Abstract
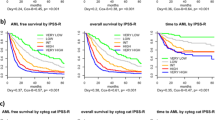
To ascertain the frequency of treatment-related acute myeloid leukemias and myelodysplastic syndromes (t-AML/t-MDS) in an unselected series, we have identified all adult cases analyzed in our department from 1976 to 1993. Further aims were to compare karyotypic features of t-AML/t-MDS with de novo AML/MDS, in our material as well as in 5098 unselected, cyto- genetically abnormal, published cases, and to analyze associations between type of prior therapy and karyotype. Among our 372 AML and 389 MDS, 47 (13%) were t-AML and 62 (16%) were t-MDS. Clonal abnormalities were significantly more common in t-AML and t-MDS than in de novo disease (68% vs 50%, P < 0.05 and 84% vs 45%, P < 0.001, respectively). Among the available 4230 AML and 1629 MDS (the present series and published cases), 14% were t-AML and 15% were t-MDS. In t-AML/t-MDS, the number of anomalies and the ploidy levels differed significantly from de novo cases, with complex and hypodiploid karyotypes being more common in t-AML/t-MDS. In t-AML, unbalanced changes in general, t(1;3), der(1;7), 3p−, −5, 5q−, −7, 7q−, t(9;11), t(11;19), t(11q23), der(12p), −17, der(17p), −18, and −21 were significantly more frequent than in de novo AML. In t-MDS, −5, −7, 7q−, 13q−, der(17p), and −18 were significantly more common. Type of prior treatment correlated significantly with number of anomalies in t-AML and with ploidy levels in t-AML/t-MDS. The frequencies of several aberrations varied with type of therapy, eg, 5q− was more frequent in radiotherapy-associated t-MDS, monosomy 7 was more common in t-AML and t-MDS after treatment with alkylators, and t(11q23) in t-AML was associated with topoisomerase II inhibitors. Abnormalities significantly more common in de novo disease were +8 as a sole anomaly, balanced changes in general, t(8;21), t(9;22), t(15;17), inv(16), and t(21q22) in AML, and −Y, 5q−, and 20q− as sole anomalies and +8 in MDS. The results emphasize the strong association between previous genotoxic exposure and karyotypic features.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Rutten FJ, Hustinx TWJ, Scheres JMJC, Wagener DJT . Trisomy-9 in the bone marrow of a patient with acute myelomonoblastic leukaemia Br J Haematol 1974 26: 391–394
Cavallin-Ståhl E, Landberg T, Ottow Z, Mitelman F . Hodgkin's disease and acute leukaemia. A clinical and cytogenetic study Scand J Haematol 1977 19: 273–280
Thirman MJ, Larson RA . Therapy-related myeloid leukemia Hematol Oncol Clin North Am 1996 10: 293–320
Pedersen-Bjergaard J, Rowley JD . The balanced and the unbalanced chromosome aberrations of acute myeloid leukemia may develop in different ways and may contribute differently to malignant transformation Blood 1994 83: 2780–2786
Rowley JD, Golomb HM, Vardiman J . Nonrandom chromosomal abnormalities in acute nonlymphocytic leukemia in patients treated for Hodgkin disease and non-Hodgkin lymphomas Blood 1977 50: 759–770
Sandberg AA, Abe S, Kowalczyk JR, Zedgenidze A, Takeuchi J, Kakati S . Chromosomes and causation of human cancer and leukemia. L. Cytogenetics of leukemias complicating other diseases Cancer Genet Cytogenet 1982 7: 95–136
Groupe Français de Cytogénétique Hématologique. Chromosome analysis of 63 cases of secondary nonlymphoid blood disorders: a cooperative study Cancer Genet Cytogenet 1984 12: 95–104
Le Beau MM, Albain KS, Larson RA, Vardiman JW, Davis EM, Blough RR, Golomb HM, Rowley JD . Clinical and cytogenetic correlations in 63 patients with therapy-related myelodysplastic syndromes and acute nonlymphocytic leukemia: further evidence for characteristic abnormalities of chromosomes no. 5 and 7 J Clin Oncol 1986 4: 325–345
Whang-Peng J, Young RC, Lee EC, Longo DL, Schechter GP, DeVita VT Jr . Cytogenetic studies in patients with secondary leukemia/dysmyelopoietic syndrome after different treatment modalities Blood 1988 71: 403–414
Pedersen-Bjergaard J, Philip P . Balanced translocations involving chromosome bands 11q23 and 21q22 are highly characteristic of myelodysplasia and leukemia following therapy with cytostatic agents targeting at DNA-topoisomerase II Blood 1991 78: 1147–1148
Pui C-H, Behm FG, Raimondi SC, Dodge RK, George SL, Rivera GK, Mirro J Jr, Kalwinsky DK, Dahl GV, Murphy SB, Crist WM, Williams DL . Secondary acute myeloid leukemia in children treated for acute lymphoid leukemia N Engl J Med 1989 321: 136–142
Gill Super HJ, McCabe NR, Thirman MJ, Larson RA, Le Beau MM, Pedersen-Bjergaard J, Philip P, Diaz MO, Rowley JD . Rearrangements of the MLL gene in therapy-related acute myeloid leukemia in patients previously treated with agents targeting DNA-topoisomerase II Blood 1993 82: 3705–3711
Sterkers Y, Preudhomme C, Laï J-L, Demory J-L, Caulier M-T, Wattel E, Bordessoule D, Bauters F, Fenaux P . Acute myeloid leukemia and myelodysplastic syndromes following essential thrombocythemia treated with hydroxyurea: high proportion of cases with 17p deletion Blood 1998 91: 616–622
Arnold JA, Ranson SA, Abdalla SH . Azathioprine-associated acute myeloid leukaemia with trilineage dysplasia and complex karyotype: a case report and review of the literature Clin Lab Haematol 1999 21: 289–292
Fourth International Workshop on Chromosomes in Leukemia. Secondary leukemias associated with neoplasia: treated and untreated Cancer Genet Cytogenet 1984 11: 319–321
Aul C, Gattermann N, Schneider W . Age-related incidence and other epidemiological aspects of myelodysplastic syndromes Br J Haematol 1992 82: 358–367
Kantarjian HM, Estey EH, Keating MJ . Treatment of therapy-related leukemia and myelodysplastic syndrome Hematol Oncol Clin North Am 1993 7: 81–107
Ruutu T, Almqvist A, Hallman H, Honkanen T, Järvenpää E, Järventie G, Koistinen P, Koivunen E, Lahtinen R, Lehtinen M, Nousiainen T-T, Pelliniemi A, Rajamäki A, Remes K, Sarkkinen R, Sinisalo M, Timonen T, Volin L, Elonen E . Oral induction and consolidation of acute myeloid leukemia with etoposide, 6-thioguanine, and idarubicin (ETI) in elderly patients: a randomized comparison with 5-day TAD Leukemia 1994 8: 11–15
Pedersen-Bjergaard J, Pedersen M, Roulston D, Philip P . Different genetic pathways in leukemogenesis for patients presenting with therapy-related myelodysplasia and therapy-related acute myeloid leukemia Blood 1995 86: 3542–3552
Park DJ, Koeffler HP . Therapy-related myelodysplastic syndromes Semin Hematol 1996 33: 256–273
Cripe LD . Adult acute leukemia Curr Probl Cancer 1997 21: 1–64
Hann IM, Stevens RF, Goldstone AH, Rees JK, Wheatley K, Gray RG, Burnett AK . Randomized comparison of DAT versus ADE as induction chemotherapy in children and younger adults with acute myeloid leukemia. Results of the Medical Research Council's 10th AML Trial (MRC AML10) Blood 1997 89: 2311–2318
Löwenberg B, Suciu S, Archimbaud E, Ossenkoppele G, Verhoef GEG, Vellenga E, Wijermans P, Berneman Z, Dekker AW, Stryckmans P, Schouten H, Jehn U, Muus P, Sonneveld P, Dardenne M, Zittoun R . Use of recombinant granulocyte–macrophage colony-stimulating factor during and after remission induction chemotherapy in patients aged 61 years and older with acute myeloid leukemia (AML): final report of AML-11, a phase III randomized study of the Leukemia Cooperative Group of European Organisation for the Research and Treatment of Cancer (EORTC-LCG) and the Dutch Belgian Hemato-Oncology Cooperative Group (HOVON) Blood 1997 90: 2952–2961
Löwenberg B, Suciu S, Archimbaud E, Haak H, Stryckmans P, de Cataldo R, Dekker AW, Berneman ZN, Thyss A, van der Lelie J, Sonneveld P, Visani G, Fillet G, Hayat M, Hagemeijer A, Solbu G, Zittoun R . Mitoxantrone versus daunorubicin in induction-consolidation chemotherapy – the value of low-dose cytarabine for maintenance of remission, and an assessment of prognostic factors in acute myeloid leukemia in the elderly: final report of the Leukemia Cooperative Group of the European Organization for the Research and Treatment of Cancer and the Dutch–Belgian Hemato–Oncology Cooperative Hovon Group. Randomized phase III study AML-9 J Clin Oncol 1998 16: 872–881
Archimbaud E, Charrin C, Magaud J-P, Campos L, Thomas X, Fière D, Rimokh R . Clinical and biological characteristics of adult de novo and secondary acute myeloid leukemia with balanced 11q23 chromosomal anomaly or MLL gene rearrangement compared to cases with unbalanced 11q23 anomaly: confirmation of the existence of different entities with 11q23 breakpoint Leukemia 1998 12: 25–33
Estey EH . Prognosis and therapy of secondary myelodysplastic syndromes Haematologica 1998 83: 543–549
Godwin JE, Kopecky KJ, Head DR, Willman CL, Leith CP, Hynes HE, Balcerzak SP, Appelbaum FR . A double-blind placebo-controlled trial of granulocyte colony-stimulating factor in elderly patients with previously untreated acute myeloid leukemia: a Southwest Oncology Group study (9031) Blood 1998 91: 3607–3615
Leone G, Mele L, Pulsoni A, Equitani F, Pagano L . The incidence of secondary leukemias Haematologica 1999 84: 937–945
Mauritzson N, Johansson B, Albin M, Billström R, Ahlgren T, Mikoczy Z, Nilsson PG, Hagmar L, Mitelman F . A single-center population-based consecutive series of 1500 cytogenetically investigated adult hematologic malignancies: karyotypic features in relation to morphology, age and gender Eur J Haematol 1999 62: 95–102
Mauritzson N, Johansson B, Albin M, Rylander L, Billström R, Ahlgren T, Mikoczy Z, Strömberg U, Mitelman F, Hagmar L, Nilsson PG . Survival time in a population-based consecutive series of adult acute myeloid leukemia – the prognostic impact of karyotype during the time period 1976-1993 Leukemia 2000 14: 1039–1043
Mauritzson N, Johansson B, Rylander L, Albin M, Strömberg U, Billström R, Ahlgren T, Mikoczy Z, Mitelman F, Hagmar L, Nilsson PG . The prognostic impact of karyotypic subgroups in myelo-dysplastic syndromes is strongly modified by sex Br J Haematol 2001 113: 347–356
Mitelman F, Johansson B, Mertens F (eds). Mitelman Data-base of Chromosome Aberrations in Cancer 2001 http://cgap.nci.nih.gov/Chromosomes/Mitelman
Coughlin SS, Benichou J, Weed DL . Attributable risk estimation in case–control studies Epidemiol Rev 1994 16: 51–64
Mitelman F, Manolova Y, Manolov G, Billström R, Heim S, Kristoffersson U, Mandahl N . High resolution analysis of the 5q− marker chromosome in refractory anemia Hereditas 1986 105: 49–54
Johansson B, Mertens F, Heim S, Kristoffersson U, Mitelman F . Cytogenetics of secondary myelodysplasia (sMDS) and acute nonlymphocytic leukemia (sANLL) Eur J Haematol 1991 47: 17–27
Mertens F, Johansson B, Heim S, Kristoffersson U, Mitelman F . Karyotypic patterns in chronic myeloproliferative disorders: report on 74 cases and review of the literature Leukemia 1991 5: 214–220
Billström R, Johansson H, Johansson B, Mitelman F . Immune-mediated complications in patients with myelodysplastic syndromes – clinical and cytogenetic features Eur J Haematol 1995 55: 42–48
Höglund M, Johansson B, Pedersen-Bjergaard J, Marynen P, Mitelman F . Molecular characterization of 12p abnormalities in hematologic malignancies: deletion of KIP1, rearrangement of TEL, and amplification of CCND2 Blood 1996 87: 324–330
Johansson B, Billström R, Kristoffersson U, Åkerman M, Garwicz S, Ahlgren T, Malm C, Mitelman F . Deletion of chromosome arm 3p in hematologic malignancies Leukemia 1997 11: 1207–1213
Andreasson P, Johansson B, Billström R, Garwicz S, Mitelman F, Höglund M . Fluorescence in situ hybridization analyses of hematologic malignancies reveal frequent cytogenetically unrecognized 12p rearrangements Leukemia 1998 12: 390–400
Secker-Walker LM, Moorman AV, Bain BJ, Mehta AB . Secondary acute leukemia and myelodysplastic syndrome with 11q23 abnormalities Leukemia 1998 12: 840–844
Gisselsson D, Höglund M, Mertens F, Johansson B, Dal Cin P, Van den Berghe H, Earnshaw WC, Mitelman F, Mandahl N . The structure and dynamics of ring chromosomes in human neoplastic and non-neoplastic cells Hum Genet 1999 104: 315–325
Johansson B, Billström R, Broberg K, Fioretos T, Nilsson P-G, Ahlgren T, Malm C, Samuelsson BO, Mitelman F . Cytogenetic polyclonality in hematologic malignancies Genes Chromosomes Cancer 1999 24: 222–229
Michels SD, McKenna RW, Arthur DC, Brunning RD . Therapy-related acute myeloid leukemia and myelodysplastic syndrome: a clinical and morphologic study of 65 cases Blood 1985 65: 1364–1372
Bloomfield CD . Chromosome abnormalities in secondary myelo-dysplastic syndromes Scand J Haematol 1986 36 (Suppl. 45): 82–90
Pedersen-Bjergaard J, Philip P . Cytogenetic characteristics of therapy-related acute nonlymphocytic leukaemia, preleukaemia and acute myeloproliferative syndrome: correlation with clinical data for 61 consecutive cases Br J Haematol 1987 66: 199–207
Iurlo A, Mecucci C, Van Orshoven A, Michaux JL, Boogaerts M, Noens L, Bosly A, Louwagie A, Van Den Berghe H . Cytogenetic and clinical investigations in 76 cases with therapy-related leukemia and myelodysplastic syndrome Cancer Genet Cytogenet 1989 43: 227–241
Pedersen-Bjergaard J, Philip P, Larsen SO, Jensen G, Byrsting K . Chromosome aberrations and prognostic factors in therapy-related myelodysplasia and acute nonlymphocytic leukemia Blood 1990 76: 1083–1091
Fenaux P, Laï JL, Quiquandon I, Preudhomme C, Dupriez B, Facon T, Lorthois C, Lucidarme D, Bauters F . Therapy related myelodysplastic syndrome and leukemia with no ‘unfavourable’ cyto-genetic findings have a good response to intensive chemotherapy: a report on 15 cases Leuk Lymphoma 1991 5: 117–125
Pedersen-Bjergaard J, Timshel S, Andersen MK, Andersen A-ST, Philip P . Cytogenetically unrelated clones in therapy-related mye-lodysplasia and acute myeloid leukemia: experience from the Copenhagen series updated to 180 consecutive cases Genes Chromosomes Cancer 1998 23: 337–349
Kantarjian HM, Keating MJ, Walters RS, Smith TL, Cork A, McCredie KB, Freireich EJ . Therapy-related leukemia and myelodysplastic syndrome: clinical, cytogenetic, and prognostic features J Clin Oncol 1986 4: 1748–1757
Berger R, Flandrin G . Chromosomal abnormalities in secondary acute myeloid leukaemia and the myelodysplastic syndromes In: Mufti GJ, Galton DAG (eds) The Myelodysplastic Syndromes Churchill Livingstone: London 1992 pp 129–139
Boice JD Jr, Blettner M, Kleinerman RA, Stovall M, Moloney WC, Engholm G, Austin DF, Bosch A, Cookfair DL, Krementz ET, Latourette HB, Peters LJ, Schulz MD, Lundell M, Pettersson F, Storm HH, Bell CMJ, Coleman MP, Fraser P, Palmer M, Prior P, Choi NW, Hislop TG, Koch M, Robb D, Robson D, Spengler RF, von Fournier D, Frischkorn R, Lochmüller H, Pompe-Kirn V, Rimpela A, Kjørstad K, Pejovic MH, Sigurdsson K, Pisani P, Kucera H, Hutchison GB . Radiation dose and leukemia risk in patients treated for cancer of the cervix J Natl Cancer Inst 1987 79: 1295–1311
Quesnel B, Kantarjian H, Pedersen Bjergaard J, Brault P, Estey E, Lai JL, Tilly H, Stoppa AM, Archimbaud E, Harousseau JL, Bauters F, Fenaux P . Therapy-related acute myeloid leukemia with t(8;21), inv(16), and t(8;16): a report on 25 cases and review of the literature J Clin Oncol 1993 11: 2370–2379
Curtis RE, Boice JD Jr, Stovall M, Bernstein L, Holowaty E, Karjalainen S, Langmark F, Nasca PC, Schwartz AG, Schymura MJ, Storm HH, Toogood P, Weyer P, Moloney WC . Relationship of leukemia risk to radiation dose following cancer of the uterine corpus J Natl Cancer Inst 1994 86: 1315–1324
Andersen MK, Johansson B, Larsen SO, Pedersen-Bjergaard J . Chromosomal abnormalities in secondary MDS and AML. Relationship to drugs and radiation with specific emphasis on the balanced rearrangements Haematologica 1998 83: 483–488
Van Limbergen H, Poppe B, Michaux L, Herens C, Brown J, Noens L, Berneman Z, De Bock R, De Paepe A, Speleman F . Identification of cytogenetic subclasses and recurring chromosomal aberrations in AML and MDS with complex karyotypes using M-FISH Genes Chromosomes Cancer 2002 33: 60–72
Mrozek K, Heinonen K, Theil KS, Bloomfield CD . Spectral karyotyping in patients with acute myeloid leukemia and a complex karyotype shows hidden aberrations, including recurrent over-representation of 21q, 11q, and 22q Genes Chromosomes Cancer 2002 34: 137–153
Paulsson K, Säll T, Fioretos T, Mitelman F, Johansson B . The incidence of trisomy 8 as a sole chromosomal aberration in myeloid malignancies varies in relation to gender, age, prior iatrogenic genotoxic exposure, and morphology Cancer Genet Cytogenet 2001 130: 160–165
Albin M, Björk J, Welinder H, Tinnerberg H, Mauritzson N, Johansson B, Billström R, Strömberg U, Mikoczy Z, Ahlgren T, Nilsson P-G, Mitelman F, Hagmar L . Acute myeloid leukemia and clonal chromosome aberrations in relation to past exposure to organic solvents Scand J Work Environ Health 2000 26: 482–491
Detourmignies L, Castaigne S, Stoppa AM, Harousseau JL, Sadoun A, Janvier M, Demory JL, Sanz M, Berger R, Bauters F, Chomienne C, Fenaux P . Therapy-related acute promyelocytic leukemia: a report on 16 cases J Clin Oncol 1992 10: 1430–1435
Kudo K, Yoshida H, Kiyoi H, Numata S, Horibe K, Naoe T . Etoposide-related acute promyelocytic leukemia Leukemia 1998 12: 1171–1175
Acknowledgements
This study was supported by grants from the Swedish Cancer Society, the Swedish Council for Work Life Research, PREEM Research Foundation, Georg Danielsson's Fund, Gunnar, Arvid and Elisabeth Nilsson's Foundation, and Lund University Hospital Funds
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mauritzson, N., Albin, M., Rylander, L. et al. Pooled analysis of clinical and cytogenetic features in treatment-related and de novo adult acute myeloid leukemia and myelodysplastic syndromes based on a consecutive series of 761 patients analyzed 1976–1993 and on 5098 unselected cases reported in the literature 1974–2001. Leukemia 16, 2366–2378 (2002). https://doi.org/10.1038/sj.leu.2402713
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2402713
Keywords
This article is cited by
-
Acute myeloid leukemia with rare recurring translocations—an overview of the entities included in the international consensus classification
Annals of Hematology (2024)
-
The complex karyotype in hematological malignancies: a comprehensive overview by the Francophone Group of Hematological Cytogenetics (GFCH)
Leukemia (2022)
-
Allogeneic Hematopoietic Stem Cell Transplantation in Therapy Related Acute Leukemia
Indian Journal of Hematology and Blood Transfusion (2021)
-
The leukemia strikes back: a review of pathogenesis and treatment of secondary AML
Annals of Hematology (2019)
-
Clinical Features and Outcomes of 666 Cases with Therapy-Related Myelodysplastic Syndrome (t-MDS)
Indian Journal of Hematology and Blood Transfusion (2018)