Summary:
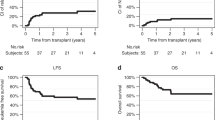
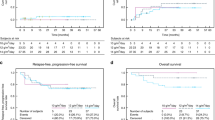
The purpose of this evaluation was to investigate the efficacy of high-dose chemotherapy with thiotepa, melphalan, and carboplatin (TMCb), and of autologous peripheral blood stem cell (PBSC) infusion in patients with aggressive non-Hodgkin's lymphoma (NHL) or Hodgkin's disease (HD). A total of 42 patients, 23 with intermediate-grade NHL and 19 with HD, received thiotepa (500 mg/m2), melphalan (100 mg/m2), and carboplatin (1050–1350 mg/m2) followed by autologous PBSC infusion. Of 21 patients with more advanced disease, four had primary refractory disease, one was in complete remission (CR)-2, 11 were in first refractory relapse, and five were beyond first relapse. Of 21 patients with less advanced disease, two were in CR-1, four were in CR-2, and 15 were in first responding relapse. In all, 14 patients (33%) had received prior radiotherapy prohibiting a total-body irradiation (TBI)-based conditioning regimen. The projected 2-year probabilities of survival, event-free survival (EFS), and relapse for all patients were 0.65, 0.60, and 0.21 (0.85, 0.80, and 0.10 for patients with less advanced disease and 0.47, 0.42, and 0.33 for patients with more advanced disease). The probability of nonrelapse mortality in the first 100 days was 0.12. Grade 3–4 regimen-related toxicities (RRT) occured in five of 42 (12%) patients and death due to grade-4 RRT occured in only one (2.5%) patient. These preliminary data suggest that 0.42% EFS in this study for advanced disease patients is highly encouraging and high-dose TMCb followed by autologous PBSC transplantation is well tolerated as well as an effective regimen in patients with intermediate-grade NHL or HD, and may be comparable to some previously used regimens including TBI-based regimens.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Sarosy G, Leyland-Jones B, Soochan P et al. The systemic administration of intravenous melphalan. J Clin Oncol 1988; 6: 1768–1782.
Wright JC, Golomb FM, Gumport SL et al. Summary of results with triethylenethiophosphoramide. Ann NY Acad Sci 1958; 68: 937–966.
Schiffman K, Buckner CD, Maziarz R et al. High-dose busulfan, melphalan, and thiotepa followed by autologous peripheral blood stem cell transplantation in patients with aggressive lymphoma or relapsed Hodgkin's disease. Biol Blood Marrow Transplant 1997; 3: 261–266.
Shea TC, Flaherty M, Elias A et al. A phase I clinical and pharmacokinetic study of carboplatin and autologous bone marrow support. J Clin Oncol 1989; 7: 651–655.
Demirer T, Ilhan O, Mandel NM et al. A phase I dose escalation study of high-dose thiotepa, melphalan and carboplatin (TMCb) followed by autologous peripheral blood stem cell transplantation (PBSCT) in patients with solid tumors and hematologic malignancies. Bone Marrow Transplant 2000; 25: 697–703.
Demirer T, Uysal VA, Ayli M et al. High-dose thiotepa, melphalan, and carboplatin (TMCb) followed by autologous stem cell transplantation in patients with advanced breast cancer – a retrospective evaluation. Bone Marrow Transplant 2003; 31: 755–761.
Hill R . The Non-Hodgkin's Lymphoma Pathologic Classification Project: National Cancer Instıtute sponsored study of classifications of non-Hodgkin's lymphomas: summary and description of a working formulation for clinical usage. Cancer 1982; 49: 2112–2117.
Lukes RJ, Butler JJ . The pathology and nomenclature of Hodgkin's disease. Cancer Res 1966; 26: 1063–1070.
Weaver CH, Petersen FB, Appelbaum FR et al. High-dose fractionated total-body irradiation, etoposide, and cyclophosphamide followed by autologous stem cell support in patients with malignant lymphoma. J Clin Oncol 1994; 12: 2559–2566.
Bearman SI, Appelbaum FR, Buckner CD et al. Regimen related toxicity in patients undergoing bone marrow transplantation. J Clin Oncol 1988; 6: 1562–1568.
Shubart MC, McDonald GB . Gastrointestinal and hepatic complications. In: Forman SJ, Blume KG, Thomas ED (eds). Bone Marrow Transplantation. Blackwell Scientific Publications: Massachusetts, USA, 1994; pp 454–459.
Crawford SW . Critical care and respiratory failure. In: Forman SJ, Blume KG, Thomas ED (eds). Bone Marrow Transplantation. Blackwell Scientific Publications: Massachusetts, USA, 1994; pp 513–517.
Demirer T, Aylı M, Ozcan M et al. Mobilization of peripheral blood stem cells with chemotherapy and recombinant human granulocyte-colony stimulating factor (Rh-GSCF): a randomized evaluation of different doses of Rh-GSCF. Br J Haematol 2002; 116: 468–472.
Demirer T, Aylı M, Daglı M et al. Influence of post-transplant recombinant human granulocyte-colony stimulating factor administration on peritransplant morbidity in patients undergoing autologous stem cell transplantation. Br J Haematol 2002; 118: 1104–1111.
Demirer T, lhan O, Aylı M et al. Monitoring of peripheral blood CD34+ cell counts on the first day of apheresis is highly predictive for efficient CD34+ cell yield. Therap Apheresis 2002; 6: 384–389.
Rowley SD, Bensinger WI, Gooley T et al. Effect of cell concentration on bone marrow and peripheral blood stem cell cryopreservation. Blood 1994; 83: 2731–2736.
Demirer T, Dagl M, Ilhan O et al. A randomized trial of assessment of efficacy of leukapheresis volumes, 8 l vs 12 l. Bone Marrow Transplant 2002; 29: 893–897.
Bensinger W, Appelbaum F, Rowley S et al. Factors that influence collection and engraftment of autologous peripheral blood stem cells. J Clin Oncol 1995; 13: 2547–2555.
Gorin NC . Stem cell processing and transplantation. The present models of acute leukemias and non-hodgkin's lymphomas in adults. Turkish J Hematol 1996; 14: 15–21.
Press OW, Livingston R, Mortimer J et al. Treatment of relapsed non-Hodgkin's lymphomas with dexamethasone, high-dose cytarabine, and cisplatin before marrow transplantation. J Clin Oncol 1991; 9: 423–432.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Appelbaum FR, Sullivan KM, Buckner CD et al. Treatment of malignant lymphoma in 100 patients with chemotherapy, total-body irradiation, and marrow transplantation. J Clin Oncol 1987; 5: 1340–1347.
Petersen FB, Appelbaum FR, Bigelow CL et al. High-dose cytosine arabinoside, total-body irradiation and marrow transplantation for advanced malignant lymphoma. Bone Marrow transplant 1989; 4: 483–488.
Gutierrez-Delgado F, Holmberg L, Hooper H et al. Autologous stem cell transplantation for Hodgkin's disease: busulfan, melphalan, and thiotepa compared to a radiation-based regimen. Bone Marrow Transplant 2003; 32: 279–285.
Weaver CH, Appelbaum FR, Petersen FB et al. High-dose cyclophosphamide, carmustine and etoposide followed by autologous bone marrow transplantation in patients with lymphoid malignancies who have received dose-limiting radiation therapy. J Clin Oncol 1993; 11: 1329–1335.
Gulati S, Yahalom J, Acaba K et al. Treatment of patients with relapsed and resistant non-Hodgkin's lymphoma using total-body irradiation, etoposide, and cyclophosphamide and autologous bone marrow transplantation. J Clin Oncol 1992; 10: 936–941.
Srivastava A, Bradstock KF, Szer J et al. Busulfan and melphalan prior to autologous bone marrow transplantation. Bone Marrow Transplant 1993; 12: 323–329.
Goldstone AH, McMillan AK, Chopra R et al. High-dose therapy for the treatment of non-Hodgkin's lymphoma. In: Armitage JO, Antman KH (eds). High-Dose Cancer Therapy; Pharmacology, Hematopoietins, Stem Cells. Williams & Wilkins: Baltimore, MD, 1992; pp 662–676.
Crump M, Smith AM, Brandwein J et al. High-dose etoposide and melphalan, and autologous bone marrow transplantation for patients with advanced Hodgkin's disease: Importance of disease status at transplant. J Clin Oncol 1993; 11: 711–740.
Wheeler C, Antin JH, Churchill M et al. Cyclophosphamide, carmustine, and etoposide with autologous bone marrow transplantation in refractory Hodgkin's disease and non-Hodgkin's lymphoma: a dose-finding study. J Clin Oncol 1990; 8: 648–654.
Horning SJ, Negrin RS, Chao NJ et al. High-dose etoposide regimens and autologous bone marrow transplantation (ABMT) for malignant lymphoma: results in 202 consecutive patients. Proc ASCO (abstract) 1993; 12: 382.
Stockerl-Goldstein KE, Horning SF, Negrin RS et al. Influence of preparatory regimen and source of hematopoietic cells on outcome of autotransplantation for non-Hodgkin's lymphoma. Biol Blood Marrow Transplant 1996; 2: 76–81.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Demirer, T., Ayli, M., Fen, T. et al. High-dose thiotepa, melphalan and carboplatin (TMCb) followed by autologous peripheral blood stem cell transplantation in patients with lymphoma – a retrospective evaluation. Bone Marrow Transplant 34, 781–786 (2004). https://doi.org/10.1038/sj.bmt.1704672
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704672
Keywords
This article is cited by
-
Long-term outcomes after thiotepa-based high-dose therapy (HDT) and autologous hematopoietic cell transplantation (auto-HCT) in non-Hodgkin lymphoma (NHL)
Bone Marrow Transplantation (2017)
-
Thiotepa-based high-dose therapy for autologous stem cell transplantation in lymphoma: a retrospective study from the EBMT
Bone Marrow Transplantation (2016)