Abstract
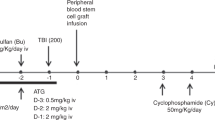
Reduced-intensity conditioning (RIC) regimens have been increasingly used as an alternative to conventional myeloablative conditioning (MAC) regimens for elderly patients, for patients medically infirm to qualify for conventional allogeneic stem cell transplantation (SCT), and for disorders in which traditional MAC-SCT are associated with high rates of non-relapse mortality. One of the theoretical advantages of RIC-SCT is that it might lend to better immune reconstitution after transplantation due to less damage of the thymus, allowing regeneration of naive T cells derived from prethymic donor stem cells, and due to the proliferation of immunologically competent host T cells that survive the conditioning regimen. Although limited, studies comparing immune recovery following RIC and MAC-SCT have been insightful. One of the main difficulties of these studies is the current spectrum of RIC protocols, which vary considerably in myeloablative and immunosuppressive potential, resulting in apparently contradictory findings. In spite of this, most reports have shown significant quantitative and/or qualitative differences in T- and B-cell reconstitution after RIC-SCT in comparison with conventional SCT. This paper will review current knowledge of immune reconstitution following RIC-SCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Bacigalupo A . Third EBMT/AMGEN Workshop on reduced-intensity conditioning allogenic haemopoietic stem cell transplants (RIC-HSCT), and panel consensus. Bone Marrow Transplant 2004; 33: 691–696.
Slavin S, Nagler A, Naparstek E, Kapelushni KY, Aker M, Cividalli G et al. Nonmyeloablative stem cell transplantation and cell therapy as an alternative to conventional bone marrow transplantation with lethal cytoreduction for the treatment of malignant and non-malignant hematological diseases. Blood 1998; 91: 756–763.
Giralt S, Thall PF, Khouri I, Wang X, Braunschweig I, Ippolitti C et al. Melphalan and purine analogs containing preparative regimens: reduced-intensity conditioning for patients with hematologic malignancies undergoing allogeneic progenitor cell transplantation. Blood 2001; 97: 631–637.
Nagler A, Aker M, Or R, Naparstek E, Varadi G, Brautbar C et al. Low-intensity conditioning is sufficient to ensure engraftment in matched unrelated bone marrow transplantation. Exp Hematol 2001; 29: 362–370.
Martino R, Caballero MD, Simon JAP, Canals C, Solano C, Urbano Ispizua A et al. Evidence for a graft-versus-leukemia effect after allogeneic peripheral blood stem cell transplantation with reduced-intensity conditioning in myelogenous leukemia and myelodisplastic syndromes. Blood 2002; 100: 2243–2245.
Khouri IF, Saliba RM, Giralt SA, Lee MS, Okoroji GJ, Hagemeister FB et al. Nonmyeloablative allogeneic hematopoietic transplantation as adoptive immunotherapy for indolent lymphoma: low incidence of toxicity, acute graft-vs-host disease, and treatment-related mortality. Blood 2001; 98: 3595–3599.
Storb R, Yu C, Wagner JL, Deeg J, Nash RA, Kiem HP et al. Stable mixed chimerism in DLA identical littermate dogs given sublethal total body irradiation before and pharmacological immunosuppression after marrow transplantation. Blood 1997; 89: 3048–3054.
McSweeney PA, Niederwieser D, Shizuru JA, Sandmaier B, Molina A, Maloney D et al. Hematopoietic cell transplantation in older patients with hematologic malignancies: replacing high-dose cytotoxic therapy with graft-vs-tumor effects. Blood 2001; 97: 3390–3400.
Delgado J, Thomson K, Russell N, Ewing J, Stewart W, Cook G et al. Results of alemtuzumab-based reduced-intensity allogeneic transplantation for chronic lymphocytic leukemia: a British Society of Blood and Marrow Transplantation Study. Blood 2006; 107: 1724–1730.
Shimoni A, Kroger N, Zabelina T, Ayuk F, Hardan I, Yeshurum M et al. Hematopoietic stem-cell transplantation from unrelated donors in elderly patients (age >55 years) with hematologic malignancies: older age is no longer a contraindication when using reduced intensity conditioning. Leukemia 2005; 19: 7–12.
Mohty M, Jacot W, Faucher C, Bay JO, Zandotti C, Collet L et al. Infectious complications following allogeneic HLA-identical sibling transplantation with antithymocyte globulin-based reduced intensity preparative regimen. Leukemia 2003; 17: 2168–2177.
Mackall C, Granger L, Sheard MA, Cepeda R, Gress RE . T-cell regeneration after bone marrow transplantation: differential CD45 isoform expression on thymic-derived versus thymic-depleted progeny. Blood 1993; 82: 2585–2594.
Haynes BF, Hale LP, Weinhod KJ, Patel DD, Liao HX, Bressler PB et al. Analysis of the adult thymus in reconstitution of T lymphocytes in HIV-infection. J Clin Invest 1999; 103: 453–469.
Picker L, Treer J, Ferguson-Darnell B, Collin PA, Buck D, Terstappen LWMM . Control of lymphocyte recirculation in man. J Immunol 1993; 150: 1105–1121.
Douek DC, McFarland RD, Keiser PH, Gage EA, Massey JM, Haynes BF et al. Changes in thymic function with age and during the treatment of HIV infection. Nature 1998; 396: 690–695.
Livak F, Schatz DG . T-cell receptor alpha locus V(D)J recombination by products are abundant in thymocytes and mature T-cells. Mol Cell Biol 1998; 6: 609–618.
De Villartay JP, Hockett RD, Coran D, Korsmeyer SJ, Cohen DI . Deletion of the human T-cell receptor δ-gene by a site specific recombination. Nature 1988; 335: 170–174.
Breit TM, Verschuren MCM, Wolvers-Tettero IL, Van Gastel-Mol EJ, Hahlen K, van Dongen JJ . Human T cell leukemias with continuos V(D)J recombinase activity for TCR-δ gene deletion. J Immunol 1997; 159: 4341–4349.
Douek DC, Vescio RA, Betts MR, Brechley JM, Hill BJ, Zhang L et al. Assessment of thymic output in adults after haematopoietic stem-cell transplantation and prediction of T-cell reconstitution. Lancet 2000; 355: 1875–1881.
Siu G, Kronenberg M, Strauss E, Hars R, Mark TW, Hood L . The structure, rearrangement and expression of D-Beta gene segments of the murine T cell antigen receptor. Nature 1984; 311: 344–350.
Gorski J, Yassai M, Zhu X, Kissella B, Keever C, Flomenberg N . Circulating T cell repertoire complexity in normal individuals and bone marrow recipients analyzed by CDR3 size spectratyping. J Immunol 1994; 152: 5109–5119.
Mackall CL, Gress RE . Thymic aging and T-cell regeneration. Immunol Rev 1997; 160: 91–102.
Mackall CL, Fry TJ, Bare C, Morgan P, Galbraith A, Gress RE . IL-7 increases both thymic-dependent and thymic-independent T-cell regeneration after bone marrow transplantation. Blood 2001; 97: 1491–1497.
Schulenburg A, Fischer M, Kalhs P, Mitterbauer M, Rabitsch W, Hildegard T et al. Immune recovery after conventional and non-myeloablative allogeneic stem cell transplantation. Leuk Lymph 2005; 46: 1755–1760.
Chao N, Liu CX, Rooney B, Chen BJ, Long GD, Vredenburg JJ et al. Nonmyeloablative regimen preserves ‘niches’ allowing for peripheral expansion of donor T-cells. Biol Blood Marrow Transplant 2002; 8: 249–256.
Jiménez M, Martínez C, Ercilla G, Carreras E, Urbano-Ispízua A, Aymerich M et al. Reduced intensity conditioning regimen preserves thymic function in the early period after hematopoietic stem cell transplantation. Exp Hematol 2005; 33: 1240–1248.
Maris M, Boeckh M, Storer B, Dawson M, White K, Keng M et al. Immunologic recovery after hematopoietic cell transplantation with nonmyeloablative conditioning. Exp Hematol 2003; 31: 941–952.
Petersen SL, Ryder LP, Björk P, Madsen HO, Heilmann C, Jacobsen N et al. A comparison of T-, B- and NK-cell reconstitution following conventional or nonmyeloablative conditioning and transplantation with bone marrow or peripheral blood stem cells from human leucocyte antigen identical sibling donors. Bone Marrow Transplant 2003; 32: 65–72.
Busca A, Lovisone E, Aliberti S, Locatelli F, Serra A, Scaravaglio P et al. Immune reconstitution and early infectious complications following nonmyeloablative hematopoietic stem cell transplantation. Hematology 2003; 8: 303–311.
Morecki S, Gelfand Y, Nagler A, Or R, Naparstek E, Varadi G et al. Immune reconstitution following allogeneic stem cell transplantation in recipients conditioned by low intensity vs myeloablative regimen. Bone Marrow Transplant 2001; 28: 243–249.
Friedman TM, Varadi G, Hopely DD, Filicko J, Wagner J, Ferber A et al. Nonmyeloablative conditioning allows for more rapid T-cell repertoire reconstitution following allogeneic matched unrelated bone marrow transplantation compared to myeloablative approaches. Biol Blood Marrow Transplant 2001; 7: 656–664.
Bahceci E, Epperson D, Douek DC, Melenhorst JJ, Childs R, Barret AJ . Early reconstitution of the T-cell repertoire after non-myeloablative peripheral blood stem cell transplantation is from post-thymic T-cell expansion and is unaffected by graft-versus-host disease or mixed chimaerism. Br J Haematol 2003; 122: 934–943.
Chakrabarti S, Avivi I, Mackinnon S, Ward K, Kottadiris PD, Osman H et al. Respiratory virus infections in transplant recipients after reduced-intensity conditioning with Campath-1H: high incidence but low mortality. Br J Haematol 2002; 119: 1125–1132.
D'Sa S, Peggs K, Pizzey A, Verfuerth S, Thuraisundaram S, Watts M et al. T- and B-cell immune reconstitution and clinical outcome in patients with multiple myeloma receiving T-cell-depleted, reduced-intensity allogeneic stem cell transplantation with an alemtuzumab-containing conditioning regimen followed by escalated donor lymphocyte infusions. Br J Haematol 2003; 123: 309–322.
Dodero A, Carrabba M, Milani R, Rizzo E, Raganato A, Montefusco V et al. Reduced-intensity conditioning containing low-dose alemtuzumab before allogeneic peripheral blood stem cell transplantation: graft-versus-host disease is decreased but T-cell reconstitution is delayed. Exp Hematol 2005; 33: 920–927.
Markert ML, Boeck A, Hale LP, Kloster AL, McLaughlin TM, Batchvarova MN et al. Transplantation of thymus tissue in complete DiGeorge syndrome. N Engl J Med 1999; 341: 1180–1189.
Chung B, Burnham B, Barsky L, Weinberg K . Radiosensitivity of thymic interleukin-7 production and thymopopiesis after bone marrow transplantation. Blood 2001; 98: 1601–1606.
Nikolic B, Khan A, Sykes M . Induction of tolerance by mixed chimerism with nonmyeloablative host conditioning: the importance of overcoming intrathymic alloresistance. Biol Blood Marrow Transplant 2001; 7: 144–153.
Mapara MY, Pelot M, Zhao G, Swenson K, Pearson D, Sykes M . Induction of stable long-term mixed hematopoietic chimerism following nonmyeloablative conditioning with T cell-depleting antibodies, cyclophosphamide, and thymic irradiation leads to donor-specific in vitro and in vivo tolerance. Biol Blood Marrow Transplant 2001; 7: 646–655.
Sykes M, Preffer F, McAfee S, Saidman SL, Weymouth D, Andrews DM et al. Mixed lymphohematopoietic chimerism is achievable following non-myeloablative therapy and HLA-mismatched donor marrow transplantation. Lancet 1998; 353: 1755–1759.
Spitzer TR, McAfee S, Sackstein R, Colby C, Toh HC, Multani P et al. Intentional induction of mixed chimerism and achievement of anti-tumor responses following non-myeloablative conditioning therapy and HLA-matched donor bone marrow transplantation for refractory hematologic malignances. Biol Blood Marrow Transplant 2000; 6: 309–320.
Bancherau J, Steinman RM . Dendritic cells and the control of immunity. Nature 1998; 392: 245–255.
Hart DNJ . Dendritic cells: unique leukocyte populations which control the primary immune response. Blood 1997; 90: 3245–3287.
Mac Donald KPA, Munster DJ, Clark GJ, Dzionek A, Schmitz J, Hart DNJ . Characterization of human blood dendritic cell subsets. Blood 2002; 100: 4512–4520.
De Jong EC, Smits HH, Kapsenberg ML . Dendritic cell-mediated T cell polarization. Springer Semin Immunol 2005; 26: 289–307.
Auffermann-Gretzinger S, Lossos IS, Vayntrub TA, Leong W, Grumet FC, Blume KG et al. Rapid establishment of dendritic cell chimerism in allogeneic hematopoietic cell transplant recipients. Blood 2002; 99: 1442–1448.
Mohty M, Gaugler B, Faucher C, Sainty D, Lafage-Pochitaloff M, Vey N et al. Recovery of lymphocyte and dendritic cell subsets following reduced intensity allogeneic bone marrow transplantation. Hematology 2002; 7: 157–164.
Della Porta M, Rigolin GM, Alessandrino EP, Maiocchi M, Malcovati L, Vanelli L et al. Dendritic cell recovery after allogeneic stem-cell transplantation in acute leukemia: correlations with clinical and transplant characteristics. Br J Haematol 2004; 72: 18–25.
Chklovskaia E, Nowbakht P, Nissen C, Gratwohl A, Bargetzi M, Wodnar-Filipowicz A . Reconstitution of dendritic cells and natural killer-cell subsets after allogeneic stem cell transplantation: effects of endogenous flt ligand. Blood 2004; 103: 3860–3868.
Morse MA, Rizzieri D, Stenzel TT, Hobeika AC, Vredenburgh JJ, Chao NJ et al. Dendritic cell recovery following nonmyeloablative allogeneic stem cell transplants. J Hematother Stem Cell Res 2002; 11: 659–668.
Sanchez-Guijo FM, Sanchez-Abarca LI, Bueno C, Villaron E, Lopez-Holgado N, Vazquez L et al. Long-term immune recovery of patients undergoing allogeneic stem cell transplantation: a comparison with their respective sibling donors. Biol Blood Marrow Transplant 2005; 11: 354–361.
Boeck S, Hamann M, Pihusch V, Heller T, Diem H, Rolf B et al. Kinetics of Dendritic cell chimerism and T cell chimerism in allogeneic hematopoietic stem cell recipients. Bone Marrow Transplant 2006; 37: 57–64.
Mohty M, Blaise D, Faucher C, Bardou VJ, Gastaut JA, Viens P et al. Impact of plasmocytoid dendritic cells on outcome after reduced-intensity conditioning allogeneic stem cell transplantation. Leukemia 2005; 19: 1–6.
Reddy V, Iturraspe JA, Tzolas AC, Maier-Kriesche HU, Schold J, Wingard JR . Low dendritic cell count after allogeneic hematopoietic stem cell transplantation predicts relapse, death, and acute graft-versus-host disease. Blood 2004; 103: 4330–4335.
Chan GW, Gorgun G, Miller KB, Foss FM . Persistence of host dendritic cells after transplantation is associated with graft-versus-host disease. Biol Blood Marrow Transplant 2003; 9: 170–176.
Nachbaur D, Kircher B, Eisendle K, Latzer K, Haun M, Gastl G . Phenotype, function and chimaerism of monocyte-derived blood dendritic cells after allogeneic haemopoietic stem cell transplantation. Br J Haematol 2003; 123: 119–126.
Weinberg K, Blazar BR, Wagner JE, Agura E, Hill BJ, Smogorzewska M et al. Factors affecting thymic function after allogeneic hematopoietic stem cell transplantation. Blood 2001; 97: 1458–1466.
Storek J, Gooley T, Witherspoon RP, Sullivan KM, Storb R . Infectious morbidity in long-term survivors of allogeneic marrow transplantation is associated with low CD4T cell counts. Am Hematol 1997; 54: 131–138.
Maury S, Mary JI, Rabian C, Schwarzinger M, Toubert A, Scieux C et al. Prolonged immune deficiency following allogeneic stem cell transplantation: risk factors and complications in adult patients. Br J Haematol 2001; 115: 630–641.
Fallen PR, McGreavy L, Madrigal JA, Potter M, Ethell M, Prentince HG et al. Factors affecting reconstitution of the T cell compartment in allogeneic haematopoietic cell transplant recipients. Bone Marrow Transplant 2003; 32: 1001–1014.
Lewin S, Heller G, Zhang L, Rodrigues E, Skulsky E, van den Brink MR et al. Direct evidence for new T-cell generation by patients after either T-cell-depleted or unmodified allogeneic hematopoietic stem cell transplantation. Blood 2002; 100: 2235–2242.
Poulin JF, Sylvestre M, Champagne P, Dion ML, Kettaf N, Dumont A et al. Evidence for adequate thymic function but impaired naive T-cell survival following allogeneic hematopoietic stem cell transplantation in the absence of chronic graft-versus-host disease. Blood 2003; 102: 4600–4607.
Seemayer TA, Lapp WS, Bolande RP . Thymic involution in murine graft versus host reaction: epithelial injury mimicking human thymic dysplasia. Am J Pathol 1977; 88: 119–133.
Seddik M, Seemayer TA, Lapp VS . T cell functional defect associated with thymic epithelial cell injury induced by a graft-versus-host reaction. Transplantation 1980; 29: 61–66.
Fukushi N, Arase H, Wang B, Ogasawara K, Gotohda T, Onoe K . Thymus: a direct target tissue in graft-versus-host reaction after allogeneic bone marrow transplantation that results in abrogation of induction of self-tolerance. Proc Natl Acad Aci USA 1990; 87: 6301–6305.
Hollander GA, Widmer B, Burakoff SJ . Loss of normal thymic repertoire selection and persistence of autoreactive T cells in graft vs host disease. J Immunol 1994; 152: 1609–1617.
van den Brink MR, Moore E, Ferrara JL, Bukaroff SJ . Graft-versus-host-disease-associated thymic damage results in the appearance of T cell clones with anti-host reactivity. Transplantation 2000; 69: 446–449.
Hazenberg MD, Otto S, de Pauw ES, Roelofs H, Fibbe WE, Hamann D et al. T-cell excision circle and T-cell dynamics after allogeneic stem cell transplantation are related to clinical events. Blood 2002; 99: 3449–3453.
Mielcarek M, Martin PJ, Leisenring W, Flowers M, Maloney D, Sandmaier B et al. Graft-versus-host disease after non-myeloablative versus conventional hematopoietic stem cell transplantation. Blood 2003; 102: 756–762.
Couriel DR, Saliba RM, Giralt S, Khouri I, Andersson B, de Lima M et al. Acute and chronic graft-versus-host disease after ablative and non-myeloablative conditioning for allogeneic hematopoietic transplantation. Biol Blood Marrow Transplant 2004; 10: 178–185.
Saito T, Kanda Y, Nakai K, Kim S-W, Arima F, Kami M et al. Immune reconstitution following reduced-intensity transplantation with cladribine, busulfan, and antithymocyte globulin: serial comparison with conventional myeloablative transplantation. Bone Marrow Transplant 2003; 32: 601–608.
Jamieson BD, Douek DC, Killian S, Hultin LE, Scripture-Adams DD, Giorgi JV et al. Generation of functional thymocytes in the human adult. Immunity 1999; 10: 569–575.
Poulin JF, Viswanathan MN, Harris JM, Komanduri KV, Wieder E, Ringuette N et al. Direct evidence for thymic function in adult humans. J Exp Med 1999; 190: 479–486.
Steinmann GG . Changes in the human thymus during aging. Curr Topics Pathol 1986; 75: 43–88.
Mackall CL, Fleicher TA, Brown MR, Andrich MP, Chen CC, Feuerstein IM et al. Age, thymopoiesis, and CD4+ T-lymphocyte regeneration after intensive chemotherapy. New Engl J Med 1995; 332: 143–149.
Weinberg K, Annett G, Kashyap A, Lenarsky C, Forman SJ, Parkman R . The effect of thymic function on immunocompetence following bone marrow transplant. Biol Blood Marrow Transplant 1995; 1: 18–23.
Storek J, Joseph A, Dawson MA, Douek DC, Storer B, Maloney DG . Factors influencing T-lymphopoiesis after allogeneic hematopoietic cell transplantation. Transplantation 2002; 73: 1154–1158.
Steeffens CM, Al-Harthi L, Shott S, Yogev R, Landay A . Evaluation of thymopoiesis using T cell receptor excision circles (TRECs): differential correlation between adult and pediatric TRECs and naïve phenotypes. Clin Immunol 2000; 97: 95–101.
Eyrich M, Wollny G, Tzaribaschev N, Dietz K, Brugger D, Bader P et al. Onset of thymic recovery and plateau of thymic output are differentially regulated after stem cell transplantation in children. Biol Blood Marrow Transplant 2005; 11: 194–205.
Jimenez M, Martinez C, Ercilla G, Carreras E, Urbano-Ispizua A, Aymerich M et al. Clinical factors influencing T-cell receptor excision circle (TRECs) counts following allogeneic stem cell transplantation in adults. Transplant Immunol 2006; 16: 52–59.
Savage WJ, Bleesing JJ, Douek D, Brown MR, Linton GM, Malech HL et al. Lymphocyte reconstitution following non-myeloablative hematopoietic stem cell transplantation follows two patterns depending on age and donor/recipient chimerism. Bone Marrow Transplant 2001; 28: 463–471.
Hogan WJ, Little MT, Zellmer E, friedetzky A, Diaconescu R, Gisburne S et al. Postgrafting immunosuppression with sirolimus and cyclosporine facilitates stable mixed hematopoietic chimerism in dogs given sublethal total body irradiation before marrow transplantation from DLA-identical littermates. Biol Blood Marrow Transplant 2003; 9: 489–495.
Kahl C, Mielcarek M, Iwata M, Harkey MA, Storer B, Torok-Storb B . Radiation dose determines the degree of myeloid engraftment following nonmyeloablative stem cell transplantation. Biol Blood Marrow Transplant 2004; 10: 826–833.
Panse JP, Heimfeld S, Guthrie KA, Maris MB, Maloney DG, Baril BB et al. Allogeneic peripheral blood stem cell graft composition affects early T-cell chimerism and later clinical outcomes after nonmyeloablative conditioning. Br J Haematol 2005; 128: 659–667.
Santos GW, Sensenbrenner LL, Burke PJ, Colvin M, Owens Jr AH, Bias WB et al. Marrow transplantation in man following cyclophosphamide. Transplant Proc 1971; 3: 400–404.
Hill RS, Petersen FB, Storb R, Appelbaum FR, Doney K, Dahlberg S et al. Mixed hematologic chimerism after allogeneic marrow transplantation for severe aplastic anemia is associated with a higher risk of graft rejection and a lessened incidence of acute graft-versus-host disease. Blood 1986; 67: 811–816.
Bretagne S, Vidaud M, Kuentz M, Cordonier C, Henni T, Vinci G et al. Mixed blood chimerism in T cell-depleted bone marrow transplantation with CD6-depleted allogeneic marrow: a stable equilibrium. Blood 1990; 75: 296–304.
Nakai K, Mineishi S, Kami M, Saito T, Hori A, Kojima R et al. Antithymocyte globuline affects the occurrence of acute and chronic graft-versus-host disease after a reduced-intensity conditioning regimen by modulating mixed chimerism induction and immune reconstitution. Transplantation 2003; 75: 2135–2143.
Maris MB, Sandmaier BM, Storer BE, Maloney DG, Shizuru JA, Agura E et al. Unrelated donor granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear cell transplantation after nonmyeloablative conditioning: the effect of postgrafting mycophenolate mofetil dosing. Biol Blood Marrow Transplant 2006; 12: 454–465.
Giaccone L, McCune JS, Maris MB, Gooley TA, Sandmaier BM, Slattery JT et al. Pharmacodinamics of mycophenolate mofetil after nonmyeloabaltive conditioning and unrelated donor hematopoietic cell transplantation. Blood 2005; 106: 4381–4388.
Wu CJ, Chillemi A, Alyea EP, Orsini E, Neuberg D, Soiffer RJ et al. Reconstitution of T-cell receptor repertoire diversity following T-cell depleted allogeneic bone marrow transplantation is related to hematopoietic chimerism. Blood 2000; 95: 352–359.
Mattsson J, Uzunel M, Remberger M, Ringden O . T cell mixed chimerism is significantly correlated to a decreased risk of acute graft-versus-host disease after allogeneic stem cell transplantation. Transplantation 2001; 71: 433–439.
Keil F, Prinz E, Moser K, Mannhalter C, Kalhs P, Worel N et al. Rapid establishment of long-term culture-initiating cells of donor origin after nonmyeloablative allogeneic hematopoietic stem-cell transplantation, and significant prognostic impact of donor T-cell chimerism on stable engraftment and progression-free survival. Transplantation 2003; 76: 230–236.
Baron F, Maris MB, Sandmaier BM, Storer BE, Sorror M, Diaconescu R et al. Graft-versus-tumor effects after allogeneic hematopoietic cell transplantation with nonmyeloablative conditioning. J Clin Oncol 2005; 23: 1993–2003.
Perez-Simon JA, Caballero D, Diez-Campelo M, Lopez-Perez R, Mateos G, Canizo C et al. Chimerism and minimal residual disease monitoring after reduced intensity conditioning (RIC) allogeneic transplantation. Leukemia 2002; 16: 1423–1431.
Dey BR, McAfee S, Colby C, Sackstein R, Saidman s, Tarbell N et al. Impact of prophylactic donor leukocyte infusions on mixed chimerism, graft-versus-host disease, and antitumor response in patients with advanced hematologic malignances treated with nonmyeloablative conditioning and allogeneic bone marrow transplantation. Biol Blood Marrow Transplant 2003; 9: 320–329.
Peggs KS, Thomson K, Hart H, Geary J, Morris EC, Yong K et al. Dose-escalated donor lymphocyte infusions following reduced intensity transplantation: toxicity, chimerism and diseases responses. Blood 2004; 103: 1548–1556.
Acknowledgements
This work was supported in part by grants from Institut d'Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Red Temática del Cáncer Instituto de Salud Carlos III n° CO3/10, FIS PI020622 and PI02/0350 from the Fondo de Investigaciones Sanitarias de la Seguridad Social, Spanish Ministry of Health, and SGR2001 00375 from Generalitat de Catalunya.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jiménez, M., Ercilla, G. & Martínez, C. Immune reconstitution after allogeneic stem cell transplantation with reduced-intensity conditioning regimens. Leukemia 21, 1628–1637 (2007). https://doi.org/10.1038/sj.leu.2404681
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2404681
Keywords
This article is cited by
-
Autoimmune cytopenias (AIC) following allogeneic haematopoietic stem cell transplant for acquired aplastic anaemia: a joint study of the Autoimmune Diseases and Severe Aplastic Anaemia Working Parties (ADWP/SAAWP) of the European Society for Blood and Marrow Transplantation (EBMT)
Bone Marrow Transplantation (2020)
-
Assessment of TREC, KREC and telomere length in long-term survivors after allogeneic HSCT: the role of GvHD and graft source and evidence for telomere homeostasis in young recipients
Bone Marrow Transplantation (2018)
-
Non-myeloablative conditioning for lower-risk myelodysplastic syndrome with bone marrow blasts less than 5 %—a feasibility study
Annals of Hematology (2016)
-
Myc and AP-1 expression in T cells and T-cell activation in patients after hematopoietic stem cell transplantation
Clinical and Experimental Medicine (2015)
-
Impact of lymphocyte and monocyte recovery on the outcomes of allogeneic hematopoietic SCT with fludarabine and melphalan conditioning
Bone Marrow Transplantation (2013)