Abstract
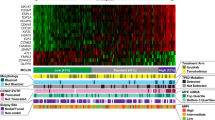
Mantle cell lymphoma (MCL) is a moderately aggressive B-cell lymphoma that responds poorly to currently used therapeutic protocols. In order to identify tumour characteristics that improve the understanding of biology of MCL, analysis of oligonucleotide microarrays were used to define specific gene expression profiles. Biopsy samples of MCL cases were compared to reactive lymphoid tissue. Among genes differentially expressed in MCL were genes that are involved in the regulation of proliferation, cell signalling, adhesion and homing. Furthermore, some genes with previously unknown function, such as C11orf32, C2orf10, TBC1D9 and ABCA6 were found to be differentially expressed in MCL compared to reactive lymphoid tissue. Of special interest was the high expression of the cannabinoid receptor 1 (CB1) gene in all MCL cases analysed. These results were further confirmed at the cellular and protein level by immunocytochemical staining and immunoblotting of MCL cells. Furthermore, there was a reduced expression of a regulator of G protein signalling, RGS13 in all MCLs, with a complete absence in the majority of cases while present in control lymphoid tissue. These results were further confirmed by PCR. Sequencing of the RGS13 gene revealed changes suggesting polymorphisms, indicating that downregulation of the expression of RGS13 is not related to mutations, but may serve as a new specific marker for MCL. Moreover, comparison between individual cases of MCL, revealed that the CCND1 gene appears to be differently expressed in MCL cases with high vs low proliferative activity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Walsh S, Thorselius M, Johnson A, Söderberg O, Jerkeman M, Björk E et al. Mutated VH genes and preferential VH3-21 usage define new subsets of mantle cell lymphoma. Blood 2003; 101: 4047–4054.
Leonard JP, Schattner EJ, Coleman M . Biology and management of mantle cell lymphoma. Curr Opin Oncol 2001; 13: 342–347.
Rosenberg CL, Wong E, Petty EM, Bale AE, Tsujimoto Y, Harris NL et al. PRAD1, a candidate BCL1 oncogene: mapping and expression in centrocytic lymphoma. Proc Natl Acad Sci USA 1991; 88: 9638–9642.
Raffeld M, Jaffe ES . bcl-1, t(11;14), and mantle cell-derived lymphomas. Blood 1991; 78: 259–263.
Lovec H, Grzeschiczek A, Kowalski MB, Moroy T . Cyclin D1/bcl-1 cooperates with myc genes in the generation of B-cell lymphoma in transgenic mice. EMBO J 1994; 13: 3487–3495.
Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, Rosenwald A et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature 2000; 403: 503–511.
Shipp MA, Ross KN, Tamayo P, Weng AP, Kutok JL, Aguiar RC et al. Diffuse large B-cell lymphoma outcome prediction by gene-expression profiling and supervised machine learning. Nat Med 2002; 8: 68–74.
Tamayo P, Slonim D, Mesirov J, Zhu Q, Kitareewan S, Dmitrovsky E et al. Interpreting patterns of gene expression with self-organizing maps: methods and application to hematopoietic differentiation. Proc Natl Acad Sci USA 1999; 96: 2907–2912.
Rosenwald A, Alizadeh AA, Widhopf G, Simon R, Davis RE, Yu X et al. Relation of gene expression phenotype to immunoglobulin mutation genotype in B cell chronic lymphocytic leukemia. J Exp Med 2001; 194: 1639–1647.
Hofmann WK, de Vos S, Tsukasaki K, Wachsman W, Pinkus GS, Said JW et al. Altered apoptosis pathways in mantle cell lymphoma detected by oligonucleotide microarray. Blood 2001; 98: 787–794.
Ek S, Hogerkorp CM, Dictor M, Ehinger M, Borrebaeck CA . Mantle cell lymphomas express a distinct genetic signature affecting lymphocyte trafficking and growth regulation as compared with subpopulations of normal human B cells. Cancer Res 2002; 62: 4398–4405.
Rosenwald A, Wright G, Wiestner A, Chan WC, Connors JM, Campo E et al. The proliferation gene expression signature is a quantitative integrator of oncogenic events that predicts survival in mantle cell lymphoma. Cancer Cell 2003; 3: 185–197.
Jadayel DM, Lukas J, Nacheva E, Bartkova J, Stranks G, De Schouwer PJ et al. Potential role for concurrent abnormalities of the cyclin D1, p16CDKN2 and p15CDKN2B genes in certain B cell non-Hodgkin's lymphomas. Functional studies in a cell line (Granta 519). Leukemia 1997; 11: 64–72.
Rimokh R, Berger F, Bastard C, Klein B, French M, Archimbaud E et al. Rearrangement of CCND1 (BCL1/PRAD1) 3′ untranslated region in mantle-cell lymphomas and t(11q13)-associated leukemias. Blood 1994; 83: 3689–3696.
Hsieh C, Brown S, Derleth C, Mackie K . Internalization and recycling of the CB1 cannabinoid receptor. J Neurochem 1999; 73: 493–501.
Schmidt EE, Ichimura K, Messerle KR, Goike HM, Collins VP . Infrequent methylation of CDKN2A(MTS1/p16) and rare mutation of both CDKN2a and CDKN2B(MTS2/p15) in primary astrocytic tumours. Br J Cancer 1997; 75: 2–8.
Stoica GE, Kuo A, Powers C, Bowden ET, Sale EB, Riegel AT et al. Midkine binds to anaplastic lymphoma kinase (ALK) and acts as a growth factor for different cell types. J Biol Chem 2002; 277: 35990–35998.
Kato H, Watanabe K, Murari M, Isogai C, Kinoshita T, Nagai H et al. Midkine expression in Reed-Sternberg cells of Hodgkin's disease. Leukemia Lymphoma 2000; 37: 415–424.
Dussault I, Giguere V . Differential regulation of the N-myc proto-oncogene by ROR alpha and RVR, two orphan members of the superfamily of nuclear hormone receptors. Mol Cell Biol 1997; 17: 1860–1867.
Delerive P, Monte D, Dubois G, Trottein F, Fruchart-Najib J, Mariani J et al. The orphan nuclear receptor ROR alpha is a negative regulator of the inflammatory response. EMBO Rep 2001; 2: 42–48.
Missbach M, Jagher B, Sigg I, Nayeri S, Carlberg C, Wiesenberg I . Thiazolidine diones, specific ligands of the nuclear receptor retinoid Z receptor/retinoid acid receptor-related orphan receptor alpha with potent antiarthritic activity. J Biol Chem 1996; 271: 13515–13522.
Galiegue S, Mary S, Marchand J, Dussossoy D, Carriere D, Carayon P et al. Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur J Biochem 1995; 232: 54–61.
Carayon P, Marchand J, Dussossoy D, Derocq JM, Jbilo O, Bord A et al. Modulation and functional involvement of CB2 peripheral cannabinoid receptors during B-cell differentiation. Blood 1998; 92: 3605–3615.
Howlett AC, Barth F, Bonner TI, Cabral G, Casellas P, Devane WA et al. International Union of Pharmacology. XXVII. Classification of Cannabinoid Receptors. Pharmacol Rev 2002; 54: 161–202.
Noe SN, Newton C, Widen R, Friedman H, Klein TW . Anti-CD40, anti-CD3, and IL-2 stimulation induce contrasting changes in CB1 mRNA expression in mouse splenocytes. J Neuroimmunol 2000; 110: 161–167.
Hollinger S, Hepler JR . Cellular regulation of RGS proteins: modulators and integrators of G protein signaling. Pharmacol Rev 2002; 54: 527–559.
Hur EM, Kim KT . G protein-coupled receptor signalling and cross-talk: achieving rapidity and specificity. Cell Signal 2002; 14: 397–405.
Johnson EN, Druey KM . Functional characterization of the G protein regulator RGS13. J Biol Chem 2002; 277: 16768–16774.
Shi GX, Harrison K, Wilson GL, Moratz C, Kehrl JH . RGS13 regulates germinal center B lymphocytes responsiveness to CXC chemokine ligand (CXCL)12 and CXCL13. J Immunol 2002; 169: 2507–2515.
Acknowledgements
This research was supported by the Swedish Cancer Society, the Swedish Medical Research Council, and the Alice and Knut Wallenberg Foundation. We thank Drs Ken Mackie, Department of Anaesthesiology, University of Washington, Seattle, WA, USA for generously providing antibodies to cannabinoid receptors and the AtT20 CB1-transfected cell line and Dr Christian Bastard, Molecular Biology Laboratory and EMI 9906-IRFMP, Centre Henri Becquerel, Rouen, France for providing the Rec 1 cell line. We are grateful to Dr Karin Dahlman-Wright and Hui Gao, Karolinska Institutet, Department of Biosciences for help and support to the users of the Affymetrix core facility and to Fiona Brew and Camilla Ejdestig, Affymetrix for the workshops on data mining. We thank Pia Lennartsson for skilful technical help.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Islam, T., Asplund, A., Lindvall, J. et al. High level of cannabinoid receptor 1, absence of regulator of G protein signalling 13 and differential expression of Cyclin D1 in mantle cell lymphoma. Leukemia 17, 1880–1890 (2003). https://doi.org/10.1038/sj.leu.2403057
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2403057
Keywords
This article is cited by
-
Function and regulation of RGS family members in solid tumours: a comprehensive review
Cell Communication and Signaling (2023)
-
Pathophysiological roles of myristoylated alanine-rich C-kinase substrate (MARCKS) in hematological malignancies
Biomarker Research (2021)
-
WIN55,212-2 induces cytoplasmic vacuolation in apoptosis-resistant MCL cells
Cell Death & Disease (2011)
-
Cannabinoids, endocannabinoids, and cancer
Cancer and Metastasis Reviews (2011)
-
High expression of 5-lipoxygenase in normal and malignant mantle zone B lymphocytes
BMC Immunology (2009)