on radiograms. This was further proven through decompressive surgery, and where there was no other evidence of active disease as mentioned above. All the patients had a previous history of two-drug chemotherapy, and four patients suffered relapses of paralysis.
Neurological status
A. Healed tuberculosis cases (n=7)
On admission, all had incomplete spastic paralysis, and were subjected to surgery. Among two children one had Frankel C and the other had Frankel D paralysis, while among five adults three had Frankel B and the two had Frankel C paralysis.
B. Active tuberculosis cases (n=26)
(a) On admission, six children had incomplete paralysis (four Frankel B, two Frankel C). In three children, paralysis progressed, and they were subjected to surgery. (b) On admission, 20 adults had various degrees of paralysis: three Frankel A (subjected to surgery), six Frankel B (two conservative, four surgery), nine Frankel C (three conservative, six surgery), and two Frankel D paralysis (conservative). In seven adults, paraplegia progressed following admission. The neurological statuses of 13 adults on the day of surgery were grave: six Frankel A and seven Frankel B.
Treatment protocol
In all cases, triple chemotherapy was initiated immediately after the initial examination, including cases that were presumed healed, until the healing was confirmed by surgery. Chemotherapy was continued for 12–18 months in the 26 patients with active disease. Ten patients with active disease (three children and seven adults) refused to have surgery, thereby, only chemotherapy was instituted. All 23 patients who were subjected to surgery provided an informed consent.
Among the seven healed cases, five (one child and four adults) were subjected to posterior decompression using a bilateral costotransversectomy approach, while two patients (one child and one adult) had anterior decompression. Posterior instrumental stabilization was instituted in one child and one adult who had bilateral costotransversectomy.
Of 26 patients with active disease, 16 had decompression surgery (12 anterior and four bilateral costotransversectomy). The remaining 10 had chemotherapy alone because they declined to have surgery and they had very poor pulmonary function. Three of six children with active disease had surgery (one anterior decompression and two posterior decompression), and the other three children were conservatively treated because of their poor general condition and poor pulmonary function. Among the 20 adults with active disease, seven had a conservative treatment and 13 had surgery (nine anterior and four posterior decompression surgery) (Table 3).
Assessment of neurology
In all cases, neurological statuses were assessed regularly at 1 and 2 weeks, and 1, 3, 6, 12, and 18 to 24 months after initial treatment.
Results
A. Healed tuberculosis cases (n=7)
In two children, one child recovered completely from Frankel C to E, and another child, became worse neurologically (from Frankel D to C) after decompression surgery.
In five adults, three Frankel B paraplegics did not improve at all, and among the remaining two Frankel C adult paraplegics, one became worse and the other remained unchanged. (Table 4).
B. Active tuberculosis
1. Children (n=6)
Among the three children treated conservatively, two recovered completely from Frankel B and C to E, and one recovered from Frankel B to D.
The three children treated surgically (two Frankel B, and one C) developed complete paralysis immediately after surgery, which subsequently recovered nearly to normal (two Frankel D, one E). In children with active disease, there were remarkable neurological recoveries regardless of the treatment method (Table 5).
2. Adults (n=20)
Seven adults treated conservatively recovered gradually, up by one or two Frankel grades (three Frankel C, three D, one E).
Among the 13 surgically treated adults (six Frankel A, seven B), one with Frankel B paralysis and one with Frankel A paralysis over a 6 month period, did not recover. The 11 remaining adults who had paralysis for 2 to 3 months showed a gradual neurological improvement of one or two grades (two Frankel B, four C, four D, one E).
The adult patients treated conservatively with active disease had good neurological recovery comparable to that of the surgically treated patients.
For the six conservatively treated children, the neurological recovery took 2 to 3 months while for the seven adults, recovery was 3 to 7 months. The 16 patients (three children and 13 adults) treated surgically took 1 to 2 months to recovery (Table 6).
Illustrative cases
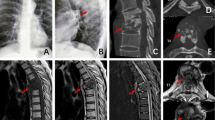
Case 1 (Figure 1)
A 39 year-old woman with severe tuberculous kyphoscoliosis (T7–T9) was transferred to our hospital from a provincial hospital because of gradually worsening spastic paralysis of the lower extremities (Frankel C) over 2 months in spite of triple chemotherapy consisting of INH, ethambutol and rifampicin (A). It was known that she suffered from tuberculosis of spine since the age of 17 years, and that she had complete two drug antituberculous chemotherapy (INH, PAS). Preoperatively there were elevation of erythrocyte sedimentation rate (65 mm/h) and increase of CRP (12 mg/dl). The preoperative MRI showed a thin tortuous cord, but no frank pus was observed around the tuberculous lesion (B). Immediately after admission, pyrazindmide was added to three drug regimen (INH, ethambutol, rifampicin). Surgery was delayed for 3 months because the informed consent could not be obtained. Prior to surgery she walked aided with crutches. After anterior decompression surgery, she recovered from frankel C paralysis to D (C), and the postoperative MRI showed a normally expanded cord at the decompression site (D). During surgery only granulation tissue around cord was found at the maximally cord-compressed site of the cord. She recovered uneventfully after surgery and could walk unaided 10 days after surgery.
Case 2 (Figure 2)
(A) Tuberculous kyphoscoliosis at T10–T12 in a 14 year-old boy with Frankel C paralysis. (B) Corrected deformity after bilateral costotransversectomy and instrumented correction with Rush nails and segmental wires. (C) Three rib grafts placed between T10–L1 to fill up the anterior column defect which was developed after instrumented deformity correction. (D) Well maintained corrected deformity at 7 months after anterior rib graft
A 14 year-old boy with kyphoscoliosis previously suffered from tuberculosis of the spine at the age of 2 years, which was thought to be treated effectively by chemotherapy. Over the next 10 years, he had not suffered from relapses of tuberculosis and paralysis (A). Thereafter, he developed a gradual weakness of the lower extremities over 2-month period (Frankel C). Bilateral costotransversectomy and bilateral posterior segmental stabilization, utilizing Rush nails and Kirschner wires were performed as a first step procedure to decompress the spinal cord, to correct the deformity, and to stabilize the destabilized spine (B). This was followed by an anterior rib strut graft procedure to fill up the anterior column defect (C). During surgery it was found that the tuberculous lesion was the healed one, because there were neither pus or granulation tissue. Culture for tuberculous bacilli was also negative. He was completely paralysed immediately after surgery, but recovered fully in 4 weeks. Radiograms, taken at postoperative 7 months, showed two pieces of rib grafts between T10–L1(D). The patient was very satisfied postoperatively, because he could lie on his back postoperatively.
Discussion
Paraplegia together with residual spinal deformity is one of the most disastrous complications of Pott's disease.3,4,6,8,9,10,11 Up to now, there have been numerous papers which dealt with Pott's paraplegia12,13,14,15,16 however, there are only a few papers, which addressed Pott's paraplegics complicated by severe spinal deformity.11,12,15 An accurate assessment of the disease activity is necessary in order to achieve a successful outcome before any initiation of treatment. A single radiographic assessment of activity is notoriously difficult because a patient does not always show clinical evidence of activity. Generally, it has been believed that chemotherapy alone is an inappropriate method for managing paraplegia in patients with advanced tuberculosis and deformity,1,7,16 since paraplegia usually resolves rapidly after adequate decompression. Many surgeons believe that it is inappropriate to require a patient to lie paralysed for extended periods waiting for a cure through conservative care, and prefer management by anterior decompression and fusion with bone graft.1,7,10,16 Therefore, the afore-mentioned treatment protocol has been well accepted, and was used for paraplegic patients with mild and moderate degrees of spinal deformity.
However, those principles could not effectively solve the neurological problems in Pott's paraplegic patients with severe spinal deformity. Chemotherapy was instituted first, but when patients were unresponsive, and had worsening neurology, decompression surgery was indicated. In these patients, radical decompressive surgery carried a high neurological risk with only a small chance of recovery.
In previous studies, the senior author of this study had listed the factors influencing the neurological recovery rate in Pott's paraplegics.5,6 The recovery rate is influenced by many factors such as: the patient's general condition, the patient's age, the condition of the spinal cord, the level, duration and severity of paraplegia, the time of onset before the initiation of treatment, the type of treatment, and the patient's drug sensitivity.
Paraplysis persisting longer than 6 months is unlikely to improve. Late paralysis with inactive disease and significant kyphosis is much less responsive to treatment as found in this current series. Paralysis caused by vascular embarrassment has a worse prognosis. Patients with an atrophic spinal cord assessed by a preoperative MRI usually do poorly after decompression.
In summary, chronicity of paralysis, late paralysis in the inactive stage, and ischemic and atrophic cord are the worst factors, which provided disappointing prognosis in our series. Thereby, it is strongly recommended that these factors are assessed before the start of any treatment for Pott's paraplegic patients with severe spinal deformity. When surgical decompression is chosen as a last choice of treatment, each patient should be cautioned about the high neurological risk and the slim chance of neurological recovery by surgery even under the cover of chemotherapy.6,17
In treating adult patients with chronic Pott's paraplegics with severe spinal deformity, decompression surgery should be avoided to prevent damage to the circulation and the compressed spinal cord. However, for child paraplegics, more promising results may be obtained through decompression surgery. That is, neurological recovery was better in children who had decompression surgery than in adults who received chemotherapy alone or in combination with decompression surgery.
It is noteworthy to remind treating physicians and surgeons that paraplegics with a severely deformed spine showed a different neurological response to chemotherapy treatment or combined chemotherapy and surgical treatments than those paraplegics with mild to moderate degrees of spinal deformity. Adult paraplegic with severe spinal deformities had poorer spinal cord conditions than those with milder deformities.5,18 Thus, it is essential to assess the condition of the spinal cord through plain X-rays, myelograms, C-T myelograms and MRI before any treatment commences. It is strongly recommended that a spinal cord circulation study be conducted wherever possible.
In two cases of this current series, the authors attempted to combine decompression surgery with posterior corrective and instrumented stabilization surgery because of segmental instability after decompression surgery. In one case, the deformity was corrected successfully and neurological recovery ensued, while in the other cases, there was no neurological recovery despite effective decompression and a relatively good correction of the deformity. For corrective surgery the risk of neurological damage by operative distraction was related both to the severity of the original deformity and to the degree of correction. For posterior instrumented corrective surgery, the length of the vertebral canal and vertebral column should be considered. A short cord may be placed at more risk in idiopathic scoliosis by posterior instrumented correction because of the short vertebral canal in comparison to the vertebral column. Thus, anterior surgery excising the body and discs may lengthen the vertebral canal relatively, and is less dangerous to the spinal cord.19 A preoperative measurement of the vertebral canal and column length might help to quantify the risk of neurological damage.
A spine with tuberculous kyphosis and kyphoscoliosis is different from idiopathic scoliosis. It was reported that a spine with tuberculous kyphosis had a relatively longer vertebral canal than vertebral column.20 Based on this information, posterior corrective surgery of tuberculous kyphosis seems clinically safe, although in practicality there are risks. Therefore, an assessment of the comparative length and shape of the vertebral canal and the column, and a three dimensional MRI assessment of the condition of the spinal cord in the canal are useful prognostic indicators for determining the risk of neurological injury during surgery.
Recently, there has been a trend by a small group of very aggressive spine surgeons to utilize a total spondylectomy procedure to excise the diseased or deformed segment of the spine compressing the cord and/or to correct deformity.20,21,22 However, it must be emphasized that the surgical procedure of total en bloc excision is difficult and dangerous with a high complication rate2,5,6,19,23. The advocates of total en bloc spondylectomy stress there is a chance of recovery from surgery, and that the procedure is safe. However, authors of this study do not recommend the total en bloc spondylectomy procedure for Pott's paraplegics with severe deformity. Most Pott's paraplegics with severe spinal deformity have an ischemic thin, and flattened spinal cord and they do not respond well neurologically to any type of decompression surgery.
In this study, it was found that the patients with active tuberculosis who showed a neurological response after the start of chemotherapy, achieve more favorable result when surgery was combined. Patients who did not show any evidence of recovery or showed worsening signs after 4∼6 weeks of chemotherapy, had poorer results even though an MRI did not show atrophic cord. The cases in which paralysis progressed slowly over several months and where there was no response to chemotherapy, showed no improvement neurologically after decompressive surgery. The patients who developed paralysis with acute and rapidly progressive pain responded to chemotherapy and also responded better to surgery. The patients who had paralysis which persisted for over 6 months before treatment, did not recover by surgery.
In summary, an accurate assessment of the spinal cord condition, the length of the compressed cord segment in the spinal canal, and a measurement of the length of the vertebral canal and column for posterior deformity correction surgery are very important in selecting the appropriate surgical candidates. Assessment of the cord and peridural conditions, utilizing CT, CT-myelograms and MRI can provide information in selecting the most effective method of treatment to reverse the paralysis.
References
Ahn BH . Treatment of Pott's paraplegia. J Korean Orthp Assoc 1967; 2: 75–87.
Goel MK . Treatment of Pott's paraplegia by operation. J Bone Joint Surg 1967; 49B: 674–681.
Govender S, Charles RW, Naildo KS & Gogre IE . Result of surgical decompression in chronic tuberculous paraplegia. S Afr Med 1988; 74: 58–59.
Moon MS & Lee MK . The Change of the kyphosis of the tuberculosis of spine in children following ambulant treatment. J Korea Orthop Assoc 1971; 6(3): 189–202.
Moon MS et al. Pott's paraplegia 67 cases. Clin Orthop 1996; 323: 122–128.
Moon MS . Tuberculosis of the spine–controversies and a new challenge. Spine 1997; 22(15): 1791–1797.
Hsu LCS & Leong JCY . Tuberculosis of the lower cervical spine (C2 to C7): A report on 40 cases. J Bone Joint Surg 1984; 66B: 1–5.
Frankel HL et al. The value of postural reduction in the initial management of closed injuries of spine with paraplegia and tetraplegia. Paraplegia 1969; 7: 179–192.
Guirgui AR . Pott's paraplegia. J Bone Joint Surg 1967; 49B: 658–667.
Hodgson AR, Shinesnes OK & Leong CY . The pathogenesis of Pott's paraplegia. J Bone Joint Surg 1967; 49A: 1147–1153.
Moon MS et al. Posterior instrumentation and anterior interbody fusion for tuberculosis kyphosis of dorsal and lumbar spine. Spine 1995; 20: 1910–1916.
Kee JI, Kang SY, Moon MS & Suk SI . Treatment of the spinal tuberculosis with severe kyphosis and paraplegia. J Korean Orthop. Assoc 1970; 5: 73–78.
Kim BJ, Ko HS & Lin Y et al. Surgical treatment of paraplegia in spinal tuberculosis. J Korean Orthop Assoc 1993; 28: 1595–1602.
Kim NH . Study of causal factor of Pott's paraplegia. J Korean Orthop Assoc 1974; 9: 209–220.
Lee HK, Ahn JW & Choi JS . Treatment of spinal tuberculosis associated with neurological symptoms. J Korean Orthop Assoc 1980; 15: 236–241.
Martin NS . Pott's paraplegia. J Bone Joint Surg 1971; 53B: 596–608.
Winter RB . Major neurological complications in spinal deformity surgery: one surgeon's carrer experience (review article). J Orthop Surg 1999; 7(2): 81–88.
Pattisson PR . Pott's paraplegia: An account of the treatment of 89 consecutive patients. Paraplegia 1986; 24: 77–91.
Bridwell KH, Lenke LG, Baldus C & Blanke K . Major intraoperative neurological deficits in pediatric and adult spinal deformity patients: Incidence and etiology at one institution. Spine 1998; 23: 324–331.
Porter RW . Idiopathic scoliosis – the relation between the vertebral canal and the vertebral bodies. Spine 2000; 25: 1360–1366.
Shimada Y, Abe E & Sato K . Total en-bloc spondylectomy for correcting congenital kyphosis. Spinal Cord 2000; 38: 382–385.
Tomita K et al. Total en bloc spondylectomy: A new surgical technique for primary malignant vertebral tumors. Spine 1997; 22: 324–333.
Kee JI & Hahn MS . A clinical study on 40 cases of Pott's paraplegia. J Korean Orthop Assoc 1987; 2: 19–24.
Acknowledgements
To Mr Rick Low and Mrs Cecilia Moon our recognition for their help in revision of the manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Moon, MS., Moon, JL., Moon, YW. et al. Pott's paraplegia in patients with severely deformed dorsal or dorsolumbar spines: treatment and prognosis. Spinal Cord 41, 164–171 (2003). https://doi.org/10.1038/sj.sc.3101366
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101366
Keywords
This article is cited by
-
Late onset of progressive neurological deficits in severe angular kyphosis related to tuberculosis spondylitis
European Spine Journal (2016)
-
Late treatment of tuberculosis-associated kyphosis: literature review and experience from a SRS-GOP site
European Spine Journal (2013)
-
Clinical and radiological outcomes after conservative treatment of TB spondylitis: is the 15 years’ follow-up in the MRC study long enough?
European Spine Journal (2013)
-
International spinal cord injury musculoskeletal basic data set
Spinal Cord (2012)
-
Late onset Pott’s paraplegia in patients with upper thoracic sharp kyphosis
International Orthopaedics (2012)