Abstract
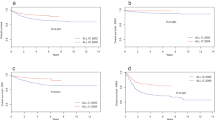
To assess the prognosis of overt testicular disease at diagnosis of acute lymphoblastic leukemia, and any therapeutic role of irradiation for this involvement, we reviewed the data of 811 boys treated on St Jude studies Total X–XI (early period) and Total XII-XIV (recent period). In all, 19 boys (2.3%) had testicular disease at diagnosis. In the early period, patients with testicular leukemia had a poorer overall survival (OS) (P=0.003), event-free survival (EFS) (P=0.064), and higher cumulative incidence of relapse (P=0.041) than did other patients. During the recent period, patients with and without overt testicular leukemia did not differ in OS (P=0.257), EFS (P=0.102), or cumulative incidence of relapse (P=0.51). In a multivariate analysis, OS was lower for patients with testicular disease than for those without the involvement in the early period (P=0.047) but not in the recent one (P=0.75). Both patients who received irradiation for residual testicular disease at the end of induction subsequently died of leukemia. Of the other 17 patients who did not receive irradiation, only one developed testicular relapse in combination with bone marrow relapse. In conclusion, the prognostic impact of overt testicular disease has diminished. Irradiation appears to provide no survival advantage to this patient population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Gajjar A, Ribeiro RC, Mahmoud HH, Sandlund JT, Liu Q, Furman WL et al. Overt testicular disease at diagnosis is associated with high-risk features and a poor prognosis in patients with childhood acute lymphoblastic leukemia. Cancer 1996; 78: 2437–2442.
Donadieu J, Auclerc MF, Baruchel A, Leblanc T, Landman-Parker J, Perel Y et al. Critical study of prognostic factors in childhood acute lymphoblastic leukaemia: differences in outcome are poorly explained by the most significant prognostic variables. Fralle group. French Acute Lymphoblastic Leukaemia study group. Br J Haematol 1998; 102: 729–739.
Pui CH, Relling MV, Downing JR . Acute lymphoblastic leukemia. N Engl J Med 2004; 350: 1535–1548.
Pui CH, Sandlund JT, Pei D, Campana D, Rivera GK, Ribeiro RC et al. Improved outcome for children with acute lymphoblastic leukemia: results of Total Therapy Study XIIIB at St Jude Children's Research Hospital. Blood 2004; 104: 2690–2696.
Schrappe M, Reiter A, Ludwig WD, Harbott J, Zimmermann M, Hiddemann W et al. Improved outcome in childhood acute lymphoblastic leukemia despite reduced use of anthracyclines and cranial radiotherapy: results of trial ALL-BFM 90. German-Austrian-Swiss ALL-BFM Study Group. Blood 2000; 95: 3310–3322.
Silverman LB, Gelber RD, Dalton VK, Asselin BL, Barr RD, Clavell LA et al. Improved outcome for children with acute lymphoblastic leukemia: results of Dana-Farber Consortium Protocol 91-01. Blood 2001; 97: 1211–1218.
Pui CH, Dodge RK, Look AT, George SL, Rivera GK, Abromowitch M et al. Risk of adverse events in children completing treatment for acute lymphoblastic leukemia: St Jude Total Therapy studies VIII, IX, and X. J Clin Oncol 1991; 9: 1341–1347.
Pui CH, Simone JV, Hancock ML, Evans WE, Williams DL, Bowman WP et al. Impact of three methods of treatment intensification on acute lymphoblastic leukemia in children: long-term results of St Jude total therapy study X. Leukemia 1992; 6: 150–157.
Rivera GK, Raimondi SC, Hancock ML, Behm FG, Pui CH, Abromowitch M et al. Improved outcome in childhood acute lymphoblastic leukaemia with reinforced early treatment and rotational combination chemotherapy. Lancet 1991; 337: 61–66.
Evans WE, Relling MV, Rodman JH, Crom WR, Boyett JM, Pui CH . Conventional compared with individualized chemotherapy for childhood acute lymphoblastic leukemia. N Engl J Med 1998; 338: 499–505.
Pui CH, Mahmoud HH, Rivera GK, Hancock ML, Sandlund JT, Behm FG et al. Early intensification of intrathecal chemotherapy virtually eliminates central nervous system relapse in children with acute lymphoblastic leukemia. Blood 1998; 92: 411–415.
Kishi S, Griener J, Cheng C, Das S, Cook EH, Pei D et al. Homocysteine, pharmacogenetics, and neurotoxicity in children with leukemia. J Clin Oncol 2003; 21: 3084–3091.
Peto R, Pike MC, Armitage P, Breslow NE, Cox DR, Howard SV et al. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. II. analysis and examples. Br J Cancer 1977; 35: 1–39.
Mantel N . Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep 1966; 50: 163–170.
Cox DR . Regression models and life tables. J Roy Stat Soc Ser B 1972; 20: 187–220.
Kalbfleisch JD, Prentice RL . The Statistical Analysis of Failure Time Data. New York: John Wiley & Sons, 1980.
Gray RJ . A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 1988; 16: 1141–1154.
Fine JP, Gray RJ . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Grundy RG, Leiper AD, Stanhope R, Chessells JM . Survival and endocrine outcome after testicular relapse in acute lymphoblastic leukaemia. Arch Dis Child 1997; 76: 190–196.
Castillo LA, Craft AW, Kernahan J, Evans RG, Aynsley-Green A . Gonadal function after 12-Gy testicular irradiation in childhood acute lymphoblastic leukaemia. Med Pediatr Oncol 1990; 18: 185–189.
Abromowitch M, Ochs J, Pui CH, Fairclough D, Murphy SB, Rivera GK . Efficacy of high-dose methotrexate in childhood acute lymphocytic leukemia: analysis by contemporary risk classifications. Blood 1988; 71: 866–869.
Dordelmann M, Reiter A, Zimmermann M, Fengler R, Henze G, Riehm H et al. Intermediate dose methotrexate is as effective as high dose methotrexate in preventing isolated testicular relapse in childhood acute lymphoblastic leukemia. J Pediatr Hematol Oncol 1998; 20: 444–450.
Freeman AI, Boyett JM, Glicksman AS, Brecher ML, Leventhal BG, Sinks LF et al. Intermediate-dose methotrexate versus cranial irradiation in childhood acute lymphoblastic leukemia: a ten-year follow-up. Med Pediatr Oncol 1997; 28: 98–107.
Pui CH, Campana D, Downing JR . Childhood acute lymphoblastic leukaemia-current status and future perspectives. Lancet Oncol 2001; 2: 597–607.
Acknowledgements
We thank Julia Cay Jones, PhD, for her expert editorial review; James Boyett, PhD, and Deo Kumar Srivastava, PhD, for helpful suggestions concerning the statistical analysis; Imella Smith Herrington for her assistance in manuscript preparation; Jeana Cromer for her administrative assistance; and Annette Stone and Gena Durham for data collection. This work was supported in part by a Cancer Center Support Grant (CA21765) from the National Cancer Institute and by the American Lebanese Syrian Associated Charities (ALSAC). Ching-Hon Pui is the American Cancer Society FM Kirby Clinical Research Professor.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hijiya, N., Liu, W., Sandlund, J. et al. Overt testicular disease at diagnosis of childhood acute lymphoblastic leukemia: lack of therapeutic role of local irradiation. Leukemia 19, 1399–1403 (2005). https://doi.org/10.1038/sj.leu.2403843
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2403843
Keywords
This article is cited by
-
St. Jude Total Therapy studies from I to XVII for childhood acute lymphoblastic leukemia: a brief review
Journal of the Egyptian National Cancer Institute (2022)
-
Overt testicular disease at diagnosis in childhood acute lymphoblastic leukemia: prognostic significance and role of testicular irradiation
The Indian Journal of Pediatrics (2010)