Abstract
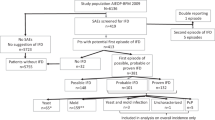
Risk factors for invasive aspergillosis (IA) are incompletely identified and may undergo changes due to differences in medical practice. A cohort of 189 consecutive, adult patients with neutropenia hospitalized in the hemato-oncology ward of the University hospital Berne between 1995 and 1999 were included in a retrospective study to assess risk factors for IA. In total, 45 IA cases (nine proven, three probable, 33 possible), 11 patients with refractory fever and 133 controls were analyzed. IA cases had more often acute leukemia or myelodysplastic syndrome (MDS) (88 vs 38%, P<0.001) and a longer duration of neutropenia (mean 20.6 vs 9.9 days, P<0.001). They also had fewer neutropenic episodes during the preceding 6 months (mean 0.42 vs 1.03, P<0.001), that is, confirmed (82%) and probable (73%) IA occurred most often during the induction cycle. A short time interval (⩽14 days) between neutropenic episodes increased the risk of IA four-fold (P=0.06). Bacteremia, however, was not related to the number of preceding neutropenic episodes. Therefore, neutropenic patients with leukemia or MDS have the highest risk of IA. The risk is highest during the first induction cycle of treatment and increases with short-time intervals between treatment cycles.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Bodey G, Bueltmann B, Duguid W, Gibbs D, Hanak H, Hotchi M et al. Fungal infections in cancer patients: an international autopsy survey. Eur J Clin Microbiol Dis 1992; 11: 99–109.
Denning DW . Invasive aspergillosis. Clin Infect Dis 1998; 26: 781–805.
Denning DW . Therapeutic outcome in invasive aspergillosis. Clin Infect Dis 1996; 23: 608–615.
von Eiff M, Roos N, Schulten R, Hesse M, Zuhlsdorf M, van de Loo J . Pulmonary aspergillosis: early diagnosis improves survival. Respiration 1995; 62: 341–347.
Prentice HG, Kibbler CC, Prentice AG . Towards a targeted, risk-based, antifungal strategy in neutropenic patients. Br J Haematol 2000; 110: 273–284.
Gerson SL, Talbot GH, Hurwitz S, Strom BL, Lusk EJ, Cassileth PA . Prolonged granulocytopenia: the major risk factor for invasive aspergillosis in patients with acute leukemia. Ann Int Med 1984; 100: 345–351.
Baddley JW, Stroud TP, Salzmann D, Pappas PG . Invasive mold infections in allogenic bone marrow transplant recipients. Clin Infect Dis 2001; 32: 1319–1324.
Roilides E, Uhlig K, Venzon D, Pizzo PA, Walsh TJ . Prevention of corticosteroid-induced suppression of human polymorphonuclear leukocyte-induced damage of Aspergillus fumigatus hyphae by granulocyte colony-stimulating factor and gamma interferon. Infect Immun 1993; 61: 4870–4877.
Ng TT, Robson GD, Denning DW . Hydrocortisone-enhanced growth of Aspergillus spp.: implications for pathogenesis. Microbiology 1994; 140: 2475–2479.
Bow EJ, Loewen R, Cheang MS, Schacter B . Invasive fungal disease in adults undergoing remission-induction therapy for acute myeloid leukemia: the pathogenetic role of the antileukemic regimen. Clin Infect Dis 1995; 21: 316–319.
Coiffier B, Frobert Y, Revol L . Polymorphonuclear function in acute myeloblastic leukemia. Biomedicine 1977; 27: 94–96.
Warnock DW, Hajjeh RA, Lasker BA . Epidemiology and prevention of invasive aspergillosis. Curr Infect Dis Rep 2001; 3: 507–516.
Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F et al. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis 2002; 34: 7–14.
Charlson ME, Pompei P, Ales KL, MacKenzie CR . A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383.
Denning DW, Marinus A, Cohen J, Spence D, Herbrecht R, Pagano L et al. An EORTC multicentre prospective survey of invasive aspergillosis in haematological patients: diagnosis and therapeutic outcome. EORTC Invasive Fungal Infections Cooperative Group. J Infect 1998; 37: 173–180.
Lortholary O, Ascioglu S, Moreau P, Herbrecht R, Marinus A, Casassus P et al. Invasive aspergillosis as an opportunistic infection in nonallografted patients with multiple myeloma: a European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the Intergroupe Francais du Myelome. Clin Infect Dis 2000; 30: 41–46.
Wiley JM, Smith N, Leventhal BG, Graham ML, Strauss LC, Hurwitz CA et al. Invasive fungal disease in pediatric acute leukemia patients with fever and neutropenia during induction chemotherapy: a multivariante analysis of risk factors. J Clin Oncol 1990; 8: 280–286.
Oren I, Haddad N, Finkelstein R, Rowe JM . Invasive pulmonary aspergillosis in neutropenic patients during hospital construction: before and after chemoprophylaxis and institution of HEPA filters. Am J Hematol 2001; 66: 257–262.
Pagano L, Girmenia C, Mele L, Ricci P, Tosti ME, Nosari A, et al., GIMEMA Infection Program, Gruppo Italiano Malattie Ematologiche dell’Adulto. Infections caused by filamentous fungi in patients with hematologic malignancies. A report of 391 cases by GIMEMA Infection Program. Haematologica 2001; 86: 862–870.
Martino P, Raccah R, Gentile G, Venditti M, Girmenia C, Mandelli F . Aspergillus colonization of the nose and pulmonary aspergillosis in neutropenic patients: a retrospective study. Haematologica 1989; 74: 263–265.
Leenders AC, van Belkum A, Behrendt M, Luijendijk A, Verbrugh HA . Density and molecular epidemiology of aspergillus in air and relationship to outbreaks of aspergillus infection. J Clin Microbiol 1999; 37: 1752–1757.
de Repentigny L, Petitbois S, Boushira M, Michaliszyn E, Senechal S, Gendron N et al. Acquired immunity in experimental murine aspergillosis is mediated by macrophages. Infect Immun 1993; 6: 3791–3802.
Marr KA, Carter RA, Crippa F, Wald A, Corey L . Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis 2002; 34: 909–917.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mühlemann, K., Wenger, C., Zenhäusern, R. et al. Risk factors for invasive aspergillosis in neutropenic patients with hematologic malignancies. Leukemia 19, 545–550 (2005). https://doi.org/10.1038/sj.leu.2403674
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2403674
Keywords
This article is cited by
-
Age difference of patients with and without invasive aspergillosis: a systematic review and meta-analysis
BMC Infectious Diseases (2024)
-
Post-hoc analysis of the safety and efficacy of isavuconazole in older patients with invasive fungal disease from the VITAL and SECURE studies
Scientific Reports (2023)
-
Optimization of a Quantitative PCR Methodology for Detection of Aspergillus spp. and Rhizopus arrhizus
Molecular Diagnosis & Therapy (2022)
-
Genetic Risk Surveillance for Invasive Aspergillosis in Hematology Patients: A Prospective Observational Study
Infectious Diseases and Therapy (2020)
-
Modulation of Immune Signaling and Metabolism Highlights Host and Fungal Transcriptional Responses in Mouse Models of Invasive Pulmonary Aspergillosis
Scientific Reports (2017)