Abstract
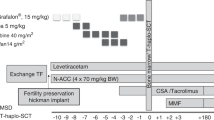
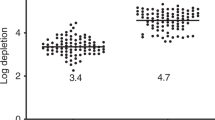
We evaluated the outcome of two modes of T cell depletion for HLA-identical sibling stem cell transplants in 34 consecutive adult patients: group A (n = 11) received PBSC post CliniMACs immuno-magnetic enrichment of CD34+ cells and group B (n = 23) received bone marrow following in vitro incubation with CAMPATH-1M and complement. All patients received an identical conditioning regimen which consisted of in vivoCAMPATH-1H 20 mg over 5 days, thiotepa 10 mg/kg, cyclophosphamide 120 mg/kg and 14.4 Gy TBI. No additional graft-versus-host disease prophylaxis was given. The mean T cell dose administered was 0.02 ± 0.05 × 106/kg for group A and 2.8 ± 2.8 106/kg for group B (P < 0.001). With a median follow-up of 28 months overall survival was 36.4% for group A at 12 months compared to 78.3% for group B (P = 0.001). Transplant-related mortality in group A at 12 months was 63.6% as compared to 18.0% in group B (P = 0.003). Most of the procedure-related deaths in group A occurred secondary to infection. These results suggest that extensive in vitro T cell depletion of peripheral blood stem cells in combination with in vivo T cell depletion may have profound effects upon the incidence of infections following allogeneic stem cell transplantation and this may adversely effect transplant-related mortality. Bone Marrow Transplantation (2001) 28, 827–834.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Waldmann H, Polliak A, Hale G et al. Elimination of graft-versus-host disease by in vitro depletion of alloreactivelymphocytes with a monoclonal rat anti-human lymphocyte antibody (CAMPATH-1) Lancet 1984 2: 483–6
Wagner JE, Donnenberg AD, Noga SJ et al. Lymphocyte depletion of donor bone marrow by counterflow centrifugal elutriation: results of a phase I clinical trial Blood 1988 72: 1168–1176
Marmont AM, Horowitz MM, Gale RP et al. T cell depletion of HLA-identical transplants in leukemia Blood 1991 78: 2120–2130
Young JW, Papadopoulos EB, Cunningham I et al. T-cell-depleted allogeneic bone marrow transplantation in adults with acute nonlymphocytic leukemia in first remission Blood 1992 79: 3380–3387
Soiffer RJ, Fairclough D, Robertson M et al. CD6-depleted allogeneic bone marrow transplantation for acute leukemia in first complete remission Blood 1997 89: 3039–3047
Urbano-Ispizua A, Rozman C, Martinez C et al. Rapid engraftment without significant graft-versus-host disease after allogeneic transplantation of CD34+ selected cells from peripheral blood Blood 1997 89: 3967–3973
Cornetta K, Gharpure V, Mills B et al. Rapid engraftment after allogeneic transplantation using CD34-enriched marrow cells Bone Marrow Transplant 1998 21: 65–71
Kernan NA, Bordignon C, Heller G et al. Graft failure after T-cell-depleted human leukocyte antigen identical marrow transplants for leukemia: I. Analysis of risk factors and results of secondary transplants Blood 1989 74: 2227–2236
Apperley JF, Jones L, Hale G et al. Bone marrow transplantation for patients with chronic myeloid leukaemia: T cell depletion with Campath-1 reduces the incidence of graft-versus-host disease but may increase the risk of leukaemic relapse Bone Marrow Transplant 1986 1: 53–66
Schattenberg A, De Witte T, Preijers F et al. Allogeneic bone marrow transplantation for leukemia with marrow grafts depleted of lymphocytes by counterflow centrifugation Blood 1990 75: 1356–1363
Verdonck LF, de Gast GC, van Heugten HG, Dekker AW . A fixed low number of T cells in HLA-identical allogeneic bone marrow transplantation Blood 1990 75: 776–780
Aversa F, Tabilio A, Terenzi A et al. Successful engraftment of T-cell-depleted haploidentical ‘three-loci’ incompatible transplants in leukemia patients by addition of recombinant human granulocyte colony-stimulating factor-mobilized peripheral blood progenitor cells to bone marrow inoculum Blood 1994 84: 3948–3955
Mavroudis D, Barrett J . The graft-versus-leukemia effect Curr Opin Hematol 1996 3: 423–429
Heitger A, Neu N, Kern H et al. Essential role of the thymus to reconstitute naive (CD45RA+) T-helper cells after human allogeneic bone marrow transplantation Blood 1997 90: 850–857
Small TN, Papadopoulos EB, Boulad F et al. Comparison of immune reconstitution after unrelated and related T-cell-depleted bone marrow transplantation: effect of patient age and donor leukocyte infusions Blood 1999 93: 467–480
Verfuerth S, Peggs K, Vyas P et al. Longitudinal monitoring of immune reconstitution by CDR3 size spectratyping after T-cell-depleted allogeneic bone marrow transplant and the effect of donor lymphocyte infusions on T-cell repertoire Blood 2000 95: 3990–3995
Roux E, Helg C, Dumont-Girard F et al. Analysis of T-cell repopulation after allogeneic bone marrow transplantation: significant differences between recipients of T-cell depleted and unmanipulated grafts Blood 1996 87: 3984–3992
Dumont-Girard F, Roux E, van Lier RA et al. Reconstitution of the T-cell compartment after bone marrow transplantation: restoration of the repertoire by thymic emigrants Blood 1998 92: 4464–4471
Godthelp BC, van Tol MJ, Vossen JM, van Den Elsen PJ . T-cell immune reconstitution in pediatric leukemia patients after allogeneic bone marrow transplantation with T-cell-depleted or unmanipulated grafts: evaluation of overall and antigen-specific T-cell repertoires Blood 1999 94: 4358–4369
Hertenstein B, Hampl W, Bunjes D et al. In vivo/ex vivo T cell depletion for GVHD prophylaxis influences onset and course of active cytomegalovirus infection and disease after BMT Bone Marrow Transplant 1995 15: 387–393
Broers AE, van Der Holt R, van Esser JW et al. Increased transplant-related morbidity and mortality in CMV-seropositive patients despite highly effective prevention of CMV disease after allogeneic T-cell-depleted stem cell transplantation Blood 2000 95: 2240–2245
Hale G, Xia MQ, Tighe HP et al. The CAMPATH-1 antigen (CDw52) Tissue Antigens 1990 35: 118–127
Schumm M, Lang P, Taylor G et al. Isolation of highly purified autologous and allogeneic peripheral CD34+ cells using the CliniMACS device J Hematother 1999 8: 209–218
Peggs KS, Ings SJ, Kottaridis PD et al. Cytomegalovirus infection and disease after autologous CD34-selected peripheral blood stem cell transplantation for multiple myeloma: no evidence of increased incidence based on polymerase-chain-reaction monitoring Blood 2000 96: 369–370
Atkinson K, Horowitz MM, Gale RP et al. Consensus among bone marrow transplanters for diagnosis, grading and treatment of chronic graft-versus-host disease. Committee of the International Bone Marrow Transplant Registry Bone Marrow Transplant 1989 4: 247–254
Przepiorka D, Weisdorf D, Martin P et al. 1994 Consensus Conference on Acute GVHD Grading Bone Marrow Transplant 1995 15: 825–828
Clarke E, Potter MN, Hale G et al. Double T cell depletion of bone marrow using sequential positive and negative cell immunoaffinity or CD34+ cell selection followed by Campath-1M; effect on CD34+ cells and progenitor cell recoveries Bone Marrow Transplant 1998 22: 117–124
Arpinati M, Green CL, Heimfeld S et al. Granulocyte-colony stimulating factor mobilizes T helper 2-inducing dendritic cells Blood 2000 95: 2484–2490
Clarke E, Potter MN, Oakhill A et al. A laboratory comparison of T cell depletion by CD34+ cell immunoaffinity selection and in vitro Campath-1M treatment: clinical implications for bone marrow transplantation and donor leukocyte therapy Bone Marrow Transplant 1997 20: 599–605
Bacigalupo A, Mordini N, Pitto A et al. Transplantation of HLA-mismatched CD34+ selected cells in patients with advanced malignancies: severe immunodeficiency and related complications Br J Haematol 1997 98: 760–766
Champlin RE, Passweg JR, Zhang MJ et al. T-cell depletion of bone marrow transplants for leukemia from donors other than HLA-identical siblings: advantage of T-cell antibodies with narrow specificities Blood 2000 95: 3996–4003
Champlin RE, Schmitz N, Horowitz MM et al. Blood stem cells compared with bone marrow as a source of hematopoietic cells for allogeneic transplantation. IBMTR Histocompatibility and Stem Cell Sources Working Committee and the European Group for Blood and Marrow Transplantation (EBMT) Blood 2000 95: 3702–3709
Bensinger WI, Martin PJ, Storer B et al. Transplantation of bone marrow as compared with peripheral-blood cells from HLA-identical relatives in patients with hematologic cancers New Engl J Med 2001 344: 175–181
Lowdell MW, Craston R, Ray N et al. The effect of T cell depletion with Campath-1M on immune reconstitution after chemotherapy and allogeneic bone marrow transplant as treatment for leukaemia Bone Marrow Transplant 1998 21: 679–686
Behringer D, Bertz H, Schmoor C et al. Quantitative lymphocyte subset reconstitution after allogeneic hematopoietic transplantation from matched related donors with CD34+ selected PBPC grafts unselected PBPC grafts or BM grafts Bone Marrow Transplant 1999 24: 295–302
Martinez C, Urbano-Ispizua A, Rozman C et al. Immune reconstitution following allogeneic peripheral blood progenitor cell transplantation: comparison of recipients of positive CD34+ selected grafts with recipients of unmanipulated grafts Exp Hematol 1999 27: 561–568
Davison GM, Novitzky N, Kline A et al. Immune reconstitution after allogeneic bone marrow transplantation depleted of T cells Transplantation 2000 69: 1341–1347
Hale G, Zhang MJ, Bunjes D et al. Improving the outcome of bone marrow transplantation by using CD52 monoclonal antibodies to prevent graft-versus-host disease and graft rejection Blood 1998 92: 4581–4590
Labadie J, van Tol MJ, Dijkstra NH et al. Transfer of specific immunity from donor to recipient of an allogeneic bone marrow graft: effect of conditioning on the specific immune response of the graft recipient Br J Haematol 1992 80: 381–390
Storek J, Witherspoon RP, Storb R . T cell reconstitution after bone marrow transplantation into adult patients does not resemble T cell development in early life Bone Marrow Transplant 1995 16: 413–425
Douek DC, Vescio RA, Betts MR et al. Assessment of thymic output in adults after haematopoietic stem-cell transplantation and prediction of T-cell reconstitution (see comments) Lancet 2000 355: 1875–1881
Hale G, Jacobs P, Wood L et al. CD52 antibodies for prevention of graft-versus-host disease and graft rejection following transplantation of allogeneic peripheral blood stem cells Bone Marrow Transplant 2000 26: 69–76
Acknowledgements
We would like to thank Nikki McKaeg, Judith Stuart and Brenda Miller for help in the collection and analysis of data. We would also like to thank Professor Paul Moss and Dr Charlie Craddock for their helpful criticisms regarding the manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Chakraverty, R., Robinson, S., Peggs, K. et al. Excessive T cell depletion of peripheral blood stem cells has an adverse effect upon outcome following allogeneic stem cell transplantation. Bone Marrow Transplant 28, 827–834 (2001). https://doi.org/10.1038/sj.bmt.1703248
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1703248
Keywords
This article is cited by
-
HIF-1α inhibitor echinomycin reduces acute graft-versus-host disease and preserves graft-versus-leukemia effect
Journal of Translational Medicine (2017)
-
Haploidentical related-donor hematopoietic cell transplantation in children using megadoses of CliniMACs-selected CD34+ cells and a fixed CD3+ dose
Bone Marrow Transplantation (2013)
-
The humanized anti-HLA-DR moAb, IMMU-114, depletes APCs and reduces alloreactive T cells: implications for preventing GVHD
Bone Marrow Transplantation (2012)
-
Alemtuzumab markedly reduces chronic GVHD without affecting overall survival in reduced-intensity conditioning sibling allo-SCT for adults with AML
Bone Marrow Transplantation (2009)
-
Influence of cytomegalovirus (CMV) sero-positivity on CMV infection, lymphocyte recovery and non-CMV infections following T-cell-depleted allogeneic stem cell transplantation: a comparison between two T-cell depletion regimens
Bone Marrow Transplantation (2004)