Abstract
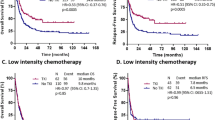
Two distinct forms of fms-like tyrosine kinase (FLT3) gene aberrations, internal tandem duplication (ITD) and tyrosine kinase domain (TKD) mutations, have been recognized in a substantial proportion of patients with acute myeloid leukemia (AML). To investigate their prognostic significance, we performed a meta-analysis of the four published studies that provided survival information according to the FLT3 status: ITD, TKD mutation, and wild type. The summary hazard ratios for disease-free survival (DFS) were 1.88 (95% confidence interval (CI) 1.58–2.23; P<0.001) for FLT3 mutations, 1.86 (95% CI: 1.52–2.29; P<0.001) for ITD, and 1.90 (95% CI: 1.40–2.60; P<0.001) for TKD mutation. The corresponding ratios for overall survival were 1.61 (95% CI: 1.37–1.89; P<0.001), 1.68 (95% CI: 1.39–2.03; P<0.001), and 1.37 (95% CI: 0.94–2.01; P=0.104). Neither white blood cell count at diagnosis nor cytogenetic risk category was a significant source of heterogeneity. These findings indicate that FLT3 mutations have an adverse effect on the outcome for AML, and that the negative impact of TKD mutation seems comparable to that of ITD with regard to DFS. Although it should be borne in mind that this meta-analysis was based on data abstracted from observational studies, these results may justify the risk-adapted therapeutic strategies for AML according to the FLT3 status.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood 1998; 92: 2322–2333.
Bloomfield CD, Lawrence D, Byrd JC, Carroll A, Pettenati MJ, Tantravahi R et al. Frequency of prolonged remission duration after high-dose cytarabine intensification in acute myeloid leukemia varies by cytogenetic subtype. Cancer Res 1998; 58: 4173–4179.
Lowenberg B, Downing JR, Burnett A . Acute myeloid leukemia. N Engl J Med 1999; 341: 1051–1062.
Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 2000; 96: 4075–4083.
Grimwade D, Walker H, Harrison G, Oliver F, Chatters S, Harrison CJ et al. The predictive value of hierarchical cytogenetic classification in older adults with acute myeloid leukemia (AML): analysis of 1065 patients entered into the United Kingdom Medical Research Council AML11 trial. Blood 2001; 98: 1312–1320.
Kiyoi H, Naoe T . FLT3 in human hematologic malignancies. Leuk Lymphoma 2002; 43: 1541–1547.
Kottaridis PD, Gale RE, Linch DC . Flt3 mutations and leukaemia. Br J Haematol 2003; 122: 523–538.
Naoe T, Kiyoi H . Normal and oncogenic FLT3. Cell Mol Life Sci 2004; 61: 2932–2938.
Thiede C, Steudel C, Mohr B, Schaich M, Schakel U, Platzbecker U et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood 2002; 99: 4326–4335.
Frohling S, Schlenk RF, Breitruck J, Benner A, Kreitmeier S, Tobis K et al. Prognostic significance of activating FLT3 mutations in younger adults (16–60 years) with acute myeloid leukemia and normal cytogenetics: a study of the AML Study Group Ulm. Blood 2002; 100: 4372–4380.
Moreno I, Martin G, Bolufer P, Barragan E, Rueda E, Roman J et al. Incidence and prognostic value of FLT3 internal tandem duplication and D835 mutations in acute myeloid leukemia. Haematologica 2003; 88: 19–24.
Beran M, Luthra R, Kantarjian H, Estey E . FLT3 mutation and response to intensive chemotherapy in young adult and elderly patients with normal karyotype. Leuk Res 2004; 28: 547–550.
Chillon MC, Fernandez C, Garcia-Sanz R, Balanzategui A, Ramos F, Fernandez-Calvo J et al. FLT3-activating mutations are associated with poor prognostic features in AML at diagnosis but they are not an independent prognostic factor. Hematol J 2004; 5: 239–246.
Sheikhha MH, Awan A, Tobal K, Liu Yin JA . Prognostic significance of FLT3 ITD and D835 mutations in AML patients. Hematol J 2003; 4: 41–46.
Kiyoi H, Naoe T, Nakano Y, Yokota S, Minami S, Miyawaki S et al. Prognostic implication of FLT3 and N-RAS gene mutations in acute myeloid leukemia. Blood 1999; 93: 3074–3080.
Abu-Duhier FM, Goodeve AC, Wilson GA, Gari MA, Peake IR, Rees DC et al. FLT3 internal tandem duplication mutations in adult acute myeloid leukaemia define a high-risk group. Br J Haematol 2000; 111: 190–195.
Rombouts WJ, Blokland I, Lowenberg B, Ploemacher RE . Biological characteristics and prognosis of adult acute myeloid leukemia with internal tandem duplications in the Flt3 gene. Leukemia 2000; 14: 675–683.
Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood 2001; 98: 1752–1759.
Whitman SP, Archer KJ, Feng L, Baldus C, Becknell B, Carlson BD et al. Absence of the wild-type allele predicts poor prognosis in adult de novo acute myeloid leukemia with normal cytogenetics and the internal tandem duplication of FLT3: a cancer and leukemia group B study. Cancer Res 2001; 61: 7233–7239.
Schnittger S, Schoch C, Dugas M, Kern W, Staib P, Wuchter C et al. Analysis of FLT3 length mutations in 1003 patients with acute myeloid leukemia: correlation to cytogenetics, FAB subtype, and prognosis in the AMLCG study and usefulness as a marker for the detection of minimal residual disease. Blood 2002; 100: 59–66.
Kainz B, Heintel D, Marculescu R, Schwarzinger I, Sperr W, Le T et al. Variable prognostic value of FLT3 internal tandem duplications in patients with de novo AML and a normal karyotype, t(15;17), t(8;21) or inv(16). Hematol J 2002; 3: 283–289.
Munoz L, Aventin A, Villamor N, Junca J, Acebedo G, Domingo A et al. Immunophenotypic findings in acute myeloid leukemia with FLT3 internal tandem duplication. Haematologica 2003; 88: 637–645.
Ciolli S, Vannucchi AM, Leoni F, Nozzoli C, Longo G, Salati A et al. Internal tandem duplications of Flt3 gene (Flt3/ITD) predicts a poor post-remission outcome in adult patients with acute nonpromyelocytic leukemia. Leuk Lymphoma 2004; 45: 73–78.
Yamamoto Y, Kiyoi H, Nakano Y, Suzuki R, Kodera Y, Miyawaki S et al. Activating mutation of D835 within the activation loop of FLT3 in human hematologic malignancies. Blood 2001; 97: 2434–2439.
Rombouts EJ, Pavic B, Lowenberg B, Ploemacher RE . Relation between CXCR-4 expression, Flt3 mutations, and unfavorable prognosis of adult acute myeloid leukemia. Blood 2004; 104: 550–557.
Frohling S, Schlenk RF, Stolze I, Bihlmayr J, Benner A, Kreitmeier S et al. CEBPA mutations in younger adults with acute myeloid leukemia and normal cytogenetics: prognostic relevance and analysis of cooperating mutations. J Clin Oncol 2004; 22: 624–633.
Stirewalt DL, Kopecky KJ, Meshinchi S, Appelbaum FR, Slovak ML, Willman CL et al. FLT3, RAS, and TP53 mutations in elderly patients with acute myeloid leukemia. Blood 2001; 97: 3589–3595.
Preudhomme C, Sagot C, Boissel N, Cayuela JM, Tigaud I, de Botton S et al. Favorable prognostic significance of CEBPA mutations in patients with de novo acute myeloid leukemia: a study from the Acute Leukemia French Association (ALFA). Blood 2002; 100: 2717–2723.
Boissel N, Cayuela JM, Preudhomme C, Thomas X, Grardel N, Fund X et al. Prognostic significance of FLT3 internal tandem repeat in patients with de novo acute myeloid leukemia treated with reinforced courses of chemotherapy. Leukemia 2002; 16: 1699–1704.
Barjesteh van Waalwijk van Doorn-Khosrovani S, Erpelinck C, Meijer J, van Oosterhoud S, van Putten WL, Valk PJ et al. Biallelic mutations in the CEBPA gene and low CEBPA expression levels as prognostic markers in intermediate-risk AML. Hematol J 2003; 4: 31–40.
Andersson A, Johansson B, Lassen C, Mitelman F, Billstrom R, Fioretos T . Clinical impact of internal tandem duplications and activating point mutations in FLT3 in acute myeloid leukemia in elderly patients. Eur J Haematol 2004; 72: 307–313.
Steudel C, Wermke M, Schaich M, Schakel U, Illmer T, Ehninger G et al. Comparative analysis of MLL partial tandem duplication and FLT3 internal tandem duplication mutations in 956 adult patients with acute myeloid leukemia. Genes Chromosomes Cancer 2003; 37: 237–251.
Care RS, Valk PJ, Goodeve AC, Abu-Duhier FM, Geertsma-Kleinekoort WM, Wilson GA et al. Incidence and prognosis of c-KIT and FLT3 mutations in core binding factor (CBF) acute myeloid leukaemias. Br J Haematol 2003; 121: 775–777.
Ozeki K, Kiyoi H, Hirose Y, Iwai M, Ninomiya M, Kodera Y et al. Biologic and clinical significance of the FLT3 transcript level in acute myeloid leukemia. Blood 2004; 103: 1901–1908.
Parmar MK, Torri V, Stewart L . Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 1998; 17: 2815–2834.
Hotta K, Matsuo K, Ueoka H, Kiura K, Tabata M, Tanimoto M . Meta-analysis of randomized clinical trials comparing Cisplatin to Carboplatin in patients with advanced non-small-cell lung cancer. J Clin Oncol 2004; 22: 3852–3859.
DerSimonian R, Laird N . Meta-analysis in clinical trials. Control Clin Trials 1986; 7: 177–188.
Begg CB, Mazumdar M . Operating characteristics of a rank correlation test for publication bias. Biometrics 1994; 50: 1088–1101.
Egger M, Davey Smith G, Schneider M, Minder C . Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634.
Bagrintseva K, Geisenhof S, Kern R, Eichenlaub S, Reindl C, Ellwart JW et al. FLT3-ITD-TKD dual mutants associated with AML confer resistance to FLT3 PTK inhibitors and cytotoxic agents by overexpression of Bcl-x(L). Blood 2005; 105: 3679–3685.
Acknowledgements
We are indebted to Drs Richard Schlenk and Konstanze Döhner (the AML Study Group Ulm) for providing additional data. We also thank Ms Mariko Nakano (Aichi Cancer Center Research Institute) for her technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yanada, M., Matsuo, K., Suzuki, T. et al. Prognostic significance of FLT3 internal tandem duplication and tyrosine kinase domain mutations for acute myeloid leukemia: a meta-analysis. Leukemia 19, 1345–1349 (2005). https://doi.org/10.1038/sj.leu.2403838
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2403838
Keywords
This article is cited by
-
TP-0184 inhibits FLT3/ACVR1 to overcome FLT3 inhibitor resistance and hinder AML growth synergistically with venetoclax
Leukemia (2024)
-
French Retrospective Database Analysis of Patient Characteristics and Treatment Patterns in Patients with R/R FLT3-Mutated AML: A Registry-Based Cohort Study
Oncology and Therapy (2023)
-
Perspectives and challenges of small molecule inhibitor therapy for FLT3-mutated acute myeloid leukemia
Annals of Hematology (2023)
-
FLT3-targeted treatment for acute myeloid leukemia
International Journal of Hematology (2022)
-
De novo adult acute myeloid leukemia with two new mutations in juxtatransmembrane domain of the FLT3 gene: a case report
Journal of Medical Case Reports (2021)