Abstract
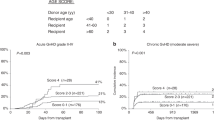
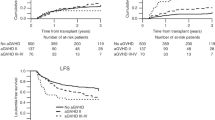
We investigated outcomes according to a new clinical grading system for chronic graft-versus-host disease (chronic GVHD) in 38 patients who developed chronic GVHD after an allogeneic hematopoietic stem cell transplantation. We categorized the patients into three grade groups, namely, grade I, grade II and grade III, according to the presence of three risk factors: extensive skin involvement, thrombocytopenia (TP) and progressive type of onset. Sixteen patients were classified into grade 1, 19 into grade II and three into grade III. The probability of withdrawal of systemic immunosuppression (IST) at 1, 2 and 3 years was 61, 76 and 87%, respectively. Patients with grades 2 or 3 chronic GVHD had prolonged duration of systemic IST compared to grade 1 (P=0.043). The probability of GVHD-specific survival (GSS) at 5 years was 52%. Twenty-two of 38 patients with chronic GVHD were still alive and the estimated 3-year overall survival (OS) rate was 60%, whereas that for the group with chronic GVHD grade I and grade II+III was 64 and 48% (P<0.05). Multivariate analysis showed that prior occurrence of acute GVHD, chronic GVHD grade, serum bilirubin over 1.5 mg/dl, date of diagnosis of chronic GVHD (<day 150 versus >day 150) and transplantation-risk factor were independent prognostic factors for GSS and OS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Atkinson K . Chronic graft-versus-host disease. Bone Marrow Transplant 1990; 5: 69–82.
Vogelsang GB . How I treat chronic graft-versus-host disease. Blood 2001; 97: 1196–1201.
Duell T, van Lint MT, Ljungman P, Tichelli A, Socie G, Apperley JF et al. Health and functional status of long-term survivors of bone marrow transplantation. EBMT Working Party on Late Effects and EULEP Study Group on Late Effects. European Group for Blood and Marrow Transplantation. Ann Intern Med 1997; 126: 184–192.
Socie G, Stone JV, Wingard JR, Weisdorf D, Henslee-Downey PJ, Bredeson C et al. Long-term survival and late deaths after allogeneic bone marrow transplantation. Late Effects Working Committee of the International Bone Marrow Transplant Registry. N Engl J Med 1999; 341: 14–21.
Sutherland HJ, Fyles GM, Adams G, Hao Y, Lipton JH, Minden MD et al. Quality of life following bone marrow transplantation: a comparison of patient reports with population norms. Bone Marrow Transplant 1997; 19: 1129–1136.
Akpek G, Zahurak ML, Piantadosi S, Margolis J, Doherty J, Davidson R et al. Development of a prognostic model for grading chronic graft-versus-host disease. Blood 2001; 97: 1219–1226.
Sullivan KM, Witherspoon RP, Storb R, Deeg HJ, Dahlberg S, Sanders JE et al. Alternating-day cyclosporine and prednisone for treatment of high-risk chronic graft-v-host disease. Blood 1988; 72: 555–561.
Wingard JR, Piantadosi S, Vogelsang GB, Farmer ER, Jabs DA, Levin LS et al. Predictors of death from chronic graft-versus-host disease after bone marrow transplantation. Blood 1989; 74: 1428–1435.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med 1980; 69: 204–217.
Arora M, Burns LJ, Davies SM, Macmillan ML, Defor TE, Miller WJ et al. Chronic graft-versus-host disease: a prospective cohort study. Biol Blood Marrow Transplant 2003; 9: 38–45.
Lee SJ, Klein JP, Barrett AJ, Ringden O, Antin JH, Cahn JY et al. Severity of chronic graft-versus-host disease: association with treatment-related mortality and relapse. Blood 2002; 100: 406–414.
Akpek G, Lee SJ, Flowers ME, Pavletic SZ, Arora M, Lee S et al. Performance of a new clinical grading system for chronic graft-versus-host disease: a multicenter study. Blood 2003; 102: 802–809.
Stewart BL, Storer B, Storek J, Deeg HJ, Storb R, Hansen JA et al. Duration of immunosuppressive treatment for chronic graft-versus-host disease. Blood 2004; 104: 3501–3506.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 1995; 15: 825–828.
Kondo M, Kojima S, Horibe K, Kato K, Matsuyama T . Risk factors for chronic graft-versus-host disease after allogeneic stem cell transplantation in children. Bone Marrow Transplant 2001; 27: 727–730.
Ochs LA, Miller WJ, Filipovich AH, Haake RJ, McGlave PB, Blazar BR et al. Predictive factors for chronic graft-versus-host disease after histocompatible sibling donor bone marrow transplantation. Bone Marrow Transplant 1994; 13: 455–460.
Randolph SS, Gooley TA, Warren EH, Appelbaum FR, Riddell SR . Female donors contribute to a selective graft-versus-leukemia effect in male recipients of HLA-matched, related hematopoietic stem cell transplants. Blood 2004; 103: 347–352.
Cutler C, Giri S, Jeyapalan S, Paniagua D, Viswanathan A, Antin JH . Acute and chronic graft-versus-host disease after allogeneic peripheral-blood stem-cell and bone marrow transplantation: a meta-analysis. J Clin Oncol 2001; 19: 3685–3691.
Flowers ME, Parker PM, Johnston LJ, Matos AV, Storer B, Bensinger WI et al. Comparison of chronic graft-versus-host disease after transplantation of peripheral blood stem cells versus bone marrow in allogeneic recipients: long-term follow-up of a randomized trial. Blood 2002; 100: 415–419.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, S., Jung, C., Lee, J. et al. New clinical grading system for chronic GVHD predicts duration of systemic immunosuppressive treatment and GVHD-specific and overall survival. Bone Marrow Transplant 39, 711–716 (2007). https://doi.org/10.1038/sj.bmt.1705661
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1705661
Keywords
This article is cited by
-
Selective activation and expansion of regulatory T cells using lipid encapsulated mRNA encoding a long-acting IL-2 mutein
Nature Communications (2022)
-
Clinical characteristics of chronic graft-versus-host disease following umbilical cord blood transplantation for adults
Bone Marrow Transplantation (2008)