Summary:
Allogeneic hematopoietic stem cell transplantation (allo-SCT) recipients are prone to infections. The incidences of mycobacterial infections after allo-SCT in several case series vary from less than 0.1–5.5%. However, no study has been published on tuberculosis following unrelated cord blood transplantation (UCBT). We retrospectively reviewed medical records of 113 adult patients with a median age of 54 years who underwent reduced-intensity UCBT (RI-UCBT) at Toranomon Hospital from March 2002 to May 2004. Mycobacterium tuberculosis infections were diagnosed in three patients (2.7%), of these two patients developed primary infection and one patient developed reactivation of latent tuberculosis. The interval between RI-UCBT and the diagnosis of tuberculosis was 34, 41 and 61 days. All the patients had disseminated disease at diagnosis. Histological examination showed the lack of granuloma in caseous necrosis. Combination antituberculous treatments showed limited efficacy, and two patients died immediately after diagnosis. M. tuberculosis caused life-threatening illness, rapidly progressing in RI-UCBT recipients. The lack of granuloma in caseous necrosis suggests the impaired T-cell function in early post transplant phase of RI-UCBT. We should consider M. tuberculosis in the differential diagnoses of fever of unknown source after RI-UCBT.
Similar content being viewed by others
Main
Unrelated cord blood transplantation (UCBT) is an attractive alternative for patients with hematologic malignancies who do not have a matched related or unrelated donor. Myeloablative UCBT for adult patients achieves engraftment in 90% of the cases and is associated with 15% of transplant-related mortality, mostly attributable to infection.1 The feasibility of UCBT using reduced-intensity regimens (RI-UCBT) for adult patients with hematologic diseases has been reported.2,3,4 Studies on immune recovery following UCBT suggested that RI-UCBT recipients may have reduced incidences of graft-versus-host disease (GVHD) and infectious complications.5 However, little information is available on infections following RI-UCBT as well as myeloablative UCBT.6,7,8
Mycobacterium tuberculosis (M. tuberculosis) is a common pathogen in the world. It is endemic to East Asia including Japan. Japan conducts a nationwide program of Bacillus Calmette-Guerin (BCG) vaccination in infants and revaccination in school children at the age of 6, 7, 13 and 14 years since 1951 and 1954, respectively. Annual incidence of tuberculosis decreased from 698 per 100 000 in 1951 to 31 per 100 000 in 2000. Tuberculosis mostly affects people at the age of 60 years or older; 82% of the patients are 40 years or older.9,10 Reactivation of latent tuberculosis is common in immunodeficient patients such as AIDS patients and organ transplant recipients.11,12 Recent studies on tuberculosis following allogeneic hematopoietic stem cell transplantation (allo-SCT) have demonstrated that this is a significant problem in endemic countries with an incidence of 0.1–5.5%.13,14,15,16,17,18,19,20,21
This is the first report, to our knowledge, on tuberculosis following RI-UCBT. Detailed description of this complication would be informative in the management of RI-UCBT.
Patients and methods
Data collection
Medical records of 113 recipients who underwent RI-UCBT between March 2002 and May 2004 at Toranomon Hospital were reviewed for the diagnosis of tuberculosis. Their characteristics were shown in Table 1. All the patients had received BCG vaccines according to the national vaccination program.10 No patients had undergone antituberculosis treatments prior to RI-UCBT.
The following data of the patients with tuberculosis were collected: demographics, past medical history including tuberculosis, the primary hematologic diseases, the presence of acute or chronic GVHD, chest radiographs, diagnostic methods and the primary site of M. tuberculosis infection, and the outcome of tuberculosis treatment.
Transplantation procedures and supportive care
The pretransplant evaluation of the respiratory system included chest radiographs, high-resolution computed tomographies (CT) and pulmonary function tests. Sputum smears and cultures for acid-fast bacilli were not routinely obtained.
A cord blood (CB) unit was searched through the Japan Cord Blood Bank Network. CB units, which were available for UCBT were 4/6 or more serologically HLA-antigen matched and contained at least 2 × 107 nucleated cells/kg of recipient body weight before freezing.
Transplantation procedures were shown in Table 1. The RI conditioning regimen consisted of fludarabine 25 mg/m2 on days −6 to −2, melphalan 40 mg/m2 on days −3 and −2, and total body irradiation (TBI) 4 Gy on day −1. Granulocyte colony-stimulating factor was administered from day 1 until neutrophil engraftment.
GVHD prophylaxis was either tacrolimus 0.03 mg/kg or cyclosporine 3 mg/kg in a continuous infusion starting on day −1. The diagnosis of GVHD was made based on clinical judgment and skin or gut biopsy results to support the clinical diagnosis. Acute GVHD was graded according to the consensus criteria.22 When patients developed grade II–IV acute GVHD, we initiated 1–2 mg/kg/day of methylprednisolone in addition to tacrolimus or cyclosporine.
Patients were managed in reverse isolation in laminar airflow-equipped rooms. All patients received prophylaxis with trimethoprim-sulfamethoxazole against Pneumocystis carinii infection. They received tosufloxacine 450 mg/day, fluconazole 200 mg/day and acyclovir 600 mg/day for the prophylaxis of bacterial, fungal and herpesvirus infection, respectively. Broad-spectrum antibiotics were initiated when neutropenic fever developed. All patients were monitored for cytomegalovirus pp65 antigenemia once a week. When the antigenemia turned positive, pre-emptive therapy with foscarnet was initiated as described previously.23
Definition of M. tuberculosis infection
A diagnosis of tuberculosis was based on the identification of M. tuberculosis on acid-fast bacilli stain of sputum, endotracheal aspirates, bone marrow aspirates or bronchoalveolar lavage (BAL), or the presence of caseous granulomas on hematoxylin–eosin staining of tissue specimens.24 All of the BAL specimens were subject to polymerase chain reactions (PCR) using M. tuberculosis-specific primers25 and COBAS AMPLICOR™ system (Roche Diagnostics KK, Tokyo, Japan).
Disease control for tuberculosis
All the staff members were screened for tuberculosis by chest X-ray annually. Anyone with positive chest X-ray and suggestive symptoms are not on service.
Any patients with suspected tuberculosis are placed in respiratory isolation until three consecutive sputum samples are negative for acid-fast bacilli. Patients with the diagnosis of tuberculosis receive the standard antituberculosis treatment with rifampicin, isoniazid and ethambutol, with or without pyrazinamide. Since rifampicin may decrease cyclosporine concentration, cyclosporine dose was adjusted by monitoring its blood levels.
Results
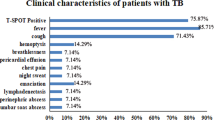
Three of the 113 RI-UCBT recipients (2.7%) developed tuberculosis. They had no different risk factors for tuberculosis compared with the other 110 patients. Their detailed clinical characteristics are shown in Table 2.
Patient 1
A 67-year-old man with chronic myeloid leukemia in blastic crisis underwent RI-UCBT in July 2003. He had no family history of tuberculosis. Screening chest CT before transplantation was normal. He developed a pre-engraftment immune reaction on day 9,3 which was successfully treated by methylprednisolone 0.25 mg/kg. He achieved neutrophil engraftment on day 19. He developed grade II acute GVHD on day 24, which responded to methylprednisolone. He developed a high-grade fever on day 61, and chest CT on day 62 revealed small nodules in bilateral lungs, which were 2 mm in diameter. The lesions were considered to be bacterial or fungal infection and we initiated empiric treatments. The fever persisted despite broad-spectrum antibiotics and antifungal agents. Follow-up CT on day 75 showed multiple cavities in bilateral lungs, which were 12 mm in diameter (Figure 1a). Ziehl–Neelsen stain and PCR of BAL specimens on day 77 were positive for M. tuberculosis. Subsequently, M. tuberculosis was cultured from BAL fluid and bone marrow aspirates. On day 61, white blood cell count was 7.3 × 109/l (neutrophil 91.0%) with 95 CD4+T-cells/μl; serum IgG was 306 mg/dl. Cyclosporine was tapered and a combination therapy with isoniazid, rifampicin, ethambutol and pyrazinamide was initiated. GVHD aggravated after tapering of cyclosporine, which was successfully treated with methylprednisolone 1 mg/kg. On day 89, he developed respiratory failure due to interstitial pneumonitis, requiring mechanical ventilation. He died of multiple-organ failure on day 116. In the post-mortem examination, almost all organs showed necrosis without granulation (Figure 2a). Ziehl–Neelsen stain identified acid-fast bacilli in the necrosis.
Chest CT scans. (a) Patient 1: follow-up CT on day 75 showed multiple cavities in bilateral lungs, which were 12 mm in diameter. (b) Patient 2: chest CT on day 34 showed infiltration in the right lower lobe, thickening of bronchial wall and pericardial effusion. (c) Patient 3: enlarged mediastinal lymph nodes.
Pathologic features of tuberculosis infection. (a) Caseous necrosis without granulation in the lung. Paraffin section with hematoxylin–eosin stain; original magnification × 100. (b) Acid-fast bacilli (arrowhead) in caseous necrosis in the liver. Paraffin section with Ziehl–Neelsen stain; original magnification × 400.
Patient 2
A 64-year-old woman with refractory acute myeloid leukemia underwent RI-UCBT in August 2003. She had no history of tuberculosis. Screening chest CT showed a small calcification nodule in the right lower lobe, which was 10 mm in diameter. She developed a pre-engraftment immune reaction on day 9,3 which was successfully controlled by methylprednisolone 0.25 mg/kg. She achieved neutrophil engraftment on day 23. The clinical course had been uneventful until day 34, when a high-grade fever developed. Chest CT on day 34 showed infiltration in the right lower lobe, thickening of bronchial wall and pericardial effusion (Figure 1b). The patient refused bronchoscopy at this point. The fever persisted despite broad-spectrum antibiotics and antifungal drugs. BAL specimens obtained on day 43 were positive for M. tuberculosis on PCR. The calcified nodule in the right lobe indicated reactivation of latent tuberculosis. Phenotype of the peripheral lymphocytes on day 43 was shown in Table 2. Combination therapy with isoniazid, rifampicin and ethambutol was immediately initiated. However, it was discontinued due to hepatic toxicity. She died of adult respiratory distress syndrome on day 57. In the post-mortem examination, almost all organs had necrosis without granulation, and Ziehl–Neelsen stain revealed acid-fast bacilli in the necrotic lesions (Figure 2b). She also had disseminated cytomegalovirus infection.
Patient 3
A 20-year-old woman with acute myeloid leukemia in second remission underwent RI-UCBT in November 2003. Screening chest CT was normal. She achieved neutrophil engraftment on day 28. The clinical course had been uneventful until she developed a high-grade fever on day 46. She had not developed either a pre-engraftment fever or acute GVHD.3 Chest CT showed mediastinal lymphadenopathy, which was 15 mm in diameter (Figure 1c). The fever did not respond to empiric broad-spectrum antibiotics. Bone marrow aspirates on day 65 were positive for M. tuberculosis on PCR and culture. She subsequently developed cutaneous tuberculosis (Figure 3) with disseminated intravascular coagulation. She was diagnosed with primary infection of M. tuberculosis. On day 46, white blood cell count and serum levels of IgG were 5.6 × 109/l (neutrophil 84.5%) and 1180 mg/dl, respectively. Phenotype of the peripheral lymphocytes on day 46 was shown in Table 2. After initiation of isoniazid, rifampicin and ethambutol, these symptoms improved gradually. She is alive without reactivation of tuberculosis on day 180.
Discussion
Japan has been an endemic country of tuberculosis. Among the newly diagnosed patients in 2001, 57.1% were at the age of 60 years and above and 17.5% were in their 20's and 30's. Many patients above 50 have a history of tuberculosis. Even without obvious history of tuberculosis, latent infection after unknown exposure is common in the generation. Therefore, Patients 1 and 2 were considered to have reactivation of latent tuberculosis. Transmission from them to Patient 3 was unlikely because Patient 3 was admitted to the hospital 20 and 25 days after patients 1 and 2 had died, respectively. No patients had tuberculosis during her hospitalization. Owing to her young age, her tuberculosis was considered a primary infection rather than reactivation of latent infection.
The incidence of tuberculosis following RI-UCBT is 2.5% in our hospital, and the median age was 54 years in this study. A high incidence of tuberculosis might be expected in RI-UCBT patients due to patients' age and prolonged immunosuppression associated with the use of CB as a stem cell source; however, the incidence of tuberculosis following RI-UCBT was comparable to that following allo-HSCT in previous reports from endemic countries.15,18,19,20,21 Tuberculosis is less frequent in RI-UCBT recipients than in the immunodeficient patients of different etiologies such as solid organ transplantation and AIDS. Immunosuppression after RI-UCBT is transient,11 while AIDS patients and solid organ transplant recipients have a life-long immunosuppression. Alternatively, the frequent and prolonged use of several antibiotics may suppress reactivation of M. tuberculosis. Fluoroquinolones are active against M. tuberculosis, and are occasionally used as antituberculous prophylaxis.16
Clinical features of tuberculosis following RI-UCBT might be different from those following conventional allo-HSCT.13,14,15,16,17,18,19,20,21 Tuberculosis following conventional allo-HSCT usually occurs several months after transplantation; the median time to presentation with tuberculosis was 324 days post transplant.18 It usually follows indolent clinical courses. The lung is the most common site of the disease, and the common manifestations are fever and cough. If treated adequately, most patients are cured without relapse. The clinical courses of our patients were different from those in the previous reports.13,14,15,16,17,18,19,20,21 Tuberculosis developed within 100 days of RI-UCBT, either reactivation or primary infection, and disseminated rapidly to various organs. It should be noted that all the three patients developed miliary tuberculosis, and two of the three patients were refractory to antituberculosis therapy and finally died. Such a rapid extrapulmonary progression of tuberculosis has been reported in solid organ recipients or AIDS patients.26,27
Although limited data are available on immune reconstitution of RI-UCBT recipients, it is clear their cellular immunity is extremely impaired (Table 3). While recovery of the immune system depends on peripheral expansion of mature T- and B-lymphocytes transferred with the graft,28 CB does not contain antigen-experienced cells, leading to a slow immune reconstitution and an increased risk of infectious complications. Functional immune recovery begins 3 months after conventional UCBT in adult patients, and T-cell reconstitution begins by 18 months.29 Chronic GVHD, immunosuppressive therapy, TBI and T-cell depletion have been shown to be risk factors for tuberculosis following conventional allo-HSCT.16,17,30 We used a TBI-containing preparative regimen, and two patients developed either GVHD or pre-engraftment immune reaction, requiring corticosteroid. Prolonged immunosuppression results in failure to acquire adoptive immunity against tuberculosis, and TBI hampers normal function of alveolar macrophages. Both might have contributed to an increased susceptibility to early-onset tuberculosis.
This study demonstrates that tuberculosis is a significant complication of RI-UCBT. There is a considerable delay from the onset of symptoms to the diagnosis of tuberculosis. Unless we have enough information on the complication, it is difficult to make an early diagnosis and to initiate an antituberculous treatment. A delay in establishing a diagnosis of tuberculosis in RI-UCBT recipients could have a pivotal impact on their survival. While needs for antituberculous prophylaxis are controversial in solid organ and marrow transplantation,31 identification of high-risk patients and prophylaxis in the subgroup may be beneficial in RI-UCBT. We suggest screening before RI-UCBT with PPD skin test in addition to chest CT, especially in the endemic areas. Further studies are warranted to investigate clinical features of tuberculosis following RI-UCBT, and to identify its optimal management.
References
Goggins TF, Rizzieri DR . Nonmyeloablative allogeneic stem cell transplantation using alternative donors. Cancer Control 2004; 11: 86–96.
Rizzieri DA, Long GD, Vredenburgh JJ et al. Successful allogeneic engraftment of mismatched unrelated cord blood following a nonmyeloablative preparative regimen. Blood 2001; 98: 3486–3488.
Miyakoshi S, Yuji K, Kami M et al. Successful engraftment after reduced-intensity umbilical cord blood transplantation for adult patients with advanced hematological diseases. Clin Cancer Res 2004; 10: 3586–3592.
Barker JN, Weisdorf DJ, DeFor TE et al. Rapid and complete donor chimerism in adult recipients of unrelated donor umbilical cord blood transplantation after reduced-intensity conditioning. Blood 2003; 102: 1915–1919.
Rocha V, Wagner Jr JE, Sobocinski KA et al. Graft-versus-host disease in children who have received a cord-blood or bone marrow transplant from an HLA-identical sibling. Eurocord and International Bone Marrow Transplant Registry Working Committee on Alternative Donor and Stem Cell Sources. N Engl J Med 2000; 342: 1846–1854.
Saavedra S, Sanz GF, Jarque I et al. Early infections in adult patients undergoing unrelated donor cord blood transplantation. Bone Marrow Transplant 2002; 30: 937–943.
Tomonari A, Iseki T, Ooi J et al. Cytomegalovirus infection following unrelated cord blood transplantation for adult patients: a single institute experience in Japan. Br J Haematol 2003; 121: 304–311.
Tomonari A, Iseki T, Takahashi S et al. Varicella zoster virus infection in adult patients after unrelated cord blood transplantation: a single institute experience in Japan. Br J Haematol 2003; 122: 802–805.
Ohmori M, Ishikawa N, Yoshiyama T et al. Current epidemiological trend of tuberculosis in Japan. Int J Tuberc Lung Dis 2002; 6: 415–423.
Mori T . Current tuberculosis problem in Japan and its control. Intern Med 2002; 41: 56–57.
Aguado JM, Herrero JA, Gavalda J et al. Clinical presentation and outcome of tuberculosis in kidney, liver, and heart transplant recipients in Spain. Spanish Transplantation Infection Study Group, GESITRA. Transplantation 1997; 63: 1278–1286.
Selwyn PA, Hartel D, Lewis VA et al. A prospective study of the risk of tuberculosis among intravenous drug users with human immunodeficiency virus infection. N Engl J Med 1989; 320: 545–550.
Navari RM, Sullivan KM, Springmeyer SC et al. Mycobacterial infections in marrow transplant patients. Transplantation 1983; 36: 509–513.
Kurzrock R, Zander A, Vellekoop L et al. Mycobacterial pulmonary infections after allogeneic bone marrow transplantation. Am J Med 1984; 77: 35–40.
Ip MS, Yuen KY, Chiu EK et al. Pulmonary infections in bone marrow transplantation: the Hong Kong experience. Respiration 1995; 62: 80–83.
Ip MS, Yuen KY, Woo PC et al. Risk factors for pulmonary tuberculosis in bone marrow transplant recipients. Am J Respir Crit Care Med 1998; 158: 1173–1177.
Martino R, Martinez C, Brunet S et al. Tuberculosis in bone marrow transplant recipients: report of two cases and review of the literature. Bone Marrow Transplant 1996; 18: 809–812.
de la Camara R, Martino R, Granados E et al. Tuberculosis after hematopoietic stem cell transplantation: incidence, clinical characteristics and outcome. Spanish Group on Infectious Complications in Hematopoietic Transplantation. Bone Marrow Transplant 2000; 26: 291–298.
George B, Mathews V, Srivastava V et al. Tuberculosis among allogeneic bone marrow transplant recipients in India. Bone Marrow Transplant 2001; 27: 973–975.
Roy V, Weisdorf D . Mycobacterial infections following bone marrow transplantation: a 20 year retrospective review. Bone Marrow Transplant 1997; 19: 467–470.
Ku SC, Tang JL, Hsueh PR et al. Pulmonary tuberculosis in allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2001; 27: 1293–1297.
Przepiorka D, Weisdorf D, Martin P et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 1995; 15: 825–828.
Reusser P, Einsele H, Lee J et al. Randomized multicenter trial of foscarnet vs ganciclovir for preemptive therapy of cytomegalovirus infection after allogeneic stem cell transplantation. Blood 2002; 99: 1159–1164.
Rieder HL, Watson JM, Raviglione MC et al. Surveillance of tuberculosis in Europe. Working Group of the World Health Organization (WHO) and the European Region of the International Union Against Tuberculosis and Lung Disease (IUATLD) for uniform reporting on tuberculosis cases. Eur Respir J 1996; 9 (5): 1097–1104.
Tevere VJ, Hewitt PL, Dare A et al. Detection of Mycobacterium tuberculosis by PCR amplification with pan-Mycobacterium primers and hybridization to an M. tuberculosis-specific probe. J Clin Microbiol 1996; 34: 918–923.
Barnes PF, Bloch AB, Davidson PT, Snider Jr DE . Tuberculosis in patients with human immunodeficiency virus infection. N Engl J Med 1991; 324: 1644–1650.
Delaney V, Sumrani N, Hong JH, Sommer B . Mycobacterial infections in renal allograft recipients. Transplant Proc 1993; 25: 2288–2289.
Parkman R, Weinberg KI . Immunological reconstitution following bone marrow transplantation. Immunol Rev 1997; 157: 73–78.
Klein AK, Patel DD, Gooding ME et al. T-cell recovery in adults and children following umbilical cord blood transplantation. Biol Blood Marrow Transplant 2001; 7: 454–466.
Atkinson K . Reconstruction of the haemopoietic and immune systems after marrow transplantation. Bone Marrow Transplant 1990; 5: 209–226.
Singh N, Wagener MM, Gayowski T . Safety and efficacy of isoniazid chemoprophylaxis administered during liver transplant candidacy for the prevention of posttransplant tuberculosis. Transplantation 2002; 74: 892–895.
Acknowledgements
This study was supported by a Grant-in-Aid for Scientific Research from the Ministry of Health, Labor and Welfare.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Maeda, T., Kusumi, E., Kami, M. et al. Disseminated tuberculosis following reduced-intensity cord blood transplantation for adult patients with hematological diseases. Bone Marrow Transplant 35, 91–97 (2005). https://doi.org/10.1038/sj.bmt.1704740
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704740
Keywords
This article is cited by
-
A unique case of tuberculosis dissemination presenting as cutaneous lesions in a post allogeneic stem cell transplant patient
Bone Marrow Transplantation (2016)
-
Tuberculosis in umbilical cord blood transplant recipients: clinical characteristics and challenges
Bone Marrow Transplantation (2015)
-
Mycobacterium tuberculosis infection: a rare late complication after cord blood hematopoietic SCT
Bone Marrow Transplantation (2009)
-
Sequential adenovirus infection of type 14 hemorrhagic cystitis and type 35 generalized infection after cord blood transplantation
International Journal of Hematology (2009)
-
Molluscum contagiosum infection after reduced-intensity cord blood transplantation
Bone Marrow Transplantation (2006)