Abstract
Study design: Review and analysis of seven cases of syringomyelia treated surgically.
Objective: To demonstrate the beneficial role of decompressive surgery for the altered cerebrospinal fluid (CSF) flow dynamics in syringomyelia not associated with Chiari I malformation. A comparison between the pre- and post-operative syrinx size and CSF flow in the subarachnoid space was made using cine-mode magnetic resonance imaging (cine-MRI) and then correlated with clinical improvement.
Setting: University Hospital, Seoul, Korea.
Methods: Conventional spinal MRI and cine-MRI were performed in the region of CSF flow obstruction preoperatively in seven patients with syringomyelia not associated with Chiari I malformation. The group consisted of one case of syrinx with post-traumatic compression fracture, one case of post-traumatic arachnoiditis, two cases of holocord syrinx associated with hydrocephalus without Chiari malformation, one case of syrinx with post-traumatic pseudomeningeal cyst, one case of post-laminectomy kyphosis-associated syringomyelia and one case of post-tuberculous arachnoiditis syringomyelia. Based on the preoperative cine-MRI, the types of surgery appropriate to correct the CSF flow obstruction were chosen: decompressive laminectomy-adhesiolysis and augmentation duraplasty in arachnoiditis cases, ventriculoperitoneal shunt for hydrocephalus, cyst extirpation in pseudomeningeal cyst and both anterior and posterior decompression-fusion in the case of post-laminectomy kyphosis. A syrinx-draining shunt operation was performed in three cases; where the syringomyelia was associated with post-traumatic compression fracture refractory to a previous decompression, where hydrocephalus was present in which the decompression by ventriculoperitoneal shunt was insufficient and where post-traumatic arachnoiditis was present in which the decompression was impossible due to diffuse adhesion. Change in syrinx size was evaluated with post-operative MRI in all seven cases and restoration of flow dynamics was evaluated with cine-MRI in three of the cases, two patients with clinical improvement and one patient with no change of clinical status, respectively.
Results: Four out of seven patients showed symptomatic improvement after each decompressive operation. In the remaining three cases, reconstruction of the spinal subarachnoid space was not possible due to diffuse adhesion or was not the main problem as in the patient with syrinx associated with hydrocephalus who had to undergo a shunt operation. One of these three patients showed clinical improvement after undergoing syringosubarachnoid shunt. A decrease of syrinx size was observed in only two out of the five patients who showed clinical improvement after treatment. Of these five patients, two patients underwent post-operative cine-MRI and the restoration of normal CSF flow dynamics was noted in both patients. Of the remaining two patients, one underwent post-operative cine-MRI and there was no change in the CSF flow dynamics evident.
Conclusion: These results suggest that the restoration of CSF flow dynamics between the syrinx and the subarachnoid space by decompressive operation is more effective than simple drainage of the syrinx cavity itself in the treatment of syringomyelia without Chiari malformation.
Similar content being viewed by others
Introduction
Numerous studies have been undertaken in an attempt to elucidate the pathophysiology of syringomyelia. It is now believed that syringomyelia with Chiari malformation is developed as a result of pressure gradient and an aberrant CSF flow in the subarachnoid space at the cervicomedullary junction impacted with cerebellar tonsil.1 However, the majority of previous reports on analysis of CSF flow dynamics in syringomyelia have been limited to cases of Chiari I malformation. In these reports, there has been a focus on the correlation of symptomatic improvement with quantitatively proven normalized flow or value for the velocity of CSF flow at the cervicomedullary junction after posterior fossa decompression.2
Definite treatment modality for syringomyelia other than Chiari malformation has yet to be established, however surgical measures aiming to reconstruct the continuity of the subarachnoid space at the site of the block are strongly recommended. To demonstrate that decompressive surgery results in the same benefits to CSF flow dynamics of syringomyelia patients not associated with Chiari I malformation, we compared both pre and post-operative syrinx size and CSF flow. Both conventional and cine-MRI were used and correlation was made between symptomatic improvement of the patient and increased flow of CSF in the subarachnoid space at suggested obstruction sites.
Material and methods
Clinical material and methods
Seven patients with syringomyelia who were treated surgically between June 1998 and January 2000 were reviewed and analyzed. These patients suffered syringomyelia not associated with Chiari malformation. Of the seven, there was one case of syrinx with post-traumatic compression fracture, one case of post-traumatic arachnoiditis, two cases of holocord syrinx associated with hydrocephalus without Chiari malformation, one case of post laminectomy kyphosis-associated syringomyelia, one case of syrinx with an associated post-traumatic pseudomeningeal cyst and one case of post-spondylitic (tuberculous) arachnoiditis-associated syringomyelia. There was one female and six male patients, age from 18 to 55 years (mean, 34.4). The extent of syringomyelia in these patients varied. Patients suffered syringomyelia in several levels of the thoracic spine and in extreme cases, suffered holocord syrinx (Table 1).
Change in the syrinx size and restoration of flow dynamics was evaluated with post-operative MRI in all seven cases and cine-MRI in three out of the seven cases. Of those patients evaluated with cine-MRI, two patients showed signs of clinical improvement and one patient had no change in their clinical status (Table 2). Imaging techniques used were the conventional spinal MRI and the midsagittal cardiac-gated phase-contrast cine-MRI at the obstruction site. Imaging was performed on a 1.5-T Signa Advantage scanner (General Electric, Milwaukee, WI, USA) both before and after surgery with the same scanning parameters. Scan parameters for cine-MRI included a TR of 5–100 ms; a TE of 8.9 ms; a field of 230×270 mm; a matrix of 168×256; a flip angle of 12–15 degrees; 16 frames/one cardiac cycle; encoding velocity of 6–12 mm/s. Then the 16 velocity-encoded images were arranged in a cine loop. The follow-up period ranged from 4 months to 26 months (average 13.6 months) and follow-up images were taken at 3 to 6 months interval after each operation on a regular basis.
Surgical methods
Based on the pre-operative cine-MRI, the types of surgery required to correct the subarachnoid CSF flow obstruction was decided upon: decompressive laminectomy-adhesiolysis and augmentation duraplasty in post-traumatic compression fracture-associated or post-tuberculosis arachnoiditis associated syringomyelia, ventriculoperitoneal shunt for hydrocephalus, cyst extirpation for the pseudomeningeal cyst and both anterior and posterior decompression-fusion for the post-laminectomy kyphosis. A syrinx-draining shunt operation was performed in three cases; one case of syringomyelia associated with post-traumatic compression fracture refractory to the initial decompression, one case of hydrocephalus in which the decompression by ventriculoperitoneal shunt was insufficient and one case of post-traumatic arachnoiditis in which the decompression was impossible due to diffuse adhesion (Table 2).
Results
Results of this study are summarized in Tables 1 and 2. Four out of seven patients (57%) showed improvement of symptoms after initial decompression. In the remaining three cases, reconstruction of the spinal subarachnoid space was not possible due to diffuse adhesion or was not the main problem, for instance where there was syrinx associated with hydrocephalus. These three patients underwent a shunt operation. One of the three patients showed signs of clinical improvement after the shunt procedure. None of the patients above underwent further decompression beyond the suggested obstruction site. Among the five patients who showed improvement, only two patients (40%) showed a decrease in syrinx size after the initial decompression or shunt operation on the regular follow-up MRI studies. These two patients were the patient with post-laminectomy kyphosis and one of the patients with hydrocephalus. From the original seven, the remaining two patients exhibited refractory clinical signs. After repeated shunt operations, one of these patients showed a collapsed syrinx, while the other patient showed no change in syrinx size. Follow-up cine-MRIs were performed on two patients out of the five who showed signs of clinical improvement and on one of the two patients where refractory syringomyelia was seen. The former group showed improved CSF flow at the operation site as expected, while the latter showed no definite change. Of the two patients with CSF flow improvement at the operation site, one patient demonstrated accompanying syrinx size decrease, whilst the other patient showed no change in syrinx size.
Illustrative cases
Case 2
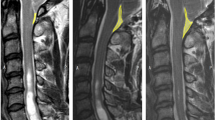
A 26-year-old male patient presented with paraparesis and hypesthesia of both lower extremities, with onset of symptoms 2 years prior. He had suffered from right lower extremity monoparesis 11 years prior and had undergone both C4 and C5 laminectomy and also removal of the tumor after diagnosis of neurofibromatosis. Simple cervical spinal X-ray on current admission showed kyphosis at the previously operated level and cervical MRI revealed stenosis of neural foramen at C4 and C5 level with syringomyelia extending from C2 to T2 level. Phase-contrast cine-MRI showed obstructed CSF flow in both the ventral and dorsal subarachnoid space at the stenotic level (Figure 1). Initial treatment was interbody fusion from C4 to C6 using autologous iliac bone graft with an anterior cervical plate and screw in order to decompress the ventral subarachnoid space. Both cervical MRI and cine-MRI were performed four months after the first operation. They revealed a greatly decreased size of syrinx and also revealed active CSF flow at the previously stenotic spinal level along with corrected alignment of cervical vertebrae (Figure 1). Seven months later, posterior fusion was performed at the same level to achieve rigid stabilization of the spine. The patient showed good recovery from his deficits 1 year after discharge on routine follow-up.
(a) T2-weighted sagittal view of cervical MRI shows syringomyelia in high-signal intensity from cervicomedullary junction to upper thoracic spine level (small arrows) with kyphotic change (large arrow) and interrupted subarachnoid space (arrowheads) at C4 and C5 level. (b) Phase-contrast mid-sagittal view of cine-MRI shows interrupted CSF flow at the C4 and C5 level (arrowheads). Faint communicating flow in the syrinx is (small arrow) also noted. (c) T1-weighted sagittal view of cervical MRI after anterior cervical interbody fusion shows metallic artifact from C4 to C6 level (arrowheads) with decreased size of syrinx (small arrows). It also reveals the previous operation site artifact (large arrow) and the cervical spine alignment is still kyphotic. (d) The cine-MRI shows improved flow of CSF (arrows) especially at the ventral subarachnoid space. Flow in the syrinx is now almost absent. (e) T1-weighted sagittal view of cervical MRI after posterior fusion shows further decreased size of syrinx especially at the lower cervical level (small arrows) and almost corrected alignment of cervical spine. Metallic artifact after the second operation (large arrow) is also revealed
Case 4
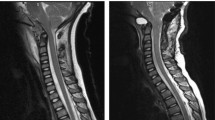
A 38-year-old male patient visited with sphincteric change and paraparesis with onset of symptoms 5 years prior. The patient suffered from similar symptoms after sustaining injury to his back whilst playing soccer 14 years before. One year later, he was diagnosed as having post-traumatic arachnoiditis and underwent a partial hemilaminectomy and adhesiolysis from T10 to T12 level. The patient managed well until he experienced defecation difficulty 5 years ago. Thoracolumbar MRI and cine-MRI on admission revealed diffuse syrinx extending from T6 to L2 interrupted at T10, 11 level (Figure 2) and also revealed diffusely obstructed CSF flow in the subarachnoid space at the lower thoracolumbar level including the previously operated site. Initial treatment was T8 to T10 bilateral total laminectomy and syringo-subarachnoid shunt to decompress the upper level syrinx and subarachnoid space. Subsequent treatment one week later involved L2 left partial hemilaminectomy and syringo-subarachnoid shunt as the extent of adhesion was so wide especially at the previously operated level that additional adhesiolysis was thought to be both impossible and insufficient. Ten months later, a further syringoperitoneal shunt at L1 level was performed since the lower level syrinx showed itself to be inadequately decompressed on imaging, suggesting shunt malfunction (Figure 2). Further follow-up imaging 15 months later revealed a decreased size of syrinx at both levels (Figure 2) however cine-MRI still revealed interrupted flow of CSF at the T10 to T12 level. The patient exhibited mild clinical improvement especially in terms of sphincteric changes but his paraparesis persisted.
(a) T1-weighted sagittal view of thoraco-lumbar MRI shows the extent of syringomyelia to be diffuse, from upper thoracic to conus level (small arrows) with interruption at T9 to T12 level which is also the previous operation site (large arrows). The dorsal subarachnoid space seems to be almost obliterated. (b) T1-weighted sagittal view of thoraco-lumbar MRI after shunt operation on both levels of syrinx shows decreased size of syrinx (arrows) especially at the upper thoracic level. (c) T1-weighted sagittal view of thoraco-lumbar MRI ten months after shunt operation shows increased size of syrinx at lower lumbar level (arrows) suggesting shunt malfunction. (d) T1-weighted sagittal view of thoraco-lumbar MRI after shunt revision on lower lumbar level syrinx shows an almost collapsed syrinx at both upper and lower levels
Discussion
In the management of syringomyelia, understanding of the pathophysiology and CSF flow dynamics is indispensable. The assumption was made that syringomyelia with Chiari I malformation is propagated by anatomical and physiological block of CSF flow at the cervicomedullary junction by herniated cerebellar tonsil. The cerebellar tonsil then acts as a piston on the partially closed cervical subarachnoid space, enlarging cervical subarachnoid space pressure and then compressing the spinal cord from without to propagate the syrinx fluid caudally. The optimal surgical management to eliminate this mechanism and to reduce the syrinx was proposed to be a procedure that could expand the CSF pathway at the foramen magnum: posterior fossa decompression, upper cervical laminectomy and augmenting duraplasty.1 Phase contrast cine-MRI made it possible to evaluate the altered cerebrospinal fluid dynamics in patients with Chiari I malformations. Postoperative changes in CSF flow profiles included an increase in velocity magnitude and a change in the direction of flow from a previously constricted posterior fossa.2
The majority of previous studies of the pathophysiology of syringomyelia have been limited to Chiari I malformation and succeeded in establishing optimal treatment strategies. In order to decide the most optimal treatment strategies for syringomyelia not associated with Chiari I malformation, it is essential to understand the various causes of CSF flow interruption, the level at which the spine is most severely obstructed and the degree of deleterious effect of syringomyelia on the neurologic deficit of the patient.3 If the same pathophysiological changes are the cause of syringomyelia not associated with Chiari I malformation, normalization of the CSF flow in the subarachnoid space at the suggested obstruction level may be preferred over simple drainage of the syrinx fluid.4,5,6 Once the suggested obstruction site has been defined by conventional MRI study, the performance of phase contrast cine-MRI on the level of the obstruction may provide information about CSF flow and pulsation in both syrinx cavity and subarachnoid space. This valuable information may allow for the selection of the optimal surgical management. Postoperative improvement of CSF dynamics could then be qualitatively evaluated by the restoration of active flow at the operation site.
Beyond qualitatively assessed improvement, the aim was to correlate the recovery of CSF flow with the symptomatic improvement of the patient and also with a decreased syrinx size. In Chiari malformation, the symptoms and signs of the patients are known to be related to the degree of herniation, abnormal configuration of the tonsil and upper cervical spinal cord or to the associated extent of syrinx. Anatomical repositioning of the tonsil, normalization of abnormal CSF flow profiles after foramen magnum decompression or decompression of syrinx itself might explain the clinical improvement of the patients.1 In the syringomyelia other than Chiari malformation, a similar but simpler concept is applied as there is no tonsillar herniation or complicating mechanism of syrinx propagation associated with it. There remains CSF flow obstruction and pathological change to the subarachnoid space, such as arachnoid adhesion or scarring, at the lesion site, either of which is the cause of the syringomyelia.5 Therefore when the anatomical distortion or the pathological process has been reversed, as in the case of subarachnoid space decompression, it may be anticipated that there will be normalization of the CSF flow dynamics, decrease in syrinx size and then symptomatic relief for the patient in sequence.5,6
Experimental results showed only minimal changes in the size of the syrinx despite clinical improvement in most of the patients.7 Where a constricted, adhered subarachnoid space around the cord parenchyma is the main problem, as in most of our cases, then the subarachnoid space decompression is sufficient for recovery of the altered CSF flow, release of the cord parenchyma and reversal of the symptoms and signs.5 The cord parenchyma is sufficiently decompressed even though its central canal is still dilated, as in case 5 of this study. The syrinx itself or the extent of the syrinx might be the next process which can or cannot be reversed after initial management but has only a secondary effect on the patient's clinical status. This suggestion about the relative importance of syrinx size may explain the persistence of paraparesis in case 4 even after decrease in syrinx size. In this case, a direct syrinx draining shunt operation was performed, as adhesiolysis was impossible due to the diffuse arachnoiditis-associated adhesion. The shunt operation succeeded in reducing the size of syrinx but failed to produce any notable improvement in the patient's clinical status as the initial pathological change of adhesion by arachnoiditis was not corrected.4,7 Alternatively if overfilling of the central canal is the main problem, as in cases 1 and 6 of this study where hydrocephalus is associated without any causative obstruction of flow, then drainage of the syrinx itself or from the ventricle is mandatory for treatment.3 In these cases, what must be kept in mind is that there are some serious disadvantages to the drainage procedure, including delayed shunt malfunction, shunt tube displacement and spinal cord damage attributable to myelotomy or insertion of the shunt tube.6,8
To the best knowledge of authors, this is the first study of the role of reconstruction of the spinal subarachnoid space in patients with syringomyelia not associated with Chiari malformation. A correlation was made between a change in the clinical status of the patient and the follow-up imaging studies, particularly cine-MRI. It is suggested, after thorough review of this information that the most important consideration is the reversal of the pathological mechanism of CSF alteration rather than a simple decrease in the extent of the syrinx. Even though a syrinx may decrease in size after a shunting procedure, the symptoms may not improve due to irreversible neuronal/axonal damage – not necessary due to inadequate therapy. Likewise, there may be clinical improvement without a change in the syrinx size. Individual clinical improvements in each patient was directly related to the subarachnoid space reconstruction, and only minimally to a change in the syrinx size.
The scope of this study was limited by a small number of patients and also by the limited performance of the postoperative follow-up cine-MRI. More patients with standardized preoperative and postoperative evaluation, as well as a longer follow-up, would be helpful to provide a more convincing argument.
Conclusion
The postoperative increase in CSF flow in the subarachnoid space at the lesion site mirrored the improvement of patient symptoms in syringomyelia. The reduction of the size of syrinx did not account for clinical improvements. These outcomes suggest that the restoration of CSF flow dynamics between the syrinx and the subarachnoid space by decompressive operation is more effective than simply draining the syrinx cavity itself in the treatment of syringomyelia without Chiari malformation.
References
Heiss JD et al. Elucidating the pathophysiology of syringomyelia J Neurosurg 1999 91: 553–562
Armonda RA, Citrin CM, Foley KT, Ellenbogen RG . Quantitative cine-mode magnetic resonance imaging of Chiari I malformations: an analysis of cerebrospinal fluid dynamics Neurosurgery 1994 35: 214–223
Milhorat TH et al. Surgical treatment of syringomyelia based on magnetic resonance imaging criteria Neurosurgery 1992 31: 231–244
Goel A, Desai K . Surgery for syringomyelia: an analysis based on 163 surgical cases Acta Neurochi (Wien) 2000 142: 293–301
Klekamp J, Batzdorf U, Samii M, Bothe HW . Treatment of syringomyelia associated with arachnoid scarring caused by arachnoiditis or trauma J Neurosurg 1997 86: 223–240
Sougoros S, Williams B . Management and outcome of postraumatic syringomyelia J Neurosurg 1996 85: 197–205
Sgouros S, Williams B . A critical appraisal of drainage in syringomyelia J Neurosurg 1995 82: 1–10
Iwasaki Y, Hida K, Koyanagi I, Abe H . Reevaluation of syringosubarachnoid shunt for syringomyelia with Chiari malformation Neurosurgery 2000 46: 407–412
Acknowledgements
This work was supported in part by a grant from the Seoul National University Hospital Research Fund.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lee, JH., Chung, CK. & Kim, H. Decompression of the spinal subarachnoid space as a solution for syringomyelia without Chiari malformation. Spinal Cord 40, 501–506 (2002). https://doi.org/10.1038/sj.sc.3101322
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101322
Keywords
This article is cited by
-
Treatment of posttraumatic syringomyelia: evidence from a systematic review
Acta Neurochirurgica (2020)
-
Post-traumatic syringomyelia with holocord involvement: a case report
Spinal Cord Series and Cases (2017)
-
Surgical management of syringomyelia unrelated to Chiari malformation or spinal cord injury
European Spine Journal (2016)
-
New surgical approach for late complications from spinal cord injury
BMC Surgery (2006)
-
Holocord myelopathy with thoracic stenosis: case report and hypothesis
Spinal Cord (2003)