Abstract
Study design: Before-After trial measured prior to cold air therapy, immediately following, after 30 and 60 min.
Objective: To determine the effect of cold air therapy in relieving spasticity, the optimal intramuscular temperature, and the duration of spasticity relief attained by cold air therapy.
Setting: Clinical research laboratory, Seoul, Korea.
Subject: Forty-six spastic paraplegic rabbits with spinal cord injury.
Methods: Spastic paraplegia was induced by transection of spinal cord in 46 rabbits. Cold air was applied to triceps surae muscles for 30 min at three different intramuscular temperatures (25, 30 and 32.5°C). Clinical parameters of spasticity (muscle tone, Babinski's sign, muscle stretch reflex and ankle clonus) and electrophysiologic parameters (F/M ratio and H/M ratio) were measured immediately following, after 30 and 60 min.
Results: In the 32.5°C group, relief in spasticity lasted less than 30 min. In the 30 and 25°C groups, the decrease in spasticity lasted for at least 30 min clinically. The spasticity relief was observed only immediately following treatment when measured electrophysiologically. However, six out of 16 cases (37.5%) in the 25°C group showed complete motor conduction block.
Conclusion: To relieve spasticity with cold air therapy, the intramuscular temperature should be maintained at 30°C. The duration of spasticity relief lasted from between 30–60 min after cold air therapy.
We certify that all applicable institutional and governmental regulations concerning the ethical use of animals were followed during the course of this research.
Similar content being viewed by others
Introduction
Spasticity is a condition of exaggerated spinal and brain stem reflexes due to upper motor neuron disease that results in increased muscle stretch reflex, ankle clonus, increased muscle tone, and involuntary spasms.1 Spastic patients suffer from muscle contracture, muscle cramp with pain, and involuntary movement of the limbs. Spasticity also interferes with the gait, exercise, and range of motion of joints. Twenty-one per cent of spinal cord injury patients have been reported to show involuntary and uncontrollable movement that is attributed to spasticity.2
Local application of cold is used clinically to diminish the resistance of spastic muscle to rapid stretching and to decrease or abolish clonus.3 Cold can be applied to the body in three different ways: immersing in cold water, rubbing with ice cubes or ice packs or using evaporative sprays such as ethyl chloride. Immersing part of body in cold water is limited because it is difficult to apply to large area of the body. In patients who do not have a sitting balance, applying this treatment to the lower extremities is difficult. Rubbing with ice cubes or packs is not applicable to patients with cold hypersensitivity. Cold air therapy with evaporative agents can be applied without direct skin contact, and can induce an abrupt decrease in temperature. However, it is impossible to apply cold with evaporative agents for longer than 10 min. A recently developed cold air therapy machine, which directly decreases the air temperature by passing air through dry ice, can be applied when continuous application for longer than 10 min is required.
The application of cryotherapeutic techniques to alleviate spasticity is well known.4,5,6,7,8,9,10 Miglietta11 demonstrated that 35 of 40 spastic patients had their clonus alleviated after 30 min of cold application. Knutsson and Mattsson12 found a reduced stretch reflex of the Achilles tendon following muscle cooling. However, these studies used either dipping or rubbing as the method of application. To our knowledge, there has been no study performed with the continuous application of cold air therapy.
The purpose of this study is to determine the effect of continuous cold air therapy in relieving spasticity, and to determine the adequate therapeutic temperature and how long the effect of treatment lasts. To accomplish this, spasticity in rabbits was induced through dissection of the spinal cord and cold air therapy was applied to the triceps surae muscles with three different target temperatures.
Methods
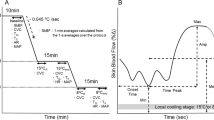
A pilot study to determine intramuscular temperature
According to literatures, if a hand is put into water at 18°C or lower, aching pain occurs in a few seconds.13 As a pilot study to determine the intramuscular temperatures, cold air therapy (Cold Air, Model HC-100, OG Gikken, Japan) was applied to triceps surae muscles of two rabbits from a distance of 10 cm above the skin surface for 1 h. The skin temperature and intramuscular temperature 1.5 cm deep in the triceps surae muscle were monitored with a digital thermometer (Model 2455, Yokogawa Corp, Singapore) every 2 min for 10 min, every 5 min for the next 20 min and every 10 min for another 30 min. From this pilot study, a graph showing the changes of the skin and intramuscular temperature with continuous application of cold air was generated (Figure 1).
As shown in Figure 1, when the skin temperature was 18.7°C, the intramuscular temperature was 30°C. From these data, we decided to divide the rabbits into three groups in which the cold air would be applied to maintain three different intramuscular temperatures, ie 32.5, 30 and 25°C.
Experimental animals
Forty-six lower extremities of New Zealand White Rabbits of either sex at an age of 4 months and weight ranging from 2 to 3 kg were included in the study. They were divided into three groups and in each group, cold air therapy was applied to maintain three different intramuscular temperatures, ie 32.5, 30 and 25°C. The numbers in each group were 16, 14, and 16, respectively. All animals were handled and cared in accordance with guidelines of ‘Seoul National University Hospital Clinical Research Institute’.
Operative procedures
All animals were anesthetized with intraperitoneal pentobarbital sodium (40 mg/kg), and intubated. Supplemental anesthesia was given intravenously, if needed through a cannulated femoral vein. In the prone position, a midline skin incision was made from T6 to the T10 spinous processes. The muscles attached to the spinous process and lamina of T8 and T9 vertebrae were separated from the bone by blunt dissection with a periosteal elevator. The spinous processes of the T8 and T9 vertebrae were removed with a large clamp. A small hole was drilled into the posterior lamina of the exposed spine and widened with a rongeur so that an entire width of the spinal cord could be visualized. After the visual verification that the portion of the exposed spine was the spinal cord but not cauda equina, the exposed spinal cord was transected with a No. 11 surgical knife and the proximal and distal end of the dissected spinal cord was interposed with a small piece of gauze.
Intravenous fluid was supplied for 24 h following operation, and antibiotics were injected intramuscularly every 8 h for 3 days. The resultant retention of urine was drained with the Crede maneuver every 8 h. A physical examination was performed everyday to determine the manifestation of spasticity.
Measurement of spasticity
The measurement of spasticity was performed using the clinical parameters such as muscle tone, muscle stretch reflex, ankle clonus, and Babinski's sign, and electrophysiological parameters such as the ratio of amplitude of the F wave to the amplitude of the compound motor unit action potential (CMAP); F/M ratio and the ratio of the amplitude of the H reflex to the amplitude of the CMAP; H/M ratio. The triceps surae muscle tone was measured using a modified Ashworth scale.14 The patella tendon reflex was graded as follows: grade 0; no reflex activity, grade 1; decreased reflex, grade 2; normal reflex, grade 3; increased reflex without pathologic reflex such as ankle clonus, grade 4; presence of pathologic reflex. The ankle clonus and Babinski's sign were measured using a grading system as described in Table 1.
For electrophysiologic parameters, Mystro PLUS EMG machine (Mystro Plus, Medelec, UK) was used. The F wave was recorded with disc type surface electrode at the abductor hallucis muscle and the posterior tibial nerve was stimulated at the ankle with a needle electrode. The stimulation frequency was 0.5 Hz and the mean amplitude of 10 evoked F waves was used for the amplitude of F wave. The amplitude of the CMAP was measured. The H reflex was recorded with a disc type surface electrode at the triceps surae muscle with stimulation of the posterior tibial nerve at the popliteal fossa using a needle electrode. The stimulation frequency was 0.3 Hz and duration of the stimulation was 0.5 ms. Maximum amplitude of five evoked H reflexes was obtained. The amplitude of the CMAP was also measured. For the purpose of determining the effect of cold air on conduction of nerve fibers, the CMAP was recorded at the abductor hallucis muscle with a surface electrode. Sciatic nerve at the hip which is proximal to the site of cold air application was stimulated with needle electrodes.
Application of cold air therapy
With the needle electrode of the digital thermometer placed 1.5 cm deep into the triceps surae muscle, cold air was applied at three different intramuscular temperatures, 32.5, 30 and 25°C in each group from a distance of 10 cm above the surface of the skin. The application of cold air was performed intermittently to maintain the target intramuscular temperature in each group. The operator of the cold air therapy machine put the applicator to or away from the treatment site so that the intramuscular temperature was maintained in less than 0.5°C above or below the target temperature. The duration of treatment was 30 min. Changes of spasticity were measured prior to, immediately following, 30 and 60 min after the treatment.
Data analysis
The Ashworth scales and electrophysiological parameters immediately following treatment, 30 and 60 min after treatment were compared with those of before treatment in each treatment group. The Ashworth scales before and after the treatment were compared with Wilcoxon signed-rank test and the electrophysiological parameters were compared with the pre-treatment data using a paired t-test in each treatment group. By comparing the effect of cold air in each group, we first sought to determine the effective treatment temperature. Then, the differences between baseline and after treatment were compared with Wilcoxon signed-rank test (Ashworth scale) and paired t-test (electrophysiological parameters) or with ANOVA test according to the numbers of groups that showed significant changes after treatment. By comparing the difference of treatment effect in the groups, we tried to seek the optimal intramuscular temperature that can satisfy the criterion of maximum treatment effect and minimum side or toxic effects. All the statistical tests were performed using an SPSS statistical program (SPSS Inc, ver 10.0.1, Chicago, IL, USA).
Results
Manifestation of spasticity
Spasticity was manifested between 1 and 3 days after spinal cord dissection. Treatment was performed between 7 and 10 days after the procedure.
Changes of intramuscular temperature
In the group where the intramuscular temperature was 32.5°C (32.5°C group), the intramuscular temperature was 35.9°C before the treatment, 32.5°C immediately following treatment, 35.8°C at 30 min after the treatment, and 35.8°C at 60 min after the treatment. In the group where the intramuscular temperature was maintained at 30°C (30°C) group), the intramuscular temperatures were 35.9, 30.1, 35 and 35.8°C, respectively. In the group with an intramuscular temperature maintained at 25°C (25°C group), the temperatures were 35.8, 25.2, 32.9 and 35.7°C, respectively.
Changes of clinical parameters (Table 2)
Muscle tone
In the 32.5°C group, muscle tone decreased immediately following treatment from a 2.2±0.6 grade to a 1.9±0.5 grade. The decrease in muscle tone was maintained for less than 30 min after treatment. In the 30 and 25°C group, muscle tone decreased significantly immediately following treatment and was maintained until 30 min after treatment. Sixty minutes after treatment, mean value of muscle tone was less than the pre-treatment value but there was no statistical significance. The decreases in muscle tone immediately following treatment was significant in the 30 and 25°C groups when compared to the 32.5°C group. There was no statistically significant difference in the changes of muscle tone 30 min after the treatment between the 30 and 25°C groups.
Muscle stretch reflex
In the 32.5°C group, the grades of muscle stretch reflexes decreased immediately following the treatment from the 2.9±0.2 grade to the 2.5±0.5 grade. The decrease in muscle stretch reflex returned to the pre-treatment value when measured 30 min after treatment. In the 30°C group, the reflex decreased immediately following treatment from the 2.9±0.2 grade of pre-treatment value to the 1.1±0.9 grade. The decrease in reflex was maintained until 30 min after treatment (1.7±0.7). At 60 min after treatment, the muscle stretch reflex returned to its pre-treatment value. In the 25°C group, the decrease in muscle stretch reflex was maintained for at least 60 min after treatment. The muscle stretch reflex decreased more in the 30 and 25°C groups than in 32.5°C group immediately following treatment. There was no statistically significant difference in the changes of muscle tone 30 min after the treatment between the 30 and 25°C group.
Ankle clonus
In the 32.5°C group, ankle clonus decreased immediately following treatment from the 1.6±0.5 grade to the 1.1±0.4 grade. The decrease in muscle stretch reflex had returned to its pre-treatment value when measured 30 min after treatment (1.4±0.5). In the 30°C group, the decrease in ankle clonus was maintained when measured 30 min after treatment. Sixty minutes after treatment, the muscle stretch reflex returned to its pre-treatment value. The 25°C group showed a decrease in muscle stretch reflex, which was maintained for at least 60 min after treatment. In the 30 and 25°C groups immediately following treatment, ankle clonus decreased more than in the 32.5°C group. There was no statistically significant difference in the changes of muscle tone between the 30 and 25°C groups 30 min after the treatment.
Babinski sign
In the 32.5°C group, the Babinski sign decreased immediately following treatment. The decrease had returned to its pre-treatment value when measured 30 min after treatment. In the 30°C group, the Babinski sign had decreased immediately following treatment from a pre-treatment value of 1.8±0.4 to 0.1±0.3. The decrease in reflex was maintained until 30 min after treatment (0.7±0.7). Sixty minutes after treatment, the muscle stretch reflex returned to its pre-treatment value. In the 25°C group, the decrease in muscle stretch reflex was maintained when measured 30 min after treatment but returned to its pre-treatment value 60 min after treatment. Babinski sign decreased more in the 30 and 25°C group compared to the 32.5°C group immediately following treatment. But there was no statistically significant difference in the changes of muscle tone between the 30 and 25°C groups 30 min after the treatment.
Changes in electrophysiologic parameters (Table 3)
F/M ratio
In the 32.5°C group, the F/M ratio showed no change with treatment. In the 30°C group, the ratio decreased immediately following treatment (from 13±6 to 10±6%, P<0.05). The decrease in F/M ratio was not maintained when measured 30 min after treatment. In the 25°C group, the ratio decreased from 13±8 to 3±1% immediately following treatment. The ratio had returned to its pre-treatment value in 30 min. When compared between the 25 and 30°C groups, the F/M ratio decreased significantly more in 25°C group.
H/M ratio
In the 32.5°C group, the H/M ratio showed no change with treatment. In the 30°C group, the ratio decreased immediately following treatment (from 16±10 to 9±6%, P<0.05) but returned to its pre-treatment value when measured 30 min later. In the 25°C group, the ratio decreased from 14±11 to 5±4% immediately following treatment and returned to its pre-treatment value after 30 min. The H/M ratio decreased more in the 25°C group than the 30°C group.
Changes of compound motor unit action potential (CMAP) (Table 4)
Latency
In the 32.5°C group, the CMAP latency showed no statistically significant change with treatment. In the 30°C group, the latency increased 25.4% immediately following treatment (from 5.9±1.0 milliseconds (ms) to 8.4±1.1 ms, P<0.05). There was no significant increase in latency when measured 30 min after treatment. In the 25°C group, the latency increased 75.4% from 6.1±0.8 to 10.7±1.8 ms immediately following treatment. The increase in latency was maintained as long as 60 min after treatment although the increases were not statistically significant.
Amplitude
In the 32.5°C group, the CMAP amplitude showed no statistically significant change with treatment. In the 30°C group, the amplitude decreased immediately following and 30 min after treatment but these decreases were not statistically significant. The amplitude had returned to its pre-treatment value 60 min after treatment. In the 25°C group, the amplitude decreased significantly from 6.0±3.4 milivolts (mV) to 3.5±2.5 mV immediately following treatment. The decrease in latency maintained for at least 30 min. When measured 60 min after treatment, the amplitude did not return to its pre-treatment value although there was no statistical significance.
No response in CMAP
In the 32.5°C group, the CMAPs were evoked in all legs of the rabbits. In the 30°C group, the CMAP was not evoked in only one out of 14 cases (7.1%). In the 25°C group, in six out of 16 cases (37.5%) the CMAPs were not evoked.
Discussion
In spastic spinal cord injured rabbits, cold air therapy was effective when the intramuscular temperature was maintained less than 32.5°C. With an intramuscular temperature of 32.5°C, the effect of treatment lasted less than 30 min after treatment. With an intramuscular temperature of 30°C, the effect of treatment was maintained for 30–60 min. The complete block of nerve fiber conduction was produced more often with an intramuscular temperature of 25°C as compared to 30°C. There was 75.4% decrease in the CMAP amplitude and in 37.5%, complete conduction block (no CMAP evoked) was noted. The latency and amplitude of CMAP were delayed and reduced at 30 min after treatment in the 25°C group, which means that the recovery of conduction slowing was delayed in this group. Therefore in consideration of duration of treatment effect and the safety aspect of treatment, an intramuscular temperature of 30°C is optimal for the treatment of spasticity in spinalized rabbits.
Many studies on the effect of cold therapy in relieving spasticity have been reported.4,5,6,7,8,9,10 However, these studies used either a dipping or rubbing method in which case direct skin contact is necessary. Cold air therapy using an evaporative agent has also been used for the treatment of myofascial trigger point syndrome in combination with a stretching technique. Cold air therapy using an evaporative agent was not applicable to spasticity because the decrease in temperature was fairly high and it was impossible to apply longer than 10 min. On the other hand, the cold air therapy machine used in this study generates cold air without spraying an evaporative agent. With this machine it is possible to apply the cold for longer than 10 min.
In the 30°C group, the effect of cold air therapy was maintained for longer than 30 min after treatment when spasticity was measured by clinical parameters but there was no significant change when measured electrophysiologically. In spastic patients, the amplitude of H reflex is not decreased after conditioning stimuli such as vibration or tendon taps are delivered.15 This phenomenon is called loss of suppression of H reflex. In recently published research, the suppression of H reflex decreased as the paralyzed soleus muscle became more fatigable.16 In their study, acutely paralyzed group showed similar H reflex suppression as the able-bodied subjects. With follow up study in one acutely paralyzed individual, the subject showed similar H reflex suppression as the chronics after 44 weeks of paralysis. The fatigability in soleus muscle dropped substantially with increased time post injury. Therefore, the changes in muscle activation retrogradely influenced reflex excitability. The alteration that was caused by cold therapy in muscle may retrogradely influence the excitability in spinal cord to decrease spasticity. This could be suggested as one of the mechanisms of relieving spasticity by cold therapy.
Additionally, recent studies about the mechanism of spasticity mentioned about the contribution of changes in mechanical properties of muscles. In the swing phase of gait, the tibialis anterior shows abnormally high levels of activity, despite the lack of any EMG activity in its antagonist, the triceps surae muscle. This suggests that mechanical changes in the extensor apparatus of the ankle, rather than muscle activity in the triceps surae itself, lead to increased resistance to dorsiflexion movements.17 Direct measurement of the resistance of the relaxed ankle to slow displacement in the hemiparetic subjects has confirmed the importance of mechanical factors.18 Decreased spasticity manifested by clinical parameters but not by electrophysiological parameters as shown in this study supports the concept that changes in the mechanical properties of muscles could contribute to spasticity.
For the quantification of spasticity, most of the studies used clinical parameters and/or electrophysiologic parameters. Forssberg and Tedroff19 recommended the Ashworth scale as the best currently available clinical method for childhood spasticity rating and considered as reliable method when pre- and post rating is performed by the same examiner, which applied to this study. Although Ashworth scale has not been utilized in an animal model, other clinical parameters such as muscle stretch reflex, ankle clonus have been used as a measurement method for spasticity.20,21 Electrophysiologic parameters are objective but there is some controversy regarding the usefulness of these parameters in evaluating spasticity. Although both H/M ratio and F/M ratio have been reported to assess either the spinal segmental reflex or excitability of the anterior horn cells,22,23 there are studies reporting that they were increased in subjects with decreased muscle stretch reflex.24,25 Little et al26 reported that these ratios were useful methods in evaluating spasticity when measured serially. Therefore, the electrophysiologic parameters do not always correlate with the clinical aspect of spasticity.
There are several shortcomings in this study. First, the results of a study using animals can not be applied to humans. In this study, the differences in the thickness of subcutaneous tissue, size of lower leg, and difference in the effect of cold to nerve tissues must be considered. However, this study at least suggests the temperature effectively reducing spasticity in muscle that is one of many important neuromuscular components that induce spasticity. Secondly, the duration of cold application has not been determined. Further research, such as determining the changes of temperatures of skin and muscle in human, and determining the duration of cold application, are necessary.
Conclusion
Cold air therapy appears to be effective in relieving spasticity in spinal cord injured rabbits. When the intramuscular temperature was maintained at both 30 and 25.5°C, spasticity measured by clinical and electrophysiological parameters, decreased immediately following treatment and 30 min after treatment. Therefore, for the relief of spasticity, the intramuscular temperature must be maintained <30°C. However, maintaining the intramuscular temperature at 25°C for 30 min induces a complete conduction block of nerve fibers in 37.5% of the rabbits. Therefore, the safe intramuscular temperature for spasticity relief is 30°C. The decrease in spasticity was maintained 30 min after 30 min of cold air treatment and there was no significant changes in parameters when measured 60 min after treatment. The duration of treatment effect lasts between 30 and 60 min.
References
Delisa JA, Little J . Managing spasticity Am J Fam Med 1982 26: 117–122
Young JS et al. Spinal cord injury statistics Phoenix: Good Samaritan Medial Center 1985
Katz RT . Management of spasticity Am J Phys Med Rehabil 1988 67: 108–116
Bell KR, Lehmann JF . Effect of cooling on H- and T-reflexes in normal subjects Arch Phys Med Rehabil 1987 68: 490–493
Hartviksen K . Ice therapy in spasticity Acta Neurol Scand 1962 38: Suppl 3 79–84
Lehmann JF, deLateur BJ . Cryotherapy in Lehmann JF (ed) Therapeutic heat and cold 4th ed Baltimore: Williams & Wilkins 1990 pp 590–632
Levine MG et al. Relaxation of spasticity by physiological techniques Arch Phys Med Rehabil 1954 35: 214–223
Lightfoot E, Verrier M, Ashby P . Neurophysiological effects of prolonged cooling of the calf in patients with complete spinal transection Phys Ther 1975 55: 251–258
Mecomber SA, Herman RM . Effects of local hypothermia on reflex and voluntary activity Phys Ther 1971 1: 124–131
Price R et al. Influence of cryotherapy on spasticity at the human ankle Arch Phys Med Rehabil 1993 74: 300–304
Miglietta O . Action of cold on spasticity Am J Phys Med Rehabil 1973 52: 198–205
Knutsson E, Mattsson E . Effects of local cooling on monosynaptic reflexes in man Scand J Rehabil Med 1969 1: 126–132
Hardy JD . Physiology of temperature regulation Physiol Rev 1961 41: 521–606
Bohannon RW, Mellissa BS . Interater reliability of a modified Ashworth scale of muscle spasticity Phys Ther 1985 65: 46–47
DeGail P, Lance J, Nielson P . Different effects on tonic and phasic mechanisms produced by vibration of muscle in man J Neurol Neurosurg Psychiatry 1966 29: 1–11
Schindler-Ivens S, Shields RK . Low frequency depression of H-reflexes in humans with acute and chronic spinal-cord injury Exp Brain Res 2000 133: 233–241
Dietz V, Quintern J, Berger W . Electrophysiological studies of gait in spasticity and rigidity: evidence that altered mechanical properties of muscle contribute to hypertonia Brain 1981 104: 431–449
Thilmann AF, Fellows SJ, Ross HF . Biomechanical changes at the ankle joint after stroke J Neurol Neurosurg Psychiatry 1991 54: 134–139
Forssberg H, Tedroff KB . Botulinum toxin treatment in cerebral palsy: intervention with poor evaluation? Dev Med Child Neurol 1997 39: 635–640
Bennett DJ et al. Spasticity in rats with sacral spinal cord injury J Neurotrauma 1999 16: 69–84
Taylor JS, Friedman RF, Munson JB, Vierck CJ . Stretch hyperreflexia of triceps surae muscles in the conscious cat after dorsolateral spinal lesions J Neurosci 1997 17: 5004–5015
Angel RW, Hofmann WW . The H reflex in normal, spastic and rigid subjects Arch Neurol 1963 8: 591–596
Eisen A, Odusote K . Amplitude of the F wave: a potential means of documenting spasticity Neurol 1979 29: 1306–1309
Diamamtopoulos E, Zander OP . Excitability of motor neurones in spinal shock in man J Neurol Neurosurg Psychiatry 1967 30: 427–431
Weaver RA, Landau WM, Higgins JF . Fusimotor function: part II evidence of fusimotor depression in human spinal shock Arch Neurol 1963 9: 127–132
Little J, Halar E . H-reflex changes following spinal cord injury Arch Phys Med Rehabil 1985 66: 19–22
Acknowledgements
This study was supported by grant from Korea Research Foundation.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lee, SU., Bang, M. & Han, T. Effect of cold air therapy in relieving spasticity: applied to spinalized rabbits. Spinal Cord 40, 167–173 (2002). https://doi.org/10.1038/sj.sc.3101279
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101279