Abstract
Study design: A case report.
Objective: To present and discuss the case of a patient with serious head and spinal injuries who suffered delayed haemorrhage from a post-traumatic aneurysm of the right posterior inferior cerebellar artery following surgical treatment of vertebral fracture and hydrocephalus.
Setting: National Spinal Injuries Unit and Institute of Neurological Sciences, Southern General Hospital, Glasgow, Scotland, UK.
Methods: Clinical and radiological follow-up of the patient.
Results: The aneurysm was treated by coil occlusion of the right vertebral artery. Post-operative films showed that the aneurysm had been successfully obliterated.
Conclusion: Post-traumatic cerebral aneurysms are very rare. Neurosurgical and rehabilitation teams need to be aware of this late treatable sequela of head injury.
Similar content being viewed by others
Introduction
Reported incidence of the association of spinal injuries with other injuries is around 50%, with head injury being the commonest associated injury.1 While managing acute spinal injuries, it is important to remain alert to the development of complications from other injuries, which could prejudice the patient's recovery. We describe the case of a young girl with serious head injury and traumatic paraplegia who developed delayed subarachnoid and intraventricular haemorrhages from a post-traumatic aneurysm of the right posterior inferior cerebellar artery.
Case Report
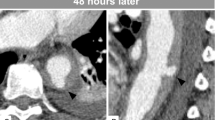
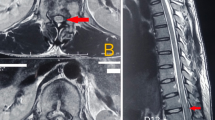
A seventeen-year old girl was admitted to hospital with a history of a fall from a height of approximately thirty feet. A Glasgow Coma Scale (GCS)2 (Table 1) of six was documented at the scene of the accident (E2,V2,M2), which had improved to nine (E3,V3,M3) on admission to the Accident and Emergency department, and to fourteen (E3,V5,M6) on admission to the regional neurosurgical unit. She had sustained a burst fracture of the seventh thoracic vertebra and was paraplegic below that level. She also had a Battle's sign (discoloration over the skin of the mastoid region in the line of the posterior auricular artery, seen in fracture of the base of the skull) on the right side with cerebrospinal fluid (CSF) otorrhoea. Computed tomography (CT) scan showed a depressed fracture of the right occipital bone and a linear fracture of the right temporal bone with a small contusion in the posterior temporal area associated with sub-arachnoid haemorrhage (SAH), and a small sub-dural haemorrhage in the middle cranial fossa. Although complicated by agitation and occasional delirium, her GCS remained stable at fourteen/fifteen. Repeat CT scan 4 days later did not show any progression of intra-cranial pathology. She was transferred to the national spinal injuries unit, where her thoracic fracture was surgically stabilised 12 days after injury.
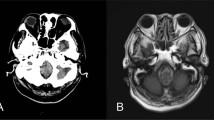
She started complaining of a frontal headache 14 days following injury, which gradually worsened over the next 5 days, with associated nausea, vomiting, and increasing drowsiness. Repeat CT scan showed gross hydrocephalus. A ventriculo-peritoneal shunt was inserted followed by a rapid improvement in consciousness (GCS 15). However, 2 days following that operation, rapid deterioration in her consciousness occurred (from GCS 15 to GCS 4). The valve of the shunt was patent and blood stained CSF was aspirated. Repeat CT scan showed widespread intra-ventricular bleeding. Cerebral angiogram showed an irregular 10 millimetre aneurysm at the origin of the right posterior inferior cerebellar artery (PICA) (Figure 1). The aneurysm was treated by coil occlusion of the right vertebral artery. Post-operative films showed non-filling of the aneurysm while the entire basilar arterial system was shown to be patent after contrast injection into the ipsilateral carotid artery. The patient's conscious level improved post-operatively. She had a weak right upper limb, which was not present before insertion of the coil. Muscle power in her right upper arm was MRC grade 3, the weakness was of upper motor neuron type.
Six months after injury the patient was mobilising in a wheelchair. She has not had any further neurological deterioration, but the ventricular shunt needed revision. No further episodes of cerebral haemorrhage occurred.
Formal neuropyschological testing 6 months after injury showed no intellectual or personality deficits. She remains alert and fully oriented and underwent successful rehabilitation for her spinal injury.
Discussion
The development of a post-traumatic cerebral aneurysm is a recognised complication of serious head injury, but one involving the PICA is extremely rare.3,4,5 The commonest presenting symptom of these aneurysms is rapid neurological deterioration following a delayed acute intra-cranial haemorrhage6 as seen in this patient. Arteriography remains the best diagnostic procedure,7 but indications remain controversial.
The angiographic features of traumatic aneurysms include: irregular sac contour, absent neck, peripheral location and delayed emptying and filling.8 Friedman and Drake was the first to describe safe and effective means of parent vessel sacrifice by surgical means to treat intra-cranial pseudoaneurysm.9 Recently less invasive techniques using endovascular coils have become well established.10,11 Because of the need to sacrifice the parent vessel, there is a significant risk of new neurological deficit following treatment.10,11
In both of the previously reported cases of post-traumatic PICA aneurysms associated with skull fractures the angiograms were performed on the basis of strong clinical suspicion.3,4 One patient had an `unusual pattern' of post-traumatic intra-cranial bleeding and the other had a skull fracture with intraventricular bleeding. The combination of sudden delayed deterioration in consciousness and intraventricular bleeding led us to suspect an arterial source of bleeding in our patient.
The proximity of the spinal injuries unit to the regional neurosurgical centre sited in the same building facilitated the early diagnosis and treatment of this aneurysm in our patient. The outcome may have been different if she had been transferred to a more remote rehabilitation unit before the aneurysm bled. We suggest that those looking after patients recovering from acute brain injury should be aware of this rare complication as a possible cause of delayed intracerebral haemorrhage.
References
Saboe LA et al. Spine trauma and associated injuries J Trauma 1991 31: 43–48
Teasdale G, Jennett B . Assessment of coma and impaired consciousness: a practical scale Lancet 1974 2: 81–84
Meguro K, Rowed DW . Traumatic aneurysm of the posterior inferior cerebellar artery caused by fracture of the clivus Neurosurgery 1985 16: 666–668
Morard M, de Tribolet N . Traumatic aneurysm of the Posterior Inferior Cerebellar Artery: Case Report Neurosurgery 1991 29: 438–441
Schuster JM et al. Acute traumatic posterinferior cerebellar artery aneurysms: report of three cases Neurosurgery 1999 45: 1465–1467
Buckingham MJ et al. Traumatic intra-cranial aneurysms in childhood. Two cases and a review of the literature Neurosurgery 1988 22: 398–408
Haddad FS, Haddad GF, Taha J . Traumatic intracranial aneurysms caused by missiles: their presentation and management Neurosurgery 1991 28: 1–7
Tani S et al. Traumatic aneurysm of the posterior inferior cerebellar artery No Shinkei Geka 1982 10: 423–427 Japan
Friedman AH, Drake CG . Subarachnoid haemorrhage from intra-cranial dissecting aneurysm J Neurosurg 1984 60: 325–334
Eckard DA et al. Coil occlusion of the parent artery for treatment of symptomatic peripheral intracranial aneurysms Am J Neuroradiol 2000 21: 137–142
Ishikawa E et al. Treatment of peripheral aneurysms of the posterior circulation No Shinkei Geka 2000 Apr 28: 337–343 Japan
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hossain, M., Brown, J., McLean, A. et al. Delayed presentation of post-traumatic aneurysm of the posterior inferior cerebellar artery in a patient with spinal cord injury. Spinal Cord 40, 307–309 (2002). https://doi.org/10.1038/sj.sc.3101290
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101290
Keywords
This article is cited by
-
Subarachnoid haemorrhage secondary to traumatic intracranial aneurysm of the posterior cerebral circulation: case series and literature review
Acta Neurochirurgica (2016)
-
Delayed post-traumatic saccular aneurysm of PICA in an adolescent
Acta Neurochirurgica (2009)