Abstract
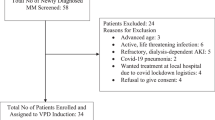
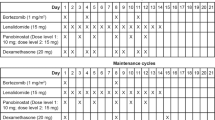
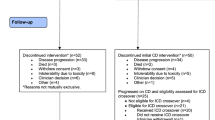
The aim of this study was the evaluation of the effect of intermediate doses of thalidomide with dexamethasone (Thal/Dex) on disease course and bone disease in patients with refractory/relapsed myeloma who were under zoledronic acid therapy. We studied 35 patients, who received thalidomide at a dose of 200 mg/daily. We measured, pre-, 3 and 6 months post-treatment soluble receptor activator of nuclear factor-κB ligand (sRANKL), osteoprotegerin (OPG), osteopontin (OPN), markers of bone resorption and formation. Before treatment, patients had increased levels of sRANKL/OPG ratio, bone resorption markers and OPN, while they had suppressed bone formation. The pretreatment sRANKL/OPG ratio correlated with the extent of bone disease. Thal/Dex administration resulted in a significant reduction of sRANKL/OPG ratio, and bone resorption. Bone formation, OPG and OPN did not show any alteration. Changes of sRANKL/OPG ratio correlated with changes of bone resorption markers. Thal/Dex was given for a median time of 10 months and the median follow-up period was 22 months. The response rate was 65.7%. The median survival was 19.5 months. β2-microglobulin, type of response and International Staging System predicted for survival. These results suggest that the combination of intermediate dose of Thal/Dex is effective in patients with refractory/relapsed myeloma and improves abnormal bone remodeling through the reduction of sRANKL/OPG ratio.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Terpos E, Rahemtulla A, Dimopoulos MA . Current treatment options for myeloma. Expert Opin Pharmacother 2005; 6: 1127–1142.
Terpos E, Apperley JF, Samson D, Giles C, Crawley C, Kanfer E et al. Autologous stem cell transplantation in multiple myeloma: improved survival in nonsecretory multiple myeloma but lack of influence of age, status at transplant, previous treatment and conditioning regimen. A single-centre experience in 127 patients. Bone Marrow Transplant 2003; 31: 163–170.
Singhal S, Mehta J, Desikan R, Ayers D, Roberson P, Eddlemon P et al. Anti tumor activity of thalidomide in refractory multiple myeloma. N Engl J Med 1999; 341: 1566–1571.
Rajkumar SV, Leonard JP, Pekle K, Lyons L, Michaeli J . Thalidomide for previously untreated indolent or smoldering multiple myeloma. Leukemia 2001; 15: 1274–1276.
Dimopoulos MA, Anagnostopoulos A, Weber D . Treatment of plasma cell dyscrasias with thalidomide and its derivatives. J Clin Oncol 2003; 21: 4444–4454.
Barlogie B, Desikan R, Eddlemon P, Spencer T, Zeldis J, Munshi N et al. Extended survival in advanced and refractory multiple myeloma after single-agent thalidomide: identification of prognostic factors in a phase 2 study of 169 patients. Blood 2001; 98: 492–494.
Wechalekar AD, Chen CI, Sutton D, Reece D, Voralia M, Stewart AK . Intermediate dose thalidomide (200 mg daily) has comparable efficacy and less toxicity than higher doses in relapsed multiple myeloma. Leukemia Lymphoma 2003; 44: 1147–1149.
Dimopoulos MA, Zervas K, Kouvatseas G, Galani E, Grigoraki V, Kiamouris C et al. Thalidomide and dexamethasone combination for refractory multiple myeloma. Ann Oncol 2001; 12: 991–995.
Anagnostopoulos A, Weber D, Rankin K, Delasalle K, Alexanian R . Thalidomide and dexamethasone for resistant multiple myeloma. Br J Haematol 2003; 121: 768–771.
Kuehl WM, Bergsagel PL . Multiple myeloma: evolving genetic events and host interactions. Nat Rev Cancer 2002; 2: 175–187.
Terpos E, Politou M, Rahemtulla A . New insights into the pathophysiology and management of bone disease in multiple myeloma. Br J Haematol 2003; 123: 758–769.
Standal T, Hjorth-Hansen H, Rasmussen T, Dahl IM, Lenhoff S, Brenne AT et al. Osteopontin is an adhesive factor for myeloma cells and is found in increased levels in plasma from patients with multiple myeloma. Haematologica 2004; 89: 174–182.
Sezer O, Heider U, Zavrski I, Kuhne CA, Hofbauer LC . RANK ligand and osteoprotegerin in myeloma bone disease. Blood 2003; 101: 2094–2098.
Vanderkerken K, De Leenheer E, Shipman C, Asosingh K, Willems A, Van Camp B et al. Recombinant osteoprotegerin decreases tumor burden and increases survival in a murine model of multiple myeloma. Cancer Res 2003; 63: 287–289.
Terpos E, Szydlo R, Apperley JF, Hatjiharissi E, Politou M, Meletis J et al. Soluble receptor activator of nuclear factor kappa-B ligand-osteoprotegerin ratio predicts survival in multiple myeloma: proposal for a novel prognostic index. Blood 2003; 102: 1064–1069.
Grimaud E, Soubigou L, Couillaud S, Coipeau P, Moreau A, Passuti N et al. Receptor activator of nuclear factor kappaB ligand (RANKL)/osteoprotegerin (OPG) ratio is increased in severe osteolysis. Am J Pathol 2003; 163: 2021–2031.
Heider U, Langelotz C, Jakob C, Zavrski I, Fleissner C, Eucker J et al. Expression of receptor activator of nuclear factor kappaB ligand on bone marrow plasma cells correlates with osteolytic bone disease in patients with multiple myeloma. Clin Cancer Res 2003; 9: 1436–1440.
Greipp PR, San Miguel J, Durie BG, Crowley JJ, Barlogie B, Blade J et al. International Staging System for multiple myeloma. J Clin Oncol 2005; 23: 3412–3420.
Blade J, Samson D, Reece D, Apperley J, Bjorkstrand B, Gahrton G et al. Criteria for evaluating disease response and progression in patients with multiple myeloma treated by high-dose therapy and haemopoietic stem cell transplantation. Myeloma Subcommittee of the EBMT. Br J Haematol 1998; 102: 1115–1123.
Kazama JJ, Shigematsu T, Yano K, Tsuda E, Miura M, Iwasaki Y et al. Increased circulating levels of osteoclastogenesis inhibitory factor (osteoprotegerin) in patients with chronic renal failure. Am J Kidney Dis 2002; 39: 525–532.
Dimopoulos MA, Anagnostopoulos A . Thalidomide in relapsed/refractory multiple myeloma: pivotal trials conducted outside the United States. Semin Hematol 2003; 40: 8–16.
Palumbo A, Bertola A, Falco P, Rosato R, Cavallo F, Giaccone L et al. Efficacy of low-dose thalidomide and dexamethasone as first salvage regimen in multiple myeloma. Hematol J 2004; 5: 318–324.
Rajkumar SV, Hayman S, Gertz MA, Dispenzieri A, Lacy MQ, Greipp PR et al. Combination therapy with thalidomide plus dexamethasone for newly diagnosed myeloma. J Clin Oncol 2002; 20: 4319–4323.
Cavenagh JD, Oakervee H . Thalidomide in multiple myeloma: current status and future prospects. Br J Haematol 2003; 120: 18–26.
Bennett CL, Schumock GT, Desai AA, Kwaan HC, Raisch DW, Newlin R et al. Thalidomide-associated deep vein thrombosis and pulmonary embolism. Am J Med 2002; 113: 603–606.
Zangari M, Barlogie B, Anaissie E, Saghafifar F, Eddlemon P, Jacobson J et al. Deep vein thrombosis in patients with multiple myeloma treated with thalidomide and chemotherapy: effects of prophylactic and therapeutic anticoagulation. Br J Haematol 2004; 126: 715–721.
Scarpace S, Hahn T, Roy H, Brown K, Paplham P, Chanan-Khan A et al. Arterial thrombosis in four patients treated with thalidomide. Leuk Lymphoma 2005; 46: 239–242.
Fahdi IE, Gaddam V, Saucedo JF, Kishan CV, Vyas K, Deneke MG et al. Bradycardia during therapy for multiple myeloma with thalidomide. Am J Cardiol 2004; 93: 1052–1055.
Pearse RN, Sordillo EM, Yaccoby S, Wong BR, Liau DF, Colman N et al. Multiple myeloma disrupts the TRANCE/osteoprotegerin cytokine axis to trigger bone destruction and promote tumor progression. Proc Natl Acad Sci USA 2001; 98: 11581–11586.
Terpos E, Politou M, Szydlo R, Nadal E, Avery S, Olavarria E et al. Autologous stem cell transplantation normalizes abnormal bone remodeling and sRANKL/osteoprotegerin ratio in patients with multiple myeloma. Leukemia 2004; 18: 1420–1426.
Terpos E, de la Fuente J, Szydlo R, Hatjiharissi E, Viniou N, Meletis J et al. Tartrate-resistant acid phosphatase isoform 5b: a novel serum marker for monitoring bone disease in multiple myeloma. Int J Cancer 2003; 106: 455–457.
Jung K, Lein M, Stephan C, Von Hosslin K, Semjonow A, Sinha P et al. Comparison of 10 serum bone turnover markers in prostate carcinoma patients with bone metastatic spread: diagnostic and prognostic implications. Int J Cancer 2004; 111: 783–791.
Saeki Y, Mima T, Ishii T, Ogata A, Kobayashi H, Ohshima S et al. Enhanced production of osteopontin in multiple myeloma: clinical and pathogenic implications. Br J Haematol 2003; 123: 263–270.
Silvestris F, Cafforio P, Tucci M, Grinello D, Dammacco F . Upregulation of osteoblast apoptosis by malignant plasma cells: a role in myeloma bone disease. Br J Haematol 2003; 122: 39–52.
Tian E, Zhan F, Walker R, Rasmussen E, Ma Y, Barlogie B et al. The role of the Wnt-signaling antagonist DKK1 in the development of osteolytic lesions in multiple myeloma. N Engl J Med 2003; 349: 2483–2494.
Seidel C, Hjertner O, Abildgaard N, Heickendorff L, Hjorth M, Westin J et al. Serum osteoprotegerin levels are reduced in patients with multiple myeloma with lytic bone disease. Blood 2001; 98: 2269–2271.
Lipton A, Ali SM, Leitzel K, Chinchilli V, Witters L, Engle L et al. Serum osteoprotegerin levels in healthy controls and cancer patients. Clin Cancer Res 2002; 8: 2306–2310.
Viereck V, Emons G, Lauck V, Frosch KH, Blaschke S, Grundker C et al. Bisphosphonates pamidronate and zoledronic acid stimulate osteoprotegerin production by primary human osteoblasts. Biochem Biophys Res Commun 2002; 291: 680–686.
Pan B, Farrugia AN, To LB, Findlay DM, Green J, Lynch K et al. The nitrogen-containing bisphosphonate, zoledronic acid, influences RANKL expression in human osteoblast-like cells by activating TNF-alpha converting enzyme (TACE). J Bone Miner Res 2004; 19: 147–154.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terpos, E., Mihou, D., Szydlo, R. et al. The combination of intermediate doses of thalidomide with dexamethasone is an effective treatment for patients with refractory/relapsed multiple myeloma and normalizes abnormal bone remodeling, through the reduction of sRANKL/osteoprotegerin ratio. Leukemia 19, 1969–1976 (2005). https://doi.org/10.1038/sj.leu.2403890
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2403890
Keywords
This article is cited by
-
Current application of dexamethasone-incorporated drug delivery systems for enhancing bone formation
Journal of Pharmaceutical Investigation (2023)
-
What’s Old is New: The Past, Present and Future Role of Thalidomide in the Modern-Day Management of Multiple Myeloma
Targeted Oncology (2022)
-
The use of single armed observational data to closing the gap in otherwise disconnected evidence networks: a network meta-analysis in multiple myeloma
BMC Medical Research Methodology (2018)
-
Immunomodulatory drugs and the risk of serious infection in multiple myeloma: systematic review and meta-analysis of randomized and observational studies
Annals of Hematology (2018)
-
Myeloma and Bone Disease
Current Osteoporosis Reports (2017)