Abstract
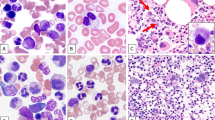
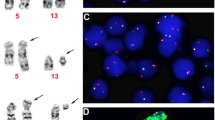
Molecular and genetic events associated with the transition from monoclonal gammopathy of undetermined significance (MGUS) to multiple myeloma (MM) are still poorly characterized. We investigated serial bone marrow specimens from 11 patients with MGUS who eventually progressed to MM (MM post-MGUS) by interphase fluorescence in situ hybridization for immunoglobulin heavy-chain gene (IgH) translocations and chromosome 13q deletions (del(13q)). In nine patients, IgH translocations were present both in MGUS and MM post-MGUS plasma cells, including three t(11;14)(q13;q32) and one t(4;14)(p16;q32), which was observed already 92 months prior to MM. Similarly, all five MM patients with del(13q) had this aberration already at the MGUS stage. Two patients without IgH translocation and del(13q) had chromosomal gains suggesting hyperdiploidy, but IgH translocations and/or del(13q) did not emerge at MM post-MGUS. IgH translocations and del(13q) are early genetic events in monoclonal gammopathies, suggesting that additional events are required for the transition from stable MGUS to progressive MM.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Kyle RA, Therneau TM, Rajkumar SV, Offord JR, Larson DR, Plevak MF et al. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med 2002; 346: 564–569.
Seidl S, Kaufmann H, Drach J . New insights into the pathophysiology of multiple myeloma. Lancet Oncol 2003; 4: 557–564.
Fonseca R, Barlogie B, Bataille R, Bastard C, Bergsagel PL, Chesi M et al. Genetics and cytogenetics of multiple myeloma: a workshop report. Cancer Res 2004; 64: 1546–1558.
Hallek M, Bergsagel PL, Anderson KC . Multiple myeloma: increasing evidence for a multistep transformation process. Blood 1998; 91: 3–21.
Kuehl WM, Bergsagel PL . Multiple myeloma: evolving genetic events and host interactions. Nat Rev Cancer 2002; 2: 175–187.
Fonseca R, Bailey RJ, Ahmann GJ, Rajkumar V, Hoyer JD, Lust LA et al. Genomic abnormalities in monoclonal gammopathy of undetermined significance. Blood 2002; 100: 1417–1424.
Avet-Loiseau H, Facon T, Daviet A, Godon C, Rapp MJ, Harousseau JL et al. 14q32 translocations and monosomy 13 observed in monoclonal gammopathy of undetermined significance delineate a multistep process for the oncogenesis of multiple myeloma. Cancer Res 1999; 59: 4546–4550.
Königsberg R, Ackermann J, Kaufmann H, Zojer N, Urbauer E, Krömer E et al. Deletions of chromosome 13q in monoclonal gammopathy of undetermined significance. Leukemia 2000; 14: 1975–1979.
Avet-Loiseau H, Li JY, Morineau N, Facon T, Brigaudeau C, Harousseau JL et al. Monosomy 13 is associated with the transition of monoclonal gammopathy of undetermined significance to multiple myeloma. Blood 1999; 94: 2583–2589.
Bernasconi P, Cavigliano PM, Boni M, Astori C, Calatroni S, Giardini I et al. Long-term follow up with conventional cytogenetics and band 13q14 interphase/metaphase in situ hybridization monitoring in monoclonal gammopathies of undetermined significance. Br J Haematol 2002; 118: 545–549.
International-Myeloma-Working-Group. Criteria for the classification of monoclonal gammopathies, multiple myeloma, and related disorders: a report of the International Myeloma Working Group. Br J Haematol 2003; 121: 749–757.
Fonseca R, Debes-Marun CS, Picken EB, Dewald GW, Bryant SC, Winkler JM et al. The recurrent IgH translocations are highly associated with nonhyperdiploid variant of multiple myeloma. Blood 2003; 102: 2562–2567.
Kaufmann H, Ackermann J, Nosslinger T, Kromer E, Zojer N, Schreiber S et al. Absence of clonal chromosomal relationship between concomitant B-CLL and multiple myeloma – a report on two cases. Ann Hematol 2001; 80: 474–478.
Zojer N, Konigsberg R, Ackermann J, Fritz E, Dallinger S, Kromer E et al. Deletion of 13q14 remains an independent adverse prognostic variable in multiple myeloma despite its frequent detection by interphase fluorescence in situ hybridization. Blood 2000; 95: 1925–1930.
Moreau P, Facon T, Leleu X, Morineau N, Huyghe P, Harousseau JL et al. Intergroupe Francophone du Myelome. Recurrent 14q32 translocations determine the prognosis of multiple myeloma, especially in patients receiving intensive chemotherapy. Blood 2002; 100: 1579–1583.
Fonseca R, Blood E, Rue M, Harrington D, Oken MM, Kyle RA et al. Clinical and biological implications of recurrent genomic aberrations in myeloma. Blood 2003; 101: 4569–4575.
Chang H, Sloan S, Li D, Zhuang L, Yi QL, Chen CI et al. The t(4;14) is associated with poor prognosis in myeloma patients undergoing autologous stem cell transplantation. Br J Haematol 2004; 125: 64–68.
Drach J, Angerler J, Schuster J, Rothermundt C, Thalhammer R, Haas OA et al. Interphase fluorescence in situ hybridization identifies chromosomal abnormalities in plasma cells from patients with monoclonal gammopathy of undetermined significance. Blood 1995; 86: 3915–3921.
Zandecki M, Lai JL, Genevieve F, Bernardi F, Volle-Remy H, Blanchet O et al. Several cytogenetic subclones may be identified within plasma cells from patients with monoclonal gammopathy of undetermined significance, both at diagnosis and during the indolent course of this condition. Blood 1997; 90: 3682–3690.
Rasillo A, Tabernero MD, Sanchez ML, Perez de Andres M, Martin Ayuso M, Hernandez J et al. Fluorescence in situ hybridization analysis of aneuploidization patterns in monoclonal gammopathy of undetermined significance versus multiple myeloma and plasma cell leukemia. Cancer 2003; 97: 601–609.
Seidl S, Ackermann J, Kaufmann H, Keck A, Nosslinger T, Zielinski CC et al. DNA-methylation analysis identifies the E-cadherin gene as a potential marker of disease progression in patients with monoclonal gammopathies. Cancer 2004; 100: 2598–2606.
Davies FE, Dring AM, Li C, Rawstron AC, Shammas MA, O’Connor SM et al. Insights into the multistep transformation of MGUS to myeloma using microarray expression analysis. Blood 2003; 102: 4504–4511.
Acknowledgements
This work was supported in part by grants from the Austrian National Bank (Jubiläumsfonds Project # 7730), CLEXO (Center of excellence in clinical and experimental oncology) and UNRUHE Privatstiftung.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaufmann, H., Ackermann, J., Baldia, C. et al. Both IGH translocations and chromosome 13q deletions are early events in monoclonal gammopathy of undetermined significance and do not evolve during transition to multiple myeloma. Leukemia 18, 1879–1882 (2004). https://doi.org/10.1038/sj.leu.2403518
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2403518
Keywords
This article is cited by
-
Plasma cell neoplasms and related entities—evolution in diagnosis and classification
Virchows Archiv (2023)
-
An enhanced genetic model of relapsed IGH-translocated multiple myeloma evolutionary dynamics
Blood Cancer Journal (2020)
-
Prognostic impact of hyperdiploidy in multiple myeloma patients with high-risk cytogenetics: a pilot study in China
Journal of Cancer Research and Clinical Oncology (2018)
-
Impact of primary molecular cytogenetic abnormalities and risk of progression in smoldering multiple myeloma
Leukemia (2013)
-
SNP-based mapping arrays reveal high genomic complexity in monoclonal gammopathies, from MGUS to myeloma status
Leukemia (2012)