Abstract
Study design: A case report of purely epidural cavernous haemangioma with MRI appearance and pathological features.
Objective: To present a rare case of extradural mass with differential diagnosis.
Setting: Delhi, India.
Method: A 55-year-old man presented with progressive weakness and diminished sensation in both lower limbs. MRI demonstrated a pure extradural mass with no bony invasion. Histopathology of the lesion revealed a typical cavernous haemangioma.
Result: The patient showed significant improvement after surgery.
Conclusion: Radiological presentation could be confusing in a purely epidural cavernous haemangioma. Awareness of the characteristics of the lesion will facilitate diagnosis and treatment of the lesion.
Similar content being viewed by others
Introduction
Cavernous haemangiomata are not considered to be vascular neoplasms,1 but rather hamartomas or malformations of the microcirculation. They may affect any part of the neuraxis.2 Most of these lesions are encountered intracranially, supra tentorial sites being most commonly affected. Spinal cord cavernomas were thought to be rare lesions, but with the advent of MRI this lesion is more frequently diagnosed, and the frequency may be greater than previously thought.3,4,5
Cavernous haemangiomas presenting as a purely epidural lesion are very rare,6,7,8,9,10,11 with only 10 cases based on MR studies having been reported so far.12 In the current study the authors describe one case of epidural haemangioma, presenting as chronic progressive spinal cord compression, its MRI features and review of the literature.
Case Report
A 55-year-old man was admitted with a 2.5 year history of mid thoracic back pain and progressively decreasing sensation in both lower limbs. For the last 2 years he had noticed progressively increasing weakness of both lower limbs, and for the last 6 months he was bedridden. There was no other significant positive or negative history.
Examination
Neurological examination revealed grade 3–4 power in both lower limbs, bilaterally symmetrically brisk, deep tendon reflexes and bilaterally extensor planter responses. He had 50–80% sensory loss for all modalities below D9 level. No bowel or bladder involvement was noted.
Investigation
His routine investigations showed Hb: 10.5 g%, TLC: 7600/cmm, DLC: P 64%, L 30%, M 4%, E 2%, ESR 20 mm in first hour, bleeding time 2.30 min, clotting time 3.5 min, fasting blood sugar 78 mg%, liver function test: serum billirubin 0.8 mg%, SGOT 20 U/l, SGPT 28 U/l, Hbs Ag −ve, kidney function test: blood urea 23 mg%, serum creatinin 0.7 mg%, urine examination normal, HIV −ve, and ECG and X-ray chest were normal.
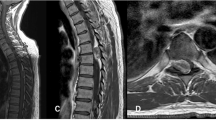
MRI showed a posteriorly situated extradural mass at D5–D7, pushing the cord anteriorly. It was isointense with the muscle and spinal cord on T1 weighted images but on T2 weighted images the lesion was of consistently high intensity, slightly less intense than cerebro-spinal fluid (CSF) (Figure 1a,b).
Preoperatively the first possibility considered was epidural tubercular granulation tissue (more common in this part of the world).
Operation notes
D5–D7 laminectomy was done and no bony erosion was noted. An extradural mass of 7×1.5 cm was seen on the posterior aspect. It did not have any lateral extension and there was no relation to any exiting nerve root. The pink coloured mass, soft to firm in consistency, was highly vascular but was easily separable from the dura. Using microsurgical technique, total excision of mass was achieved.
Histopathology
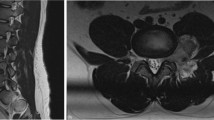
The lesion consisted of a large number of thin walled vascular channels in collagenous connective tissue (Figure 2), lined by a single layer of endothelial cells. Some of these were filled with blood. A diagnosis of cavernous haemangioma was made.
Postoperative course
The patient made a good recovery after surgery both in motor strength and sensations and was able to walk with support. At 5 months follow-up his muscle strength in the legs was MRC grade 4 to 5, the deep tendon reflexes of both lower limbs well within normal range with bilaterally flexor plantar responses, and a minimum sensory deficit of 10% to 20% for all modalities.
Discussion
Cavernous haemangiomas may develop anywhere in the neuraxis and its surrounding membranes.2 They represent approximately 5% to 12% of the vascular lesions of the spine.13 Epidural spinal cavernous haemangiomas are rare lesions, and commonly affect the vertebral bodies sometimes extending intraspinaly into the epidural space. So far only 56 cases have been reported in the literature.7,8,13,14,15,16,20
The most frequent clinical presentation of spinal cord cavernous haemangioma is a progressive compressive myelopathy, an acute onset is rare and is caused by an intramedullary haemorrhage. Turjman in his 11 cases of spinal cord haemangiomas, described only two acute presentations.21
The lesion or abnormality usually develops in the thoracic or lumbar regions.1 The most common site is the posterior part of the epidural space. The MR imaging of spinal cavernous haemangiomas are not as characteristic as those of cranial cavernomas. In most of the cases the T1 weighted images of spinal cavernous haemangioma shows a homogenous signal intensity similar to that of spinal cord and muscle, while on T2 weighted images the signal of the lesion is consistently high (as observed in the current case). Frequently the lesion is characterized by its extension, into the intervertebral foramen.9,10,22 The rim of hypointensity resulting from haemosidirin deposits, seen in intramedullary cavernous haemangioma is not seen in epidural cavernous haemangioma.22,23
These radiological characteristics help to distinguish cavernous haemangiomas from other lesions of the spine. In the present case due to its location (epidural) and MR characteristics (isointense on T1 and hyperintense on T2 weighted images) we considered the possibility of a tubercular granulation tissue. The other differential diagnoses for these types of lesion include neurinoma, meningioma, lymphoma and metastasis.24,25
The diagnosis is much easier when the lesion is associated with epidural haemorrhagic changes, but then other vascular informations can have similar MRI appearance. Conventional or MR angiography is useful and should be performed whenever there is doubt to differentiate these from other lesions.
References
Lee JP, Dah Jium Wang A, yau Yau Wai Yat-Sen H . Spinal extradural cavernous haemangioma Surg Neurol 1990 34: 345–351
Dobyns WB et al. Familial cavernous malformations of the central nervous systems and retina Ann Neurol 1987 21: 578–583
Cosgrove GR et al. Cavernous angiomas of the spinal cord J Neurosurg 1988 68: 31–36
Vaquero J, Martinez R, Martinez P . Cavernomas of the spinal cord: report of two cases Neurosurg 1988 22: 143–144
McCormick PC et al. Cavernous malformations of the spinal cord Neurosurgery 1988 23: 459–463
Harrington JF, Khan A, Grunnet M . Spinal epidural angioma presenting as a lumbar radiculopathy with analysis of magnetic resonance imaging characteristics; case report Neurosurgery 1995 36: 581–584
Enomoto H, Goto H . Spinal epidural cavernous angioma. MRI finding Neuroradiology 1991 33: 462
Feider HK, Yuille DL . An epidural cavernous haemangioma of the spine AJNR Am J Neuroradiol 1991 12: 243–244
Fukushima M et al. Dumbbell shaped spinal extradural haemangioma Arch Orthop Trauma Surg 1987 106: 394–396
Graziani N et al. Cavernous angiomas and arteriovenous malformations of the spinal epidural space; report of 11 cases Neurosurgery 1994 35: 856–864
Haimes AB, Krol G . Dumbbell-shaped spinal cavernous haemangioma a case report AJNR 1991 12: 1021–1022
Isla A et al. Spinal epidural haemangiomas J Neurosurg Sci 1993 37: 39–42
Padovani R et al. Extrathecal cavernous haemangioma Surg Neurol 1982 18: 463–465
Decker RE, San Augustin W, Epstein JA . Spinal epidural venous angioma causing foraminal enlargement and erosion of vertebral body J Neurosurg 1978 49: 605–606
Fields WS, Jones JR . Spinal epidural hemangioma in pregnancy Neurology 1957 7: 825–828
Padovani R et al. Spinal epidural haemangiomas Spine 1981 6: 336–340
Richardson RR, Cerullo LJ . Spinal epidural cavernous haemangioma Surg Neurol 1979 12: 266–268
Singh RVP et al. Spinal extradural cavernous angiomas Br J Neurosurg 1993 7: 79–82
Turner OA, Kernohan JW . Vascular malformations and vascular tumors involving the spinal cord. A pathologic study of 46 cases Arch Neurol Psychiatry 1949 46: 444–463
Vanderkelen B et al. Angiomas of the epidural space Acta Neurol Belg 1975 75: 99–106
Turjman E et al. MRI of intramedullary cavernous haemangiomas Neuroradiology 1995 37: 296–302
Fontaine S et al. Cavernous haemangiomas of the spinal cord: MR imaging Radiology 1988 166: 839–841
Rigamonti D et al. The MRI appearance of cavernous malformations (angiomas) J Neurosurg 1987 67: 518–524
Osborn AG . Diagnostic Neuroradiology St. Louis: Mosby 1994 pp 820–875
Osborn AG . Diagnostic Neuroradiology St. Louis: Mosby 1994 pp 876–918
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Goyal, A., Singh, A., Gupta, V. et al. Spinal epidural cavernous haemangioma: a case report and review of literature. Spinal Cord 40, 200–202 (2002). https://doi.org/10.1038/sj.sc.3101248
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101248
Keywords
This article is cited by
-
Clinical features and long-term surgical outcomes of pure spinal epidural cavernous hemangioma—report of 23 cases
Acta Neurochirurgica (2020)
-
Clinical and radiological presentation of spinal epidural haemangiomas: clinical series in a tertiary care centre during a 10-year period
European Spine Journal (2014)
-
Spinal epidural cavernous angiomas: a clinical series of four cases
Acta Neurochirurgica (2014)
-
Solitary spinal epidural cavernous angioma: report of nine surgically treated cases and review of the literature
European Spine Journal (2013)
-
Intralesional hemorrhage and thrombosis without rupture in a pure spinal epidural cavernous angioma: a rare cause of acute lumbal radiculopathy
European Spine Journal (2010)