Abstract
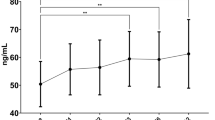
The osteoprotegerin (OPG)/receptor activator of NF-kappa B ligand (RANKL) system has a major role in the pathogenesis of bone disease in myeloma (MM). The effect of autologous stem cell transplantation (ASCT) on bone turnover in MM was evaluated in 51 patients (35M/16F). Markers of bone resorption (NTX, TRACP-5b), bone formation (bone-alkaline phosphatase (bALP), osteocalcin), OPG and sRANKL were measured pre- and every month post-ASCT. The median follow-up period was 12 months. Four patients were transplanted in CR, 44 were transplanted in PR and three patients had progressive/resistant disease. All patients received bisphosphonates both pre- and post-ASCT. At baseline the majority of patients had increased NTX, TRACP-5b levels, and sRANKL/OPG ratio, while markers of bone formation were strongly suppressed. ASCT produced a significant reduction of sRANKL/OPG ratio, with a concomitant decrease of NTX, and TRACP-5b levels, starting the second month post-ASCT. Bone formation markers, osteocalcin and bALP, started to increase after the 9th and 11th month post-ASCT, respectively, while the increase of OPG preceded this. These results provide biochemical evidence that ASCT normalizes the abnormal bone resorption in MM patients possibly through the decrease of RANKL/OPG ratio, while bone formation requires a longer period to return to normal.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Ashcroft AJ, Davies FE, Morgan GJ . Aetiology of bone disease and the role of bisphosphonates in multiple myeloma. Lancet Oncol 2003; 4: 284–292.
Kuehl WM, Bergsagel PL . Multiple myeloma: evolving genetic events and host interactions. Nat Rev Cancer 2002; 2: 175–187.
Michigami T, Shimizu N, Williams PJ, Niewolna M, Dallas SL, Mundy GR et al. Cell–cell contact between marrow stromal cells and myeloma cells via VCAM-1 and alpha(4)beta(1)-integrin enhances production of osteoclast-stimulating activity. Blood 2000; 96: 1953–1960.
Terpos E, Politou M, Szydlo R, Goldman JM, Apperley JF, Rahemtulla A . Serum levels of macrophage inflammatory protein-1 alpha (MIP-1alpha) correlate with the extent of bone disease and survival in patients with multiple myeloma. Br J Haematol 2003; 123: 106–109.
Hsu H, Lacey DL, Dunstan CR, Solovyev I, Colombero A, Timms E et al. Tumor necrosis factor receptor family member RANK mediates osteoclast differentiation and activation induced by osteoprotegerin ligand. Proc Natl Acad Sci USA 1999; 96: 3540–3545.
Vanderkerken K, Asosingh K, Croucher P, Van Camp B . Multiple myeloma biology: lessons from the 5TMM models. Immunol Rev 2003; 194: 196–206.
Kim N, Odgren PR, Kim DK, Marks Jr SC, Choi Y . Diverse roles of the tumor necrosis factor family member TRANCE in skeletal physiology revealed by TRANCE deficiency and partial rescue by a lymphocyte-expressed TRANCE transgene. Proc Natl Acad Sci USA 2000; 97: 10905–10910.
Sezer O, Heider U, Zavrski I, Kuhne CA, Hofbauer LC . RANK ligand and osteoprotegerin in myeloma bone disease. Blood 2003; 101: 2094–2098.
Pearse RN, Sordillo EM, Yaccoby S, Wong BR, Liau DF, Colman N et al. Multiple myeloma disrupts the TRANCE/osteoprotegerin cytokine axis to trigger bone destruction and promote tumor progression. Proc Natl Acad Sci USA 2001; 98: 11581–11586.
Vanderkerken K, De Leenheer E, Shipman C, Asosingh K, Willems A, Van Camp B et al. Recombinant osteoprotegerin decreases tumor burden and increases survival in a murine model of multiple myeloma. Cancer Res 2003; 63: 287–289.
Terpos E, Szydlo R, Apperley JF, Hatjiharissi E, Politou M, Meletis J et al. Soluble receptor activator of nuclear factor kappa-B ligand-osteoprotegerin ratio predicts survival in multiple myeloma: proposal for a novel prognostic index. Blood 2003; 102: 1064–1069.
Grimaud E, Soubigou L, Couillaud S, Coipeau P, Moreau A, Passuti N et al. Receptor activator of nuclear factor kappaB ligand (RANKL)/osteoprotegerin (OPG) ratio is increased in severe osteolysis. Am J Pathol 2003; 163: 2021–2031.
Sezer O, Heider U, Jakob C, Zavrski I, Eucker J, Possinger K et al. Immunocytochemistry reveals RANKL expression of myeloma cells. Blood 2002; 99: 4646–4647, (letter).
Heider U, Langelotz C, Jakob C, Zavrski I, Fleissner C, Eucker J et al. Expression of receptor activator of nuclear factor kappaB ligand on bone marrow plasma cells correlates with osteolytic bone disease in patients with multiple myeloma. Clin Cancer Res 2003; 9: 1436–1440.
Farrugia AN, Atkins GJ, To LB, Pan B, Horvath N, Kostakis P et al. Receptor activator of nuclear factor-κB ligand expression by human myeloma cells mediates osteoclast formation in vitro and correlates with bone destruction in vivo. Cancer Res 2003; 63: 5438–5445.
Attal M, Harousseau JL, Stoppa AM, Sotto JJ, Fuzibet JG, Rossi JF et al. A prospective, randomised trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Francais du Myelome. N Engl J Med 1996; 335: 91–97.
Child JA, Morgan GJ, Davies FE, Owen RG, Bell SE, Hawkins K, et al. Medical Research Council Adult Leukaemia Working Party. High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N Engl J Med 2003; 348: 1875–1883.
Clark RE, Flory AJ, Ion EM, Woodcock BE, Durham BH, Fraser WD . Biochemical markers of bone turnover following high-dose chemotherapy and autografting in multiple myeloma. Blood 2000; 96: 2697–2702.
Gandhi MK, Lekamwasam S, Inman I, Kaptoge S, Sizer L, Love S et al. Significant and persistent loss of bone mineral density in the femoral neck after haematopoietic stem cell transplantation: long-term follow-up of a prospective study. Br J Haematol 2003; 121: 462–468.
Blade J, Samson D, Reece D, Apperley J, Bjorkstrand B, Gahrton G et al. Criteria for evaluating disease response and progression in patients with multiple myeloma treated by high-dose therapy and haemopoietic stem cell transplantation. Myeloma Subcommittee of the EBMT. Br J Haematol 1998; 102: 1115–1123.
Roux S, Meignin V, Quillard J, Meduri G, Guiochon-Mantel A, Fermand JP et al. RANK (receptor activator of nuclear factor-jB) and RANKL expression in multiple myeloma. Br J Haematol 2002; 117: 86–92.
Terpos E, Politou M, Rahemtulla A . New insights into the pathophysiology and management of bone disease in multiple myeloma. Br J Haematol 2003; 123: 758–769.
Terpos E, Palermos J, Viniou N, Vaiopoulos G, Meletis J, Yataganas X . Pamidronate increases markers of bone formation in patients with multiple myeloma in plateau phase under interferon-alpha treatment. Calcif Tissue Int 2001; 68: 285–290.
Abildgaard N, Glerup H, Rungby J, Bendix-Hansen K, Kassem M, Brixen K et al. Biochemical markers of bone metabolism reflect osteoclastic and osteoblastic activity in multiple myeloma. Eur J Haematol 2000; 64: 121–129.
Halleen JM, Alatalo SL, Suominen H, Cheng S, Janckila AJ, Vaananen HK . Tartrate-resistant acid phosphatase 5b: a novel serum marker of bone resorption. J Bone Miner Res 2000; 15: 1337–1345.
Silvestris F, Cafforio P, Tucci M, Grinello D, Dammacco F . Upregulation of osteoblast apoptosis by malignant plasma cells: a role in myeloma bone disease. Br J Haematol 2003; 122: 39–52.
Tian E, Zhan F, Walker R, Rasmussen E, Ma Y, Barlogie B et al. The role of the Wnt-signaling antagonist DKK1 in the development of osteolytic lesions in multiple myeloma. N Engl J Med 2003; 349: 2483–2494.
Carlson K, Simonsson B, Ljunghall S . Acute effects of high-dose chemotherapy followed by bone marrow transplantation on serum markers of bone metabolism. Calcif Tissue Int 1994; 55: 408–411.
Banfi A, Bianchi G, Galotto M, Cancedda R, Quarto R . Bone marrow stromal damage after chemo/radiotherapy: occurrence, consequences and possibilities of treatment. Leuk Lymphoma 2001; 42: 863–870.
Rosen LS, Gordon D, Kaminski M, Howell A, Belch A, Mackey J et al. Long-term efficacy and safety of zoledronic acid compared with pamidronate disodium in the treatment of skeletal complications in patients with advanced multiple myeloma or breast carcinoma: a randomized, double-blind, multicenter, comparative trial. Cancer 2003; 98: 1735–1744.
Pan B, Farrugia AN, To LB, Findlay DM, Green J, Lynch K et al. The nitrogen-containing bisphosphonate, zoledronic acid, influences RANKL expression in human osteoblast-like cells by activating TNF-alpha converting enzyme (TACE). J Bone Miner Res 2004; 19: 147–154.
Croucher PI, De Hendrik R, Perry MJ, Hijzen A, Shipman CM, Lippitt J et al. Zoledronic acid treatment of 5T2MM-bearing mice inhibits the development of myeloma bone disease: evidence for decreased osteolysis, tumor burden and angiogenesis, and increased survival. J Bone Miner Res 2003; 18: 482–492.
Salomo M, Jurlander J, Nielsen LB, Gimsing P . How myeloma cells escape bisphosphonate-mediated killing: development of specific resistance with preserved sensitivity to conventional chemotherapeutics. Br J Haematol 2003; 122: 202–210.
Viereck V, Emons G, Lauck V, Frosch KH, Blaschke S, Grundker C et al. Bisphosphonates pamidronate and zoledronic acid stimulate osteoprotegerin production by primary human osteoblasts. Biochem Biophys Res Commun 2002; 291: 680–686.
Ebeling PR, Thomas DM, Erbas B, Hopper JL, Szer J, Grigg AP . Mechanisms of bone loss following allogeneic and autologous hemopoietic stem cell transplantation. J Bone Miner Res 1999; 14: 342–350.
Author information
Authors and Affiliations
Corresponding author
Additional information
The paper has been presented as a poster presentation in the American Society of Hematology Annual Meeting 2003 in San Diego: ‘Autologous Stem Cell Transplantation normalizes abnormal bone resorption through the reduction of sRANKL/osteoprotegerin ratio in multiple myeloma’ (Blood 2003; 102: abstract no. 3658).
Rights and permissions
About this article
Cite this article
Terpos, E., Politou, M., Szydlo, R. et al. Autologous stem cell transplantation normalizes abnormal bone remodeling and sRANKL/osteoprotegerin ratio in patients with multiple myeloma. Leukemia 18, 1420–1426 (2004). https://doi.org/10.1038/sj.leu.2403423
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2403423
Keywords
This article is cited by
-
Prognostic and predictive biomarker developments in multiple myeloma
Journal of Hematology & Oncology (2021)
-
Comparison of 18F-sodium fluoride uptake in the whole bone, pelvis, and femoral neck of multiple myeloma patients before and after high-dose therapy and conventional-dose chemotherapy
European Journal of Nuclear Medicine and Molecular Imaging (2020)
-
Pathogenesis of bone disease in multiple myeloma: from bench to bedside
Blood Cancer Journal (2018)
-
Myeloma and Bone Disease
Current Osteoporosis Reports (2017)
-
Treatment response evaluation with 18F-FDG PET/CT and 18F-NaF PET/CT in multiple myeloma patients undergoing high-dose chemotherapy and autologous stem cell transplantation
European Journal of Nuclear Medicine and Molecular Imaging (2017)