Abstract
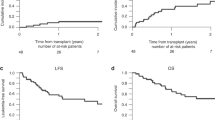
The major problems with busulfan/cyclophosphamide (Bu/Cy)-containing conditioning regimens are acute toxicities and graft failure. To decrease acute toxicities, we have prospectively evaluated a reduced intensity conditioning (RIC) regimen using targeted dosing of i.v. busulfan, fludarabine, and rabbit ATG (Bu/Flu/rATG) in children with diagnoses that historically would have been conditioned with Bu/Cy regimens. Nineteen pediatric patients were enrolled in the study. The donors included HLA-matched and one antigen-mismatched unrelated volunteers (n=11), unrelated cord blood (n=1), and related donors (n=7). Four patients developed graft failure, which occurred between 1 and 8.5 months post transplant. All four of them underwent a second transplantation and 3/4 are alive without evidence of disease. The mean follow-up of living patients is 29.5±s.d. 11 months. Despite excellent 2-year post-transplant overall survival (89±s.d.7%) and event-free survival (74±s.d.10%), the study was closed prematurely due to high graft failure rate (21%). Receiving a transplant from a mismatched unrelated donor was identified as a risk factor for graft failure. The Bu/Flu/rATG RIC regimen was very well tolerated, resulted in excellent overall survival, and provided sustained engraftment in patients undergoing transplant from matched sibling and unrelated donors. However, it did not provide sustained engraftment in the majority of children with nonmalignancies undergoing mismatched unrelated donor transplants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Walters MC, Patience M, Leisenring W, Eckman JR, Scott JJ, Mentzer WC et al. Bone marrow transplantation for sickle cell disease. N Engl J Med 1996; 335: 369–376.
Lucarelli G, Clift RA, Galimberti M, Angelucci E, Giardini C, Baronciani D et al. Bone marrow transplantation in adult thalassemic patients. Blood 1999; 93: 1164–1167.
Peters C, Steward CG, on behalf of the NMDP, IBMTR and the Working Party on Inborn Errors of the EBMT. Hematopoietic cell transplantation for inherited metabolic diseases: an overview of outcomes and practice guidelines. Bone Marrow Transplant 2003; 31: 229–239.
Antoine C, Muller S, Cant A, Cavazzana-Calvo M, Veyes P, Vossen J et al. Long-term survival and transplantation of hematopoietic stem cells for immunodeficiencies: report of the European experience 1968–1999. Lancet 2003; 361: 553–560.
Clift RA, Buckner CD, Thomas ED, Bensinger WI, Bowden R, Brayant E et al. Marrow transplantation for chronic myeloid leukemia: a randomized study comparing cyclophosphamide and total body irradiation with busulfan and cyclophosphamide. Blood 1994; 84: 2036–2043.
Locatelli F, Pession A, Bonetti F, Maserati E, Prete L, Pedrazzoli P et al. Busulfan, cyclophosphamide and melphalan as conditioning regimen for bone marrow transplantation in children with myelodyplastic syndromes. Leukemia 1994; 8: 844–849.
Grigg A, McLachlan R, Zaja J, Szer J . Reproductive status in long-term bone marrow transplant survivors receiving busulfan–cyclophosphamide (120 mg/kg). Bone Marrow Transplant 2000; 26: 1089–1095.
Ozkaynak MF, Weinberg K, Kohn D, Dender L, Parkman R, Lenarsky C . Hepatic veno-occlusive disease post-bone marrow transplantation in children conditioned with busulfan and cyclophosphamide: incidence, risk factors, and clinical outcome. Bone Marrow Transplant 1991; 7: 467–474.
Teinturier C, Hartmann O, Valteau-Couanet D, Benhamou E, Bougneres PF . Ovarian function after autologous bone marrow transplantation in childhood: high-dose busulfan is major cause of ovarian failure. Bone Marrow Transplant 1998; 22: 989–994.
Peters C, Balthazor M, Shapiro EG, King RJ, Kollman C, Hegland JD et al. Outcome of unrelated donor bone marrow transplantation in 40 children with Hurler syndrome. Blood 1996; 87: 4894–4902.
Bolinger AM, Zangwill AB, Slattery JT, Risler LJ, Sultan DH, Glidden DV et al. Target dose adjustment of busulfan in pediatric patients undergoing bone marrow transplantation. Bone Marrow Transplant 2001; 28: 1013–1018.
Kashyap A, Wingard J, Cagnoni P, Roy J, Tarantolo S, Hu W et al. Intravenous versus oral busulfan as part of busulfan/cyclophosphamide preparative regimen for allogneic hematopoietic stem cell transplantation: decreased incidence of hepatic venoocclusive disease (HVOD), HVOD-related mortalilty, and overall 100-day mortality. Biol Blood Marrow Transplant 2002; 8: 493–500.
Duval M, Pedron B, Rohrlich P, Legrand F, Faye A, Lescoeur B et al. Immune reconstitution after haematopoietic transplantation with two different doses of pre-graft antithymocyte globulin. Bone Marrow Transplant 2002; 30: 421–426.
Przepiorka D, Wiesdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transplant 1995; 15: 825–828.
Bearman S, Anderson G, Mori M, Hinds MS, Shulman MM, McDonald GB . Venoocclusive disease of the liver: development of a model for predicting fatal outcome after marrow transplantation. J Clin Oncol 1993; 11: 1729–1736.
Satwani P, Harrison L, Morris E, Del Toro G, Cairo MS . Reduced-intensity allogeneic stem cell transplantation in adults and children with malignant and nonmalignant disease: end of the beginning and future challenges. Biol Blood Marrow Transplant 2005; 11: 403–422.
Mothy M, Bay JO, Faucher C, Choufi B, Bilger K, Tournilhac O et al. Graft-versus-host disease following allogeneic transplantation from HLA-identical siblings with antithymocyte globulin-based reduced-intensity preparative regimen. Blood 2003; 102: 470–476.
Nagler A, Aker M, Or R, Naparstek E, Varadi G, Brautbar C et al. Low-intensity conditioning is sufficient to ensure engraftment in matched unrelated bone marrow transplantation. Exp Hematol 2001; 29: 362–370.
Shaughnessy PJ, Ornstein D, Ririe D, Callander NS, Anderson JE, Pollack MS et al. Phase II study of moderate-intensity preparative regimen with allogeneic peripheral blood stem cell transplantation for hematologic disease: the Texas Transplant Consortium experience. Biol Blood Marrow Transplant 2002; 8: 420–428.
Del Toro G, Satwani P, Harrison L, Cheung YK, Brigid Bradley M, George D et al. A pilot study of reduced intensity conditioning and allogeneic stem cell transplantation from unrelated cord blood and matched family donors in children and adolescent recipients. Bone Marrow Transplant 2004; 33: 613–622.
Jacobsohn DA, Duerst R, Tse W, Ketzel M . Reduced intensity hematopoietic stem-cell transplantation for treatment of non-malignant diseases in children. Lancet 2004; 364: 156–162.
Bornhauser M, Storer B, Slattery J, Appelbaum FR, Deeg HJ, Hansen J et al. Conditioning with fludarabine and targeted busulfan for transplantation of allogeneic hematopoietic stem cells. Blood 2003; 102: 820–826.
Perez-Simon JA, Diez-Campelo M, Martino R, Brunet S, Urbano A, Caballero D et al. Impact of CD34+ cell dose on the outcome of patients undergoing reduced-intensity-conditioning allogeneic peripheral blood stem cell transplantation. Blood 2003; 102: 1108–1113.
Valcarcel D, Martino R, Caballero D, Mateos MW, Perez-Simon JA, Canals C et al. Chimerism analysis following allogeneic peripheral blood stem cell transplantation with reduced-intensity conditioning. Bone Marrow Transplant 2003; 31: 387–392.
Duval M, Pedron B, Rohrlich P, Legrand F, Faye A, Lescoeur B et al. Immune reconstitution after hematopoietic transplantation with two different doses of pre-graft antithymocyte globulin. Bone Marrow Transplant 2002; 30: 421–426.
Shenoy S, Grossman WJ, DiPersio J, Yu LC, Wilson D, Barnes YJ et al. A novel reduced-intensity stem cell transplant regimen for nonmalignant disorders. Bone Marrow Transplant 2005; 35: 345–352.
Acknowledgements
Busulfan pharmacokinetic studies were carried out in the Pediatric Clinical Research Center, Moffitt Hospital, University of California San Francisco with funds provided by the National Center for Research Resources, 5 M01 RR-01271, US Public Health Service.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horn, B., Baxter-Lowe, LA., Englert, L. et al. Reduced intensity conditioning using intravenous busulfan, fludarabine and rabbit ATG for children with nonmalignant disorders and CML. Bone Marrow Transplant 37, 263–269 (2006). https://doi.org/10.1038/sj.bmt.1705240
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1705240
Keywords
This article is cited by
-
Allogeneic stem cell transplantation for X-linked agammaglobulinemia using reduced intensity conditioning as a model of the reconstitution of humoral immunity
Journal of Hematology & Oncology (2016)
-
New Directions for Rabbit Antithymocyte Globulin (Thymoglobulin®) in Solid Organ Transplants, Stem Cell Transplants and Autoimmunity
Drugs (2014)
-
A pilot study of reduced toxicity conditioning with BU, fludarabine and alemtuzumab before the allogeneic hematopoietic SCT in children and adolescents
Bone Marrow Transplantation (2011)
-
Treosulfan-based preparative regimens for allo-HSCT in childhood hematological malignancies: a retrospective study on behalf of the EBMT pediatric diseases working party
Bone Marrow Transplantation (2011)
-
Reduced-intensity conditioning in children: a reappraisal in 2008
Bone Marrow Transplantation (2008)