Summary:
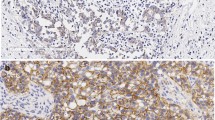
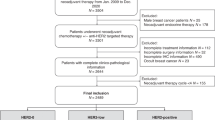
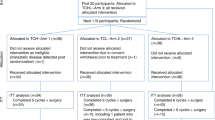
We retrospectively evaluated the predictive and prognostic role of HER2 expression in 44 metastatic breast cancer (MBC) patients treated with high-dose consolidation chemotherapy (HDCT) and autologous stem cell support after induction chemotherapy (IC) with six courses of epirubicin+paclitaxel (22 patients) or gemcitabine+epirubicin+paclitaxel (22 patients). HER2 expression was evaluated by an immunohistochemical method (Herceptest, Dako). A total of 13 patients (29.5%) showed a HER2 overexpression (score 3+). After IC, nine patients were in complete response (CR), 30 in partial response (PR), and five in stable disease (SD); after HDCT, 20 (45.5%) obtained a CR, and 23 were in PR, for a conversion rate of 48.5%. Conversion rate for HER2-positive patients was 87.5 vs 37% for HER2-negative patients (P=0.018). The median progression-free (PFS) and overall survivals (OS) were 17.6 (95% CI 13.2–22.0) and 44 (95% CI 25.9–62.3) months, respectively. Patients with HER2 overexpression experienced a significantly (P=0.0042) shorter median PFS (15.3 months, 95% CI 11.1–19.5) compared to HER2-negative patients (21.3 months, 95% CI 14.3–28.4). The median OS was 27.6 months (95% CI 4.5–50.7) in HER2-positive patients and 50.3 months (95% CI 38.7–62.0) in HER2-negative patients (P=0.345). These results indicate that HER2 overexpression predicts a worse outcome for patients with MBC treated with HDCT, despite the high CR rate obtained in this subset of patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Akiyama T, Sudo C, Ogawara H et al. The product of the human c-erbB-2 gene: a 185-kilodalton glycoprotein with tyrosine kinase activity. Science 1986; 232: 1644–1646.
Stern DF, Heffernan PA, Weinberg RA . p185, a product of the neu proto-oncogene, is a receptor like protein associated with tyrosine kinase activity. Mol Cell Biol 1986; 6: 1729–1740.
Slamon DJ, Clark GM, Wong SG et al. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987; 235: 177–182.
Ross JS, Fletcher JA . The HER/2neu oncogene: prognostic factor, predictive factor, and target for therapy. Semin Cancer Biol 1999; 9: 125–138.
Borg A, Baldetorp B, Ferno M et al. ERBB2 amplification is associated with tamoxifen resistance in steroid-receptor positive breast cancer. Cancer Lett 1994; 81: 137–144.
Berns EM, Foekens JA, van Staveren IL et al. Oncogene amplification and prognosis in breast cancer: relationship with systemic treatment. Gene 1995; 159: 11–18.
Carlomagno C, Perrone F, Gallo C et al. c-erb B2 over-expression decreases the benefit of adjuvant tamoxifen in early-stage breast cancer without axillary lymph node metastases. J Clin Oncol 1996; 14: 2702–2708.
Yamauchi H, O'Neill A, Gelman R et al. Prediction of response to antiestrogen therapy in advanced breast cancer patients by pretreatment circulating levels of extracellular domain of the HER-2/c-neu protein. J Clin Oncol 1997; 15: 2518–2525.
Jukkola A, Bloigu R, Soini Y et al. c-erbB-2 positivity is a factor for poor prognosis in breast cancer and poor response to hormonal or chemotherapy treatment in advanced disease. Eur J Cancer 2001; 37: 347–354.
De Placido S, De Laurentiis M, Carlomagno C et al. Twenty-year results of the Naples GUN randomized trial: predictive factors of adjuvant tamoxifen efficacy in early breast cancer. Clin Cancer Res 2003; 9: 1039–1046.
Paik S, Bryant J, Park C et al. erbB-2 protein and response to doxorubicin in patients with axillary lymph node-positive, hormone receptor-negative breast cancer. J Natl Cancer Inst 1998; 90: 1361–1370.
Baselga J, Seidman AD, Rosen PP, Norton L . Her-2 over-expression and paclitaxel sensitivity in breast cancer: therapeutic implications. Oncology (Huntington) 1997; 11: 43–48.
Gianni L, Capri G, Mezzelani A et al. Her-2/neu (HER2) amplification and response to doxorubicin/paclitaxel (AT) in women with metastatic breast cancer. Proc Am Soc Clin Oncol 1997; 15: 139a (abstr. 491).
Hamilton A, Larsimont D, Paridaens R et al. A study of the value of p53, HER2, and Bcl-2 in the prediction of response to doxorubicin and paclitaxel as single agents in metastatic breast cancer: a companion study to EORTC 10923. Clin Breast Cancer 2000; 1: 233–240.
Sparano JA . Taxanes for breast cancer: an evidence-based review of randomized phase II and phase III trials. Clin Breast Cancer 2000; 1: 32–40; discussion 41–42.
Yu D . Mechanisms of ErbB2-mediated paclitaxel resistance and trastuzumab-mediated paclitaxel sensitization in ErbB2-overexpressing breast cancers. Semin Oncol 2001; 28 (suppl. 16): 12–17.
Hortobagyi GN . High-dose chemotherapy for primary breast cancer: facts vs anecdotes. J Clin Oncol 1999; 17 (supplement): 25–29.
Bewick M, Chadderton T, Conlon M et al. Expression of C-erbB-2/HER-2 in patients with metastatic breast cancer undergoing high-dose chemotherapy and autologous blood stem cell support. Bone Marrow Transplant 1999; 24: 377–384.
Bewick M, Conlon M, Gerard S et al. HER-2 expression is a prognostic factor in patients with metastatic breast cancer treated with a combination of high-dose cyclophosphamide, mitoxantrone, paclitaxel and autologous blood stem cell support. Bone Marrow Transplant 2001; 27: 847–853.
Kim YS, Konoplev SN, Montemurro F et al. HER-2/neu overexpression as a poor prognostic factor for patients with metastatic breast cancer undergoing high-dose chemotherapy with autologous stem cell transplantation. Clin Cancer Res 2001; 7: 4008–4012.
Nieto Y, Nawaz S, Jones RB et al. Prognostic model for relapse after high-dose chemotherapy with autologous stem-cell transplantation for stage IV oligometastatic breast cancer. J Clin Oncol 2002; 20: 707–718.
Harris LN, Liotcheva V, Broadwater G et al. Comparison of methods of measuring HER-2 in metastatic breast cancer patients treated with high-dose chemotherapy. J Clin Oncol 2001; 19: 1698–1706.
Bengala C, Pazzagli I, Tibaldi C et al. Mobilization, collection, and characterization of peripheral blood hemopoietic progenitors after chemotherapy with epirubicin, paclitaxel, and granulocyte-colony stimulating factor administered to patients with metastatic breast carcinoma. Cancer 1998; 82: 867–873.
Bengala C, Pazzagli I, Innocenti F et al. High-dose thiotepa and melphalan with hemopoietic progenitor support following induction therapy with epirubicin-paclitaxel-containing regimens in metastatic breast cancer (MBC). Ann Oncol 2001; 12: 69–74.
Bengala C, Danesi R, Guarneri V et al. High-dose consolidation chemotherapy with idarubicin and alkylating agents following induction with gemcitabine–epirubicin–paclitaxel in metastatic breast cancer: a dose finding study. Bone Marrow Transplant 2003; 31: 275–280.
Oken MM, Creech RH, Tormey DC et al. Toxicity and response criteria of the Eastern cooperative oncology group. Am J Clin Oncol 1982; 5: 649–655.
Kaplan EL, Meier P . Nonparametric estimation for incomplete observation. J Am Stat Assoc 1958; 53: 457–481.
Cox DR . Regression models and life-tables. J R Stat Soc B 1972; 34: 187–220.
Stadtmauer EA, O'Neill A, Goldstein LJ et al. Conventional-dose chemotherapy compared with high-dose chemotherapy plus autologous hematopoietic stem-cell transplantation for metastatic breast cancer. Philadelphia Bone Marrow Transplant Group. N Engl J Med 2000; 342: 1069–1076.
Schmid P, Samonigg H, Nitsch T et al. Randomized trial of up front tandem high-dose chemotherapy (HD) compared to standard chemotherapy with doxorubicin and paclitaxel (AT) in metastatic breast cancer (MBC). Proc Am Soc Clin Oncol 2002; 21: 171 (abstract).
Crown J, Perey L, Lind M et al. Superiority of tandem high-dose chemotherapy (HDC) vs optimized conventionally-dosed chemotherapy (CDC) in patients (patients) with metastatic breast cancer (MBC): The International Randomized Breast Cancer Dose Intensity Study (IBDIS 1). Proc Am Soc Clin Oncol 2003; 22: 23 (abstr. 88).
Roche H, Viens P, Biron P et al. High-dose chemotherapy for breast cancer: the French PEGASE experience. Cancer Control 2003; 10: 42–47.
Rodenhuis S, Bontenbal M, Beex LV et al. Netherlands working party on autologous transplantation in solid tumors: high-dose chemotherapy with hematopoietic stem-cell rescue for high-risk breast cancer. N Engl J Med 2003; 349: 7–16.
Slamon DJ, Leyland-Jones B, Shak S et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 2001; 344: 783–792.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guarneri, V., Bengala, C., Orlandini, C. et al. HER2 overexpression as a prognostic factor in metastatic breast cancer patients treated with high-dose chemotherapy and autologous stem cell support. Bone Marrow Transplant 34, 413–417 (2004). https://doi.org/10.1038/sj.bmt.1704619
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704619
Keywords
This article is cited by
-
Prognostic factors for survival in metastatic breast cancer by hormone receptor status
Breast Cancer Research and Treatment (2014)
-
Cardiac toxicity of trastuzumab in metastatic breast cancer patients previously treated with high-dose chemotherapy: a retrospective study
British Journal of Cancer (2006)