Abstract
Objectives: Evaluation of a FES (Functional Electrical Stimulation) device for the relief of postural hypertension and augmentation of cough in a C3 ventilator-dependent tetraplegic.
Study design: A single case study.
Setting: A supra regional spinal unit in the UK.
Method: A dual channel stimulator was designed that allowed selection and initiation of two predetermined stimulation intensities using a chin controlled joystick. Two sets of 70 mm diameter electrodes were placed either side of the abdomen. Approximately 80 mA, 300 μs, 40 Hz was required for assisted cough while about 40 mA was required for maintenance of blood pressure. After eating, the lower level stimulus is self-administered every 3 to 5 min gradually increasing the time between groups of burst to once every hour after 90 min.
Results: Following eating, a blood pressure of 60/45 mmHg was recorded. After five 1 s bursts of stimulation in quick repetition, this was increased to 133/92 mmHg. After 2 min blood pressure had fallen to 124/86 mmHg and to 93/66 after a further 4 min. The electrical stimulation was then repeated, returning the blood pressure to the previous higher level. Measurement of peak expiratory flow showed an increase from 275 l/min for an unassisted cough to 425 l/min when using the device.
Conclusion: The device is used every day. The user is now independent in coughing function and no longer requires suction or manual assistance. Maintenance of blood pressure has significantly improved his quality of life.
Similar content being viewed by others
Introduction
Tetraplegia at the C3/4 level results in severe compromise of respiratory muscles, both inspiratory and expiratory. The loss of inspiratory muscle function obviates the need for positive pressure ventilation most commonly in the UK via a tracheostomy. The lack of expiratory muscle function requires the use of tracheal suctioning and/or the use of assisted coughing to facilitate the clearance of pulmonary secretions to minimise pulmonary infection. Tracheal suction is an invasive technique that carries with it several well recognised complications even in a medically stable patient. Some of these are: repeated introduction of infection into the lungs,1 trauma to the airway mucosa,2 atelectasis and enforced apnoea in a ventilated patient. For these reasons it is desirable to keep this technique to a minimum or eliminate the need for it altogether.
Several authors have reported on the use of FES to assist respiratory function however these systems were all solely used with a respiratory application.3,4,5 This system is unique in that it has dual application for both the problems of postural hypotension and the inability to cough that are common in the high tetraplegic population.
Autonomic dysreflexia is a common complication of spinal cord injury above the spinal level of T6.6 It manifests as a sudden rise in blood pressure in response to a noxious stimulus below the level of the lesion and, if the stimulus is not removed, can lead to headache, cutis anserina (goose flesh), paresthesias, shivering, flushing and other symptoms. The rise in blood pressure is a consequence of reflex arterial spasm in response to the stimulation of the sympathetic nervous system. In the intact nervous system baroreceptors in the cerebral vessels, carotid sinuses and aorta detect the hypertension and stimulate a parasympathetic response, the principal consequence being vasodilatation and a fall in heart rate. However, in this group, the signals are blocked by the lesion, the resulting vasodilatation only occurring above the lesion. This is insufficient to return the blood pressure to normal levels. In a similar manner, lowering of blood pressure due to change of posture from lying to sitting can be poorly controlled resulting in postural or orthostatic hypotension.
Autonomic dysreflexia in response to electrical stimulation has been reported by several authors. Ashley et al7 reported rises in blood pressure in response to resistance training using electrical stimulation of the quadriceps muscles. The rise would occur immediately on starting the electrical stimulation but blood pressure returned to normal levels very quickly after stimulation had stopped. More recently, Sampson et al8 reported an investigation into the effect of electrical stimulation on blood pressure in C5–T4 SCI subjects with induced orthostatic hypotension. In this study, repeatable falls in blood pressure was induced using a tilt table. At two separate sessions, the quadriceps and pretibial muscles or the patellae and malleoli were stimulated using a 50 Hz, 250 μs wave form with currents up to 160 mA. Consistent rises in blood pressure were recorded, overcoming the fall due to induced orthostatic hypotension, whichever stimulation site was used, suggesting that the increase in the muscle pump action on venous return was not a significant factor in the effect. The rise in blood pressure increased with increasing stimulation amplitude but plateaued after 96 mA.
This study describes a single case study of the use of FES to increase the blood pressure of a C3 ventilator- dependent tetraplegic (male, 40 years of age) who was subject to chronic postural hypotension. This was moderately well controlled by the drug Midon (midodrine hydrochloride) but low blood pressure remained a problem, particularly after meal times. The subject had learned to control his own blood pressure by adjusting his posture by tilting the back and leg rests of his electric wheelchair, controlled by a chin joystick. The subject was unable to produce an effective voluntary cough and was dependent on manual assistance and tracheal suction to maintain his airways.
It was found that a rise in blood pressure could be induced by stimulation of the common peroneal nerve, quadriceps muscles or the abdominal muscles. By closing his epiglottis, the subject was able to prevent expiration and thus stack up to three breaths. When stimulation of the abdominal muscles was timed to occur just before the end of the third inhalation period, a cough of some force was produced.9
Method
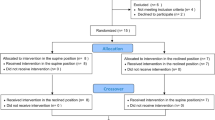
As the subject was very aware of the status of his blood pressure, it was decided to use a self-administrated system. Two pairs of electrodes were used to stimulate the upper and lower abdomen (Figure 1). An Odstock 2 Channel stimulator (O2CHS)10 was used. This device is a foot switch controlled stimulator intended for gait assistance in SCI, MS and stroke. In this application its foot switch input was controlled by a spare channel of the Possum Companion. When the joystick was pushed forward, the stimulator gave a 1 s burst of 300 μs, 40 Hz stimulation at amplitudes adjustable between 0 and 80 mA. With a little practice, the subject was able to synchronise the stimulation with epiglottis control and the ventilator's cycle.
The system was used in this form for some months but it soon became apparent that blood pressure was best controlled by fairly frequent but low level bursts of stimulation, lower than that required to produce a cough. The cough function was required less frequently and so the user required assistance to increase the levels of the device when he wanted to cough. It was therefore decided to design a system that allowed the user to select two pre-set levels of stimulation, by use of the chin joystick. The new system delivers a low level stimuli if the joystick is flicked for a short time but a larger output is selected if the joystick is pushed forward for 3 s and then released. An audio warning is given when the cough setting is selected.
Assessments
Blood pressure and heart rate were measured using an AND digital blood pressure monitor (UA-767). It was measured prior to electrical stimulation, immediately after stimulation and then at 2 min intervals until it returned to its previous level.
Peak expiratory flow was measured using a spirometer (Wright Peak Flow Mini Metre, Airmed.)
Results
The results reported here are from a single session. However they are representative of an effect observed repeatedly on several occasions.
Following eating a blood pressure of 60/45 mmHg with a heart rate of 81 beats per minute were recorded. After five 1 s bursts of stimulation at an amplitude of approximately 40 mA in quick repetition, the blood pressure increased to 133/92 mmHg together with an increase in heart rate to 92 beats per minute. After 2 min blood pressure had fallen to 124/86 mmHg and to 93/66 after a further 4 min. The heart rate was 91 and 85 beats per minute at the same periods. The electrical stimulation was then repeated, returning the blood pressure and heart rate to the previous levels.
Measurement of peak expiratory flow showed an increase from 275 l/min for an unassisted cough to 425 l/min when using the device. This in the normal range.
The system has been in daily use for 3 years. His carer puts on the device each morning when first in the chair and it is removed each evening before going to bed. Typically it is used for regulation of blood pressure after eating. Bursts of stimulation are self-administered every 3 to 5 min immediately after a meal and the period between bursts gradually increased over 90 min. At this point the device would typically be used hourly.
The user is now independent in coughing function and no longer requires suction or manual assistance.
Discussion
While the rise in blood pressure in response to the `noxious' electrical stimulus is consistent with autonomic dysreflexia, the accompanying rise in heart rate may appear at first to be contrary to the classic explanation of its mechanism. However, in a survey of 40 cases of autonomic dysreflexia only 10% had significant bradycardia while in 38 cases tachycardia was reported.11 It is possible that the spinal reflexes that cause vasoconstriction below the level of the lesions may also involve the excitatory sympathetic nerves that supply the heart. As these fibres originate from C3 to C8 spinal level the effect would be spinal lesion level dependent, increased heart rates occurring when the lesion was above T1.5
It is also possible that indirect effects may be occurring. Contraction of the abdominal muscles may increase bladder pressure which itself may induce the effect of autonomic dysreflexia. Increased intra-abdominal pressure may also increase pressure within the venae cavae resulting in greater filling of the right atrium of the heart. In accordance with the Frank-Starling law this will result in an increased stroke volume and therefore increased blood pressure. While these indirect effects may be contributory factors, as rises in blood pressure were seen in response to electrical stimulation of legs, it is likely that autonomic dysreflexia in direct response to the stimulation is the dominant factor.
This study describes a device designed to respond to the specific problems of one individual and it is not clear if it would have application in a wider group. Further work is required to obtain a better understanding of the mechanism of its action. That said, the device has been well accepted by its user and it would appear that by better maintenance of homeostasis, and by removal of the need for suction, it has contributed to an improved quality of life.
References
Sottile FD . Nosocomial pulmonary infection Crit Care Med 1986 14: 265–270
Kleiber C, Krutzfield N, Rose EF . Acute histologic changes in the tracheobronchial tree associated with different suction catheter insertion techniques Heart Lung 1988 17: 10–14
Zupan A et al. Effects of respiratory muscle training and electrical stimulation of abdominal muscles on respiratory capabilities in tetraplegic patients Spinal Cord 1997 35: 540–545
Linder SH . Functional electrical stimulation to enhance cough in quadriplegia Chest 1993 103: 166–169
Lin VWH, Singh H, Chitkara RK, Perkash I . Functional magnetic stimulation for restoring cough in patients with tetraplegia Arch Phys Med Rehabil 1998 79: 517–522
Karlsson AK . Autonomic dysreflexia, Scientific review Spinal Cord 1999 37: 383–391
Asley EA et al. Evidence of autonomic dysreflexia during functional electrical stimulation in individuals with spinal cord injuries Paraplegia 1993 31: 593–605
Sampson EE, Roberts MD, Burnham RS, Andrews BJ . Functional electrical stimulation effect on orthostatic hypotension after spinal cord injury Arch Phys Med Rehabil 2000 81: 139–143
Linder SH . Functional Electrical Stimulation to enhance cough in spinal cord injury Chest 1993 103: 166–169
Taylor PN et al.. Correction of Dropped Foot using the Odstock 2 Channel Stimulator (O2CHS). 4th annual IFESS conference 1999 257-260 ISBN 4-9980783-0-5
Kewalramani LS . Autonomic dysreflexia in tramuatic myelopathy Am J Phys Med 1980 59: 1–21
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Taylor, P., Tromans, A., Harris, K. et al. Electrical stimulation of abdominal muscles for control of blood pressure and augmentation of cough in a C3/4 level tetraplegic. Spinal Cord 40, 34–36 (2002). https://doi.org/10.1038/sj.sc.3101250
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101250
Keywords
This article is cited by
-
COVID-19 tsunami: the first case of a spinal cord injury patient in Italy
Spinal Cord Series and Cases (2020)
-
Electrical stimulation-evoked contractions blunt orthostatic hypotension in sub-acute spinal cord-injured individuals: two clinical case studies
Spinal Cord (2015)
-
Detection of the motor points of the abdominal muscles
European Journal of Applied Physiology (2014)
-
Electromyographic signal-activated functional electrical stimulation of abdominal muscles: the effect on pulmonary function in patients with tetraplegia
Spinal Cord (2007)