Summary:
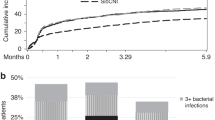
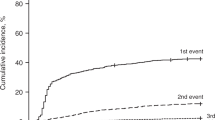
The safety and efficacy of early bacterial prophylaxis with piperacillin–tazobactam were prospectively evaluated in 51 autologous peripheral blood stem cell transplantation (PBSCT) recipients. The results were compared with those obtained in 51 control patients receiving oral fluoroquinolones in a retrospective matched-pair control study. Overall, 76% of the study group and 98% of the control group developed at least one febrile episode during neutropenia (P=0.002). Time from neutropenia to the first febrile episode (FFE) was significantly longer in the study group than in the control group (P=0.04). Once a febrile episode appeared, the duration of fever was significantly longer in cases than in controls (median of 5 and 2 days respectively, P<0.001), and led to a more frequent use of empirical amphotericin B (AmB), not statistically significant (P=0.13). However, the total time of antibiotic administration was significantly greater in the control than in the study group (P=0.05). The duration of AmB treatment shows a trend toward a longer duration in the control than in study group (P=0.2). Overall, 86% of the Gram-positive bacteremia and 85% of the Gram-negative bacteria were susceptible to the tested antibiotics. Our study suggests that a subgroup of patients could benefit from prophylaxis with piperacillin–tazobactam without increasing toxicity or bacterial resistance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Engels EA, Ellis CA, Supran SE et al. Early infection in bone marrow transplantation: quantitative study of clinical factors that affect risk. Clin Infect Dis 1999; 28: 256–266.
Kruger W, Russmann B, Kroger N et al. Early infections in patients undergoing bone marrow or blood stem cell transplantation – a 7 year single centre investigation of 409 cases. Bone Marrow Transplant 1999; 23: 589–597.
Barton T, Collis T, Stadtmauer E, Schuster M . Infectious complications the year after autologous bone marrow transplantation or peripheral stem cell transplantation for treatment of breast cancer. Clin Infect Dis 2001; 32: 391–395.
Saavedra S, Jarque I, Sanz GF et al. Infectious complications in patients undergoing unrelated donor bone marrow transplantation: experience from a single institution. Clin Microbiol Infect 2002; 8: 725–733.
Buzyn A, Tancrede C, Nitenberg G, Cordonnier C . Reflections on gut decontamination in hematology. Clin Microbiol Infect 1999; 5: 449–456.
Kerr KG . The prophylaxis of bacterial infections in neutropenic patients. J Antimicrobial Chemother 1999; 44: 587–591.
Sepkowitz KA . Antibiotic prophylaxis in patients receiving hematopoietic stem cell transplant. Bone Marrow Transplant 2002; 29: 367–371.
Cruciani M, Rampazzo R, Malena M et al. Prophylaxis with fluoroquinolones for bacterial infections in neutropenic patients: a meta-analysis. Clin Infect Dis 1996; 23: 795–805.
Horvathova Z, Spanik S, Sufliarsky J et al. Bacteremia due to methicillin-resistant staphylococci occurs more frequently in neutropenic patients who received antimicrobial prophylaxis and is associated with higher mortality in comparison to methicillin-sensitive bacteriemia. Int J Antimicrobial Agents 1998; 10: 55–58.
Elting LS, Bodey GP, Keefe BH . Septicemia and shock syndrome due to viridans streptococci: a case–control study of predisposing factors. Clin Infect Dis 1992; 14: 1201–1207.
Tunkel AR, Sepkowitz KA . Infections caused by viridans streptococci in patients with neutropenia. Clin Infect Dis 2002; 34: 1524–1529.
Yeh SP, Hsueh EJ, Yu MS et al. Oral ciprofloxacin as antibacterial prophylaxis after allogeneic bone marrow transplantation: a reappraisal. Bone Marrow Transplant 1999; 24: 1207–1211.
van Kraaij MG, Dekker AW, Peters E et al. Emergence and infectious complications of ciprofloxacin-resistant Escherichia coli in haematological cancer patients. Eur J Clin Microbiol Infect Dis 1998; 17: 591–592.
Oethinger M, Conrad S, Kaifel K et al. Molecular epidemiology of fluoroquinolone-resistant Escherichia coli bloodstream isolates from patients admitted to European cancer centers. Antimicrobial Agents Chemother 1996; 40: 387–392.
Baum HV, Franz U, Geiss HK . Prevalence of ciprofloxacin-resistant Escherichia coli in hematologic-oncologic patients. Infection 2000; 28: 278–281.
Avril M, Hartmann O, Valteau-Couanet D et al. Antiinfective prophylaxis with ceftazidime and teicoplanin in children undergoing high-dose chemotherapy and bone marrow transplantation. Pediatr Hematol Oncol 1994; 11: 63–73.
Kroschinsky F, Wichmann G, Bornhauser M et al. Efficacy and tolerability of prophylactic treatment with intravenous piperacillin/tazobactam in patients undergoing hematopoietic stem cell transplantation. Transpl Infect Dis 2002; 4: 132–136.
Meisenberg B, Gollard R, Brehm T et al. Prophylactic antibiotics eliminate bacteremia and allow safe outpatient management following high-dose chemotherapy and autologous stem cell rescue. Support Care Cancer 1996; 4: 364–369.
National Committee for Clinical Laboratory Standards (NCCLS). Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically, Approved Standard, 5th edn. Clinical and Laboratory Standards Institute: Wayne, PA, 2000 (http://www.nccls.org).
Bauernfeind A, Abele-Horn M, Emmerling P, Jungwirth R . Multiclonal emergence of ciprofloxacin-resistant clinical isolates of Escherichia coli and Klebsiella pneumoniae. J Antimicrobial Chemother 1994; 34: 1074–1076.
Sanders CC, Sanders Jr WE, Goering RV, Werner V . Selection of multiple antibiotic resistance by quinolones, beta-lactams, and aminoglycosides with special reference to cross-resistance between unrelated drug classes. Antimicrobial Agents Chemother 1984; 26: 797–801.
Hughes WT, Armstrong D, Bodey GP et al. 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 2002; 34: 730–751.
Karp JE, Dick JD, Angelopulos C et al. Empiric use of vancomycin during prolonged treatment-induced granulocytopenia. Randomized, double-blind, placebo-controlled clinical trial in patients with acute leukemia. Am J Med 1986; 81: 237–242.
Petersen F, Thornquist M, Buckner C et al. The effects of infection prevention regimens on early infectious complications in marrow transplant patients: a four arm randomized study. Infection 1988; 16: 199–208.
Jagannath S, Vesole DH, Zhang M et al. Feasibility and cost-effectiveness of outpatient autotransplants in multiple myeloma. Bone Marrow Transplant 1997; 20: 445–450.
Meisenberg BR, Ferran K, Hollenbach K et al. Reduced charges and costs associated with outpatient autologous stem cell transplantation. Bone Marrow Transplant 1998; 21: 927–932.
Chandrasekar PH, Abraham OC, Klein J et al. Low infectious morbidity after intensive chemotherapy and autologous peripheral blood progenitor cell transplantation in the outpatient setting for women with breast cancer. Clin Infect Dis 2001; 32: 546–551.
Rovira M . Outpatient management of autologous haematopoietic cell transplantation: the Barcelona experience. Presse Med 2004; 33: 479–481.
Sanz MA, Lopez J, Lahuerta JJ et al. Cefepime plus amikacin versus piperacillin–tazobactam plus amikacin for initial antibiotic therapy in haematology patients with febrile neutropenia: results of an open, randomized, multicentre trial. J Antimicrobial Chemother 2002; 50: 79–88.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Solano, C., Gutierrez, A., Martinez, F. et al. Prophylaxis of early bacterial infections after autologous peripheral blood stem cell transplantation (PBSCT): a matched-pair study comparing oral fluoroquinolones and intravenous piperacillin–tazobactam. Bone Marrow Transplant 36, 59–65 (2005). https://doi.org/10.1038/sj.bmt.1705005
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1705005
Keywords
This article is cited by
-
Low circulating mannan-binding lectin levels correlate with increased frequency and severity of febrile episodes in myeloma patients who undergo ASCT and do not receive antibiotic prophylaxis
Bone Marrow Transplantation (2017)
-
The role of prophylactic antimicrobials during autologous stem cell transplantation: a single-center experience
European Journal of Clinical Microbiology & Infectious Diseases (2012)
-
Clinical impact of cycling the administration of antibiotics for febrile neutropenia in Japanese patients with hematological malignancy
European Journal of Clinical Microbiology & Infectious Diseases (2012)
-
A randomized comparison of empiric or pre-emptive antibiotic therapy after hematopoietic stem cell transplantation
Bone Marrow Transplantation (2007)