Abstract
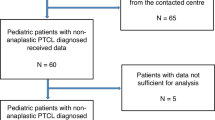
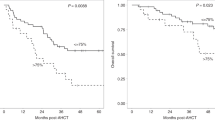
It was the aim of our study to examine the clinical significance of t(14;18)-positive cells in samples from 47 patients with follicular non-Hodgkin’s lymphoma (NHL) who underwent high-dose therapy with autologous peripheral blood stem cell (PBSC) transplantation. At the time of PBSC mobilization, 25 patients were in first remission, while 22 patients had a history of previous treatment failure. At the same time, 43 patients had polymerase chain reaction (PCR)-positive cells in samples from bone marrow (BM) and/or peripheral blood (PB). Independent of the remission status, high-dose cytarabine and mitoxantrone with granulocyte colony-stimulating factor (G-CSF) support were administered for PBSC mobilization. Following high-dose conditioning therapy which consisted of cyclophosphamide (200 mg/kg) and hyperfractionated total body irradiation (TBI, 14.4 Gy) or BEAM (carmustine, etoposide, cytarabine, melphalan), 34 patients received PCR-positive and 13 patients received PCR-negative autografts. After a median follow-up time of 20 months (range, 6–50) post-transplantation, 33 patients were in remission, while 14 patients had relapsed after a median time of 14.5 months (range, 10–42). Using the Andersen–Gill proportional hazards regression model for the analysis of relapse-free survival, we found that PCR-positive findings in samples from BM and/or PB at any given time-point after transplantation were associated with an increased estimated hazard ratio of 4.5 in comparison with a PCR-negative finding (P = 0.013). On the other hand, patients included while they were in first remission had a smaller estimated hazard ratio of 0.3 when compared with patients with a history of previous treatment failure (P = 0.048). For the latter group of patients, this translates into a significantly smaller probability of relapse-free survival in comparison to patients who were in first remission at the time of PBSC-mobilization (P = 0.012). In conclusion, the remission status of the patients before autografting and the PCR status as assessed on the occasion of follow-up examinations are significant prognostic parameters for relapse-free survival in patients with follicular lymphoma undergoing high-dose therapy with PBSC autografting.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Moos, M., Schulz, R., Martin, S. et al. The remission status before and the PCR status after high-dose therapy with peripheral blood stem cell support are prognostic factors for relapse-free survival in patients with follicular non-Hodgkin’s lymphoma. Leukemia 12, 1971–1976 (1998). https://doi.org/10.1038/sj.leu.2401242
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2401242
Keywords
This article is cited by
-
Rituximab purging and maintenance combined with auto-SCT: long-term molecular remissions and prolonged hypogammaglobulinemia in relapsed follicular lymphoma
Bone Marrow Transplantation (2009)
-
Commercial LightCycler®-based quantitative real-time PCR compared to nested PCR for monitoring of Bcl-2/IgH rearrangement in patients with follicular lymphoma
Annals of Hematology (2009)
-
Prolonged survival and low incidence of late toxic sequelae in advanced follicular lymphoma treated with a TBI-free autografting program: updated results of the multicenter consecutive GITMO trial
Leukemia (2006)
-
PCR detection of residual Bcl-2/IgH-positive cells after high-dose therapy with autologous stem cell transplantation is a prognostic factor for event-free survival in patients with low-grade follicular non-Hodgkin's lymphoma
Bone Marrow Transplantation (2003)
-
Positron emission tomography with [18F]2-fluoro-D-2-deoxyglucose (FDG-PET) predicts relapse of malignant lymphoma after high-dose therapy with stem cell transplantation
Leukemia (2002)