Abstract
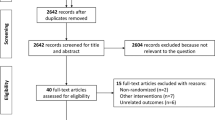
Study design: Literature review to evaluate the complications seen in patients on intermittent catheterization (IC) and intermittent self-catheterization (ISC).
Objectives: To find the prevalence of most complications seen in patients on IC. To study the prevention and the treatment of these complications.
Setting: An international literature review.
Methods: Most relevant articles on the subject are reviewed.
Conclusion: Urinary tract infection is the most frequent complication in patients performing IC. Catheterization frequency and the avoidance of bladder overfilling are amongst the most important prevention measures. Asymptomatic bacteriuria does not need to be treated with antibiotics. Long-term antibacterial prevention does seem to bear a risk of development of bacterial resistance. Previous treatment with indwelling catheters is a risk factor for chronic infection and urinary sepsis. Prostatitis is more frequently present than often thought. Epididymitis and urethritis are rare. Trauma from catheterization occurs regularly, but lasting effects are more limited. However, the prevalence of urethral strictures and false passages increases with longer use of IC. The use of hydrophilic catheters might be able to lower the urethral complication rate but additional proof through comparative studies is needed. The most important prevention measures are good education of all involved in IC, good patient compliance, the use of a proper material and the application of a good catheterization technique.
Similar content being viewed by others
Introduction
Intermittent catheterization (IC) is nowadays widely used for the urological management of patients with a neurogenic bladder due to a spinal cord lesion. The fact that bladder emptying can be achieved without foreign material remaining permanently in the lower urinary tract has shown many advantages. IC with adjunctive treatment using bladder relaxing drugs seems to be able to keep the urodynamic functions of bladder pressure and bladder compliance within safe limits even in the long term. IC is considered preferable to other forms of bladder emptying in neuropathic patients as it has less complications and a better outcome. Most authors endorse this opinion by comparing the outcome with previous treatment methods. Several studies1,2,3 compared urological outcome in patients from 2–15 years after SCI and found that those with indwelling catheter, transurethrally or cystostomy, reflex voiding and incontinence pads had worse outcomes and more frequent and more serious complications compared to those on IC. Also in recent studies4,5 the incidence of both urinary tract dilatation and vesicoureteral reflux was significantly lower in the IC group then if abdominal straining, Crede, tapping and indwelling catheter were used.
On the other hand, the introduction of a catheter several times a day can give rise to complications. This review gives data on the major complications occurring in patients on intermittent catheterization (IC) and self-catheterization (ISC). It also looks into treatment and prevention of these complications.
Method
We looked into the most relevant literature data about complications of IC published during the last 25 years.
Results
One of the most frequent complications is infection of the urinary tract (UTI). Prevalence of UTI varies widely in the literature. This is due to the various methods used for evaluation, to the different techniques of IC, different frequencies of urine analysis, different criteria for infection, whether prophylaxis is used, to the group of patients studied, and other factors. Some publications give the percentage of sterile urine: between 12 and 88%.6,7,8,9,10,11,12 Eleven per cent prevalence for asymptomatic UTI and 53% for symptomatic bacteriuria are given in different series.13,14 Bakke15 found in 407 patients, 252 with neurogenic bladder, during an observation period of one year, 24.5% with non-clinical UTI, 58.6% with minor symptoms, 14.3% with more comprehensive or frequent symptoms, while 2.6% claimed major symptoms. Biering-Sörensen et al16 found in 77 SCI patients, on IC for 5 years, that 81% had been treated for at least one UTI. Twenty-two per cent had two/three UTI/year and 12% four or more UTI/year. It remains difficult, however, to get a proper estimate of the risk of infection from literature. The data differ so much, that many different factors must influence the prevalence of this complication.
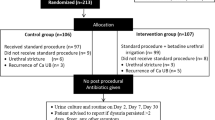
In the acute stage of SCI, with proper management, urine can be kept sterile for 15–20 days without antibiotic prophylaxis, and for 16–55 days if prophylaxis is given.17,18,19 Prieto-Fingerhut et al20 determined in a randomized controlled trial the effect of sterile and non-sterile IC on the incidence of urinary tract infection in 29 patients after SCI. With urine analysis on a weekly basis they found in the group on sterile IC a 28.6% UTI incidence while in the non-sterile catheterization group 42.4% incidence was found. The cost of antibiotics for the sterile IC group was only 43% of the cost for those on non-sterile IC. However, the cost of the sterile IC kits was 371% of the cost of the kits used by the non-sterile IC group, bringing the total cost of the sterile program to 277% of the other program. Rhame and Perkash18 published the results of UTI prevalence in 70 SCI patients in the initial rehabilitation hospitalization treated with sterile catheterization and a neomycin-polymixin irrigant. Fifty-four per cent developed an infection at an over-all rate of 10.3 infections per 1000 patient-days on IC. Bakke and Volset21 studied factors that may predict the occurrence of bacteriuria and clinical UTI in 302 patients using clean IC. Predictive factors of clinical infection were low age and high mean catheterization volume in women, low age, neurogenic bladder dysfunction and nonself-catheterization in men, in addition to urine leakage in patients with neurogenic dysfunction. Bacteriuria was a risk factor of future clinical infection. Risk factors for bacteriuria were present in men: low frequency of catheterization, high age and non-self-catheterization. If antibacterial prophylaxis was used, fewer episodes of bacteriuria were noticed, but significantly more clinical UTI were seen. Shekelle et al made a systematic review of risk factors for UTI in adults with spinal cord dysfunction.22 In this review article they evaluated 22 studies, from which many, however, had important methodological deficiencies. They found two studies that provide evidence supporting increased bladder residual volume as a risk factor. Patients on IC had fewer infections than those with indwelling catheters. They found conflicting evidence over the value of sterile or `non touch' catheter techniques compared with CIC. They found insufficient evidence to assess risk due to psychological, behavioral and hygiene factors, sex, level of function and time since injury.
In order to diagnose UTI, it should be recommended to obtain the urine by catheterization.23 The frequency of examining urine samples differs greatly between studies. Several advocate daily use of a dipslide technique during the acute phase after SCI, once a week during the subacute phase and monthly or a few times a year in long-term care.24,25,26 If a urine culture reveals more than 104 cfu/ml, this indicates significant bacteriuria. Pyuria alone is not considered reliable in patients with neurogenic bladder.27,28 The bacteria found mostly are E Coli, Proteus, Citrobacter, Pseudomonas, Klebsiella, Staphylococcus aureus and faecalis in short-term cases while the same bacteria plus Acinetobacter and Streptococcus faecalis are found in the long-term IC patients.29,30 E Coli is considered the dominant species in several studies.15 The detection of E Coli on the periurethra corresponds in much higher percentage (93%) with bacteriuria than if other bacteria are present on the periurethra (80% or less).31 E Coli isolates from patients who develop symptomatic UTI may be distinguished from bacteria recovered from patients who remain asymptomatic and possibly from normal fecal E Coli.32 Urinary sepsis is fortunately rare.33,34 Previous treatment with an indwelling catheter represents a special risk to develop sepsis.35 In his thesis Wyndaele36 found sepsis in 21 of 115 patients with SCI during the in hospital rehabilitation. The prevalence of sepsis was highest in those treated beforehand with an indwelling catheter. Factors of risk were the period of 24 h to 3 days after changing from indwelling to IC drainage when UTI was present.
Wyndaele and Maes37 in their follow-up study in 69 patients with neurogenic bladder and a literature survey till 1989 on IC found justification of several conclusions concerning the relationship between IC and UTI: If catheterization is begun by patients with recurrent or chronic UTI and urinary retention, the incidence of infection decreases and patients may become totally free of infection; If symptomatic infections occur, improper practice of IC or misuse can often be found; Chronic infection persists after IC has been started, if the cause of the chronicity remains.
To prevent UTI a non-infecting technique is needed. But also some additional factors can play a role in infection prevention. Nursing education is important and educational intervention by a clinic nurse is a simple, cost-effective mean to decrease the risk of UTI's in individuals with SCI on IC who are identified as at risk.38 Anderson19 found a fivefold incidence when IC was done 3 times a day compared to 6 times a day. Also prevention of bladder overdistention is important.22,39 Cross infection is less if IC during hospitalization is done by a catheter team40 or by the patients themselves.41 As residual urine plays a role in infection, attention must be made to empty the bladder completely.22
Treatment of UTI is necessary if the infection is symptomatic. Waites et al42 treated men with SCI on IC to determine efficacy of ciprofloxacine 1 g per day for 10 days in eradicating susceptible organisms from urine, urethra and perineum. Susceptible bacteria disappeared from urine in all and were significantly reduced in perineum and urethra. However they were replaced shortly after by resistant Gram-positive cocci. This shows the importance to reserve antibiotics for symptomatic patients only and to take into account the data from the antibiogram. The value of non-treatment for chronic non-symptomatic bacteriuria throughout an hospitalization has been demonstrated.43
Whether antibacterial prophylaxis improves the infection rate has been the subject of different studies, but randomized controlled trials are scarce. Pearman44 compared two groups of patients with acute SCI treated with non-touch IC and found that those who had kanamycin colistin solution instilled into the bladder at the end of each catheterization had only half the incidence of significant bacteriuria. The same effect could not be found in a comparison study with instillations of neomycin.45 Ascorbic acid has been used by several authors. It is considered only useful as adjuvant therapy together with other antibacterial drugs.46,47 Johnson et al48 in a 3 months study in children on IC found a prevalence of UTI of 39% with placebo and 19% on single daily dose prophylaxis with nitrofurantoin. Anderson19 found a significant reduction in infection rates when patients were treated with intravesical neomycin/polymyxin-B and low dose of nitrofurantoin, also prophylaxis with methenamine mandelate and acidification, and with methenamine hippurate resulted in a lower infection rate.15,49 Cranberry juice has been evaluated recently in children on IC and showed no convincing effect on bacteriuria.31 Several studies have studied the risk of developing dangerous resistance to antibiotics when given prophylactically either orally or by instillation.50,51,52 Galloway et al53 state that the threat of emergence of resistant organisms, the risk to patients of side effects to the antibiotics, the expense and the risk to other patients from cross infection with resistant organisms are strong arguments against prophylactic antibacterials.
An overall conclusion can not be made at this stage. However it would seem logical to use antibacterial prophylaxis only for a short time, during the initial stage of IC. It does seem to be less indicated for long-term use though it can help specific patients to lower the rate of symptomatic infections for which no well defined cause is found.
Urethritis and epididymo-orchitis have been reported in several case series (Table 1). The prevalence figures vary widely. This may be related to differences in IC technique, materials used, and investigation method. But also the primary treatment can be very important. With long-term indwelling catheter, a larger prevalence is seen.36 Genital infections can lower fertility in SCI patients. Allas54 performed two spermograms, one before and one after an episode of epididymitis in paraplegics on IC, and found that azospermia increased from 7 to 50% when epididymitis occurred. If IC is used to empty the neurogenic bladder, better sperm quality and better pregnancy rates have been found than with indwelling catheterization.55,56
Prostatitis can be a cause of recurrent UTI. Either acute or chronic it is difficult to diagnose in patients with neurogenic bladder and special tests have been developed for this.69,70 The overall incidence was previously thought to be around 5 to 18%71 but 33% may be a more realistic figure.67
Urethral bleeding is frequently seen in new patients, and occurs regularly in one-third on a long-term basis.62 Trauma of the urethra especially in men can cause false passages, meatal stenosis but the incidence is rare (Table 1). The incidence of urethral strictures increases with a longer follow-up, with most events occurring after 5 years of IC.37,67 Günther et al72 in 2000 presented their results on 230 men on IC, and found urethral changes in 26.9% (3.7% strictures) when previously an indwelling catheter had been used.72 In men with IC and no history of indwelling catheter the prevalence of urethral changes was 16.9% and no strictures had occurred. Moreover in 311 men, not on IC, with a history of indwelling catheter 25.4% urethral changes (2.5% strictures), and without a history of indwelling catheter, 17.9% urethral changes (1.5%) strictures were found. Urethral changes were also documented in SCI men on IC for an average of 5 years, using one single re-usable silicone catheter for an average of 3 years (from 1 to 7 years).73 Urethrograms showed 70% normal, 11% minor abnormalities, 15% narrowed urethra and 4% stricture that needed operation.
To prevent urethral strictures, gentle introduction of the catheter, substantial lubrication of the catheter and perhaps the use of hydrophilic catheters can play a role. Forceful manipulation during catheter insertion and significant bleeding proved important contributory factors for the development of urethral strictures in patients on IC.74 The surface of the catheter is claimed to be an important factor, with less stricture development when hydrophilic catheters are used. The degree of urethral inflammation by urethral cytology proved to be less in patients using hydrophilic catheters compared to PVC catheters.75 No extra strictures occured in patients on IC with hydrophilic catheters after a mean follow-up of 7 years in a study of Waller et al.76 Such data are suggestive that there is an advantage in using hydrophilic catheters to prevent stricture formation in the long-term but comparative studies have not been published. Urethral trauma with false passages can, in neurogenic patients on CIC, successfully be treated with 5 days antibiotics and 6 weeks indwelling catheter. The false passage will disappear also on cystoscopy and IC can be safely restarted.77
Other complications such as hydronephrosis, vesico-ureteral reflux, and bladder cancer seem to relate rather to infection, bladder trabeculation, detrusor pressure or neuropathy than to IC itself.78
Bladder calculi caused by the introduction of pubic hair,79,80 loss of the catheter in the bladder,81 bladder perforation and bladder necrosis82 have been reported as rare complications of IC.
Conclusion
There are strong arguments that intermittent catheterization is a safe and efficacious method to treat neurogenic bladder dysfunction due to a spinal cord lesion. Complications can occur. Urinary tract infection is the most important, but prevention is possible in the short-term. Infection of the uro-genital organs seems mostly related to the primary treatment given. Trauma from catheterization occur regularly, but lasting effects are more limited. However the prevalence of urethral strictures and false passages increases with longer use of IC. The use of hydrophilic catheters might be able to lower the urethral complication rate but additional proof through comparative studies would be welcome. Other complications of IC are occasional.
Very important are good education of all involved in IC, good patient compliance, the use of a proper material and the application of a good catheterization technique.
References
Wyndaele JJ, De Sy A, Claessens H . Evaluation of different methods of bladder drainage used in the early care of spinal cord injury patients Paraplegia 1985 23: 18–26
McGuire EJ, Savastano J . Comparative urological outcome in women with spinal cord injury J Urol 1986 135: 730–731
Bennett CJ et al. The effect of urethral introducer tip catheters on the incidence of urinary tract infection outcomes in spinal cord injured patients J Urol 1997 158: 519–521
Giannantoni A et al. Clean intermittent catheterization and prevention of renal disease in spinal cord injury patients Spinal Cord 1998 36: 29–32
Weld KJ, Dmochowski RR . Effect of bladder management on urological complications in spinal cord injured patients J Urol 2000 163: 768–772
Guttmann L, Frankel H . The value of intermittent catheterization in the early management of traumatic paraplegia and tetraplegia Paraplegia 1966 4: 63–83
Pearman JW . Prevention of urinary tract infection following spinal cord injury Paraplegia 1971 9: 95–104
Lapides J, Diokno AC, Lowe BS, Kalish MD . Follow-up on unsterile intermittent self-catheterization J Urol 1974 111: 184–187
Donovan W, Stolov W, Clowers D, Clowers M . Bacteriuria during intermittent catheterization following spinal cord injury Arch Phys Med Rehabil 1978 59: 351–357
Maynard F, Diokno A . Urinary infection and complications during clean intermittent catheterization following spinal cord injury J Urol 1984 132: 943–946
Murray K, Lewis P, Blannin J, Shepherd A . Clean intermittent self-catheterization in the management of adult lower urinary tract dysfunction Br J Urol 1984 56: 379–380
Wyndaele JJ . Clean intermittent self-catheterization in the prevention of lower urinary tract infections In: Van Kerrebroeck Ph, Debruyne F (eds) Dysfunction of the lower urinary tract: present achievements and future perspectives Bussum: Medicom 1990 pp. 187–195
Sutton G, Shah S, Hill V . Clean intermittent self-catheterization for quadriplegic patients-a five year follow up Paraplegia 1991 29: 542–549
Whitelaw S, Hamonds J, Tregallas R . Clean intermittent self-catheterization in the elderly Br J Urol 1987 60: 125–127
Bakke A . Clean intermittent catheterization-physical and psychological complications Scan J Urol Nephrol Suppl 1993 150: 1–69
Biering-Sorensen F, Nielans HM, Dorflinger T, Sorensen B . Urological situation five years after spinal cord injury Scand J Urol Nephrol 1999 33: 157–161
Ott R, Rosier AB . The importance of intermittent catheterization in bladder re-education of acute spinal cord lesions. Proceedings of the 18th Vet Admi Spinal Cord Injury Conference, 1971 18: 139–148
Rhame FS, Perkash I . Urinary tract infections occurring in recent spinal cord injury patients on intermittent catheterization J Urol 1979 122: 669–673
Anderson RU . Prophylaxis of bacteriuria during intermittent catheterization of the acute neurogenic bladder J Urol 1980 123: 364–366
Prieto-Fingerhut T, Banovac K, Lynne CM . A study comparing sterile and nonsterile urethral catheterization in patients with spinal cord injury Rehabil Nurs 1997 22: 299–302
Bakke A, Vollset SE . Risk factors for bacteriuria and clinical urinary tract infection in patients treated with clean intermittent catheterization J Urol 1993 149: 527–531
Shekelle PG et al. Systematic review of risk factors for urinary tract infection in adults, with spinal cord dysfunction J Spinal Cord Med 1999 22: 258–272
Barnes D et al. Correlation of bacteriological flora of the urethra, glans and perineum with organisms causing urinary tract infection in the spinal injuries male patient Paraplegia 1992 30: 851–854
King RB et al. Clean and sterile intermittent catheterization methods in hospitalized patients with spinal cord injury Arch Phys Med Rehabil 1992 73: (9) 798–802
Darouiche R et al. Progression from asymptomatic to symptomatic urinary tract infection in patients with SCI: a preliminary study J Am Parap Soc 1992 16: 219–224
National Institute on Disability and Rehabilitation Research Consensus Statement Jan 27–29, 1992. The prevention and management of urinary tract infections among people with spinal cord injuries J Am Parap Soc 1992 15: 194–204
Gribble MJ, Puterman ML, McCallum NM . Pyuria: its relationship to bacteriuria in spinal cord injured patients on intermittent catheterization Arch Phys Med Rehabil 1989 70: 376–379
Menon EB, Tan ES . Pyuria: index of infection in patients with spinal cord injury injuries Br J Urol 1992 69: 141–146
Noll F et al. Intermittent catheterization versus percutaneous suprapubic cystostomy in the early management of traumatic spinal cord lesions Paraplegia 1988 26: 4–9
Yadav A, Vaidyanathan S, Panigraphi D . Clean intermittent catheterization for the neuropathic bladder Paraplegia 1993 31: 380–380
Schlager TA et al. Correlation of periurethral bacterial flora with bacteriuria and urinary tract infection in children with neurogenic bladder receiving intermittent catheterization Clin Infect Dis 1999 28: 346–350
Hull RA, Rudy DC, Wieser IE, Donovan WH . Virulence factors of Escherichia coli isolates from patients with symptomatic and asymptomatic bacteriuria and neuropathic bladders due to spinal cord and brain injuries J Clin Microbiol 1998 36: 115–117
McGuire EJ, Diddel G, Wagner Jr F . Balanced bladder function in spinal cord injury patients J Urol 1977 118: 626–628
Sperling KB . Intermittent catheterization to obtain catheter-free bladder in spinal cord injury Arch Phys Med Rehabil 1978 59: 4–8
Barkin M et al. The urological care of the spinal cord injury patient J Urol 1983 129: 335–339
Wyndaele JJ . Early urological treatment of patients with an acute spinal cord injury. Thesis Doctor in Biomedical Science State University Ghent 1983
Wyndaele JJ, Maes D . Clean intermittent self-catheterization: a 12 year follow-up J Urol 1990 143: 906–908
Barber DB, Woodard FL, Rogers SJ, Able AC . The efficacy of nursing education as an intervention in the treatment of recurrent urinary tract infections in individuals with spinal cord injury SCI Nurs 1999 16: 54–56
Lapides J, Diokno AC, Gould FR, Lowe BS . Further observations on self-catheterization J Urol 1976 116: 169–172
Lindan R, Bellomy V . The use of intermittent catheterization in a bladder training program, preliminary report J Chron Dis 1971 24: 727–735
Wyndaele JJ, De Taeye N . Early intermittent self-catheterization after spinal cord injury Paraplegia 1990 28: 76–80
Waites KB, Canupp KC, Brookings ES, DeVivo MJ . Effect of oral ciprofloxacin on bacterial flora of perineum, urethra, and lower urinary tract in men with spinal cord injury J Spinal Cord Med 1999 22: 192–198
Lewis RI, Carrion HM, Lockhart JL, Politano VA . Significance of asymptomatic bacteriuria in neurogenic bladder disease Urology 1984 23: 343–347
Pearman JW . The value of kanamycin-colistin bladder instillations in reducing bacteriuria during intermittent catheterization of patients with acute spinal cord injury Br J Urol 1979 51: 367–374
Haldorson AM, Keys TF, Maker MD, Opitz JL . Nonvalue of neomycin instillation after intermittent urinary catheterization Antimicrob Agents Chemother 1978 14: 368–370
Murphy FJ, Zelman S, Mau W . Ascorbic acid as urinary acidifying agent. II: Its adjunctive role in chronic urinary infection J Urol 1965 94: 300–303
Stover SL, Fleming WC . Recurrent bacteriuria in complete spinal cord injury patients on external condom drainage Arch Phys Med Rehabil 1980 61: 178–181
Johnson HW et al. A short-term study of nitrofurantoin prophylaxis in children managed with clean intermittent catheterization Pediatrics 1994 93: 752–755
Kevorkian CG, Merritt JL, Ilstrup DM . Methenamine mandelate with acidification: an effective urinary antiseptic in patients with neurogenic bladder Mayo Clin Proc 1984 59: 523–529
Dollfus P, Molé P . The treatment of the paralysed bladder after spinal cord injury in the accident unit of Colmar Paraplegia 1969 7: 204–205
Vivian JM, Bors E . Experience with intermittent catheterization in the southwest regional system for treatment of spinal injury Paraplegia 1974 12: 158–166
Pearman J, Bailey M, Riley L . Bladder instillations of trisdine compared with catheter introducer for reduction of bacteriuria during intermittent catheterization of patients with acute spinal cord trauma Br J Urol 1991 67: 483–490
Galloway A et al. Serial concentrations of Creactive protein as an indicator of urinary tract infection in patients with spinal injury J Clin Pathol 1986 39: 851–855
Allas T, Colleu D, Le Lannon D . Fonction génitale chez l'homme praplégique. Aspects immunologiques Presse Med 1986 29: 2119
Ohl DA et al. Fertility of spinal cord injured males: effect of genitourinary infection and bladder management on results of electroejaculation J Am Paraplegia Soc 1992 15: 53–59
Rutkowski SB et al. The influence of bladder management on fertility in spinal cord injured males Paraplegia 1995 33: 263–266
Orikasa S et al. Experience with non-sterile intermittent self-catheterization J Urol 1976 115: 141–142
Wyndaele JJ, Oosterlinck W, De Sy W . Clean intermittent self-catheterization in the chronical management of the neurogenic bladder Eur Urol 1980 6: 107–110
Maynard FM, Diokno A . Clean intermittent catheterization for spinal cord injured patients J Urol 1982 128: 477–480
Labat JJ et al. L'autosondage intermittent propre dans la réeducation des blesses medullaires et de la queue de cheval II Annales de Réadaptation et de Médicine Physique 1985 28: 125–136
Maynard FM, Glass J . Management of the neuropathic bladder by clean intermittent catheterization: 5 year outcomes Paraplegia 1987 25: 106–110
Webb R, Lawson A, Neal D . Clean intermittent self-catheterization in 172 adults Br J Urol 1990 65: 20–23
Hellstrom P, Tammela T, Lukkarinen O, Kontturi M . Efficacy and safety of clearn intermittent catheterization in adults Eur Urol 1991 20: 117–121
Kuhn W, Rist M, Zach GA . Intermittent urethral self-catheterisation: long term results (bacteriological evolution, continence, acceptance, complications) Paraplegia 1991 29: 222–232
Thirumavalan VS, Ransley PG . Eididymitis in children and adolescents on clean intermittent catheterization Eur Urol 1992 22: 53–56
Perkash I, Giroux J . Clean intermittent catheterization in spinal cord injury patients: a follow up study J Urol 1993 149: 1068–1071
Perrouin-Verbe B et al. Clean intermittent catheterization from the acute period in spinal cord injury patients. Longterm evaluation of urethral and genital tolerance Paraplegia 1995 33: 619–624
Waller L, Jonsson O, Norlén L, Sullivan L . Clean intermittent catheterization in spinal cord injury patients: long-term follow up of a hydrophilic low friction technique J Urol 1995 153: 345–348
Kuhlemeier KV, Lloyd LK, Stover SL . Localization of upper and lower urinary tract infections in patients with neurogenic bladders SCI Digest 1982 336–342
Wyndaele JJ . Chronic prostatitis in spinal cord injury patients Paraplegia 1985 23: 164–169
Cukier J, Maury M, Vacant J, Mlle Lucet . L'infection de l'appareil urinaire chez le paraplégique adults Nouv Presse Med 1976 24: 1531–1532
Günther M, Löchner-Ernst D, Kramer G, Stöhrer M . Intermittent catheterization in male neurogenics: no harm to the urethra Abstract poster 93 presented during Annual Scientific Meeting of IMSOP, Sydney, Australia 2000. Abstract book p 112
Kovindha A, Na W, Madersbacher H . Radiological abnormalities in spinal cord injured men using clean intermittent catheterization with a re-usable silicone catheter in developing country Poster 86 presented during the Annual Scientific Meeting of IMSOP, Sydney, Australia, 2000. Abstract book p 112
Mandal AK, Vaidayanathan S . Management of urethral stricture in patients practising clean intermittent catheterization Int Urol Nephrol 1993 25: 395–399
Vaidyanathan S, Soni BM, Dundas S, Krishnan KR . Urethral cytology in spinal cord injury patients performing intermittent catheterization Paraplegia 1994 32: 493–500
Waller L, Telander M, Sullivan L . The importance of osmolality in hydrophilic urethral catheters crossovers study Spinal Cord 1998 36: 368–369
Michielsen D, Wyndaele JJ . Management of false passages in patients practising clean intermittent self catheterization Spinal cord 1999 37: 201–203
Damanski M . Vesico-ureteric reflux in paraplegics Br J Surg 1965 52: 168–177
Solomon MH, Foff SA, Diokno AC . Bladder calculi complicating intermittent catheterization J Urol 1980 124: 140–141
Amendola MA, Sonda LP, Diokno AC, Vidyasagar M . Bladder calculi complicating intermittent clean catheterization A J Roentgenol 1983 141: 751–753
Morgan JDT, Weston PMT . The disappearing catheter-a complication of intermittent self-catheterization Br J Urol 1990 65: 113–114
Reisman EM, Preminger GM . Bladder perforation secondary to clean intermittent catheterization J Urol 1989 142: 1316–1317
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Wyndaele, J. Complications of intermittent catheterization: their prevention and treatment. Spinal Cord 40, 536–541 (2002). https://doi.org/10.1038/sj.sc.3101348
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101348
Keywords
This article is cited by
-
A scoping review on the impact of hydrophilic versus non-hydrophilic intermittent catheters on UTI, QoL, satisfaction, preference, and other outcomes in neurogenic and non-neurogenic patients suffering from urinary retention
BMC Urology (2022)
-
Prevalence of bacteriuria in cats with neurogenic bladder
Veterinary Research Communications (2022)
-
Catheters for intermittent catheterization: a systematic review and network meta-analysis
Spinal Cord (2021)
-
Improved global response outcome after intradetrusor injection of adult muscle-derived cells for the treatment of underactive bladder
International Urology and Nephrology (2021)
-
Langetermijnresultaten van continent katheteriseerbare urostoma’s bij volwassenen met niet-neurogene of neurogene blaasontledigingsstoornissen
Tijdschrift voor Urologie (2020)