Abstract
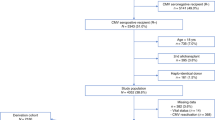
Potential risk factors for CMV infection and the use of quantitative CMV PCR screening to guide pre-emptive anti-CMV therapy were reviewed retrospectively in 32 allogeneic bone marrow transplant patients accrued over a 2-year period. Significant CMV PCR positivity (an indicator of CMV infection) developed in 34% of patients. When analysed by recipient CMV IgG serostatus, 69% of seropositive recipients developed significant CMV PCR positivity while none of the seronegative recipients did so (P = 0.00007). Considering only the seropositive recipients, 100% of those who received the low intensity campath-1H/fludarabine/melphalan ‘mini-allograft’ conditioning regimen developed significant CMV PCR positivity, while only 44% of those who had received cyclophosphamide/TBI did so (P = 0.0337). The mean time to first episode of significant CMV PCR positivity for those who had received campath/fludarabine/ melphalan was 25 days while for those who had received cyclophosphamide/TBI, this was 66 days (P = 0.0372). For the first episode of significant CMV PCR positivity, the mean index and peak CMV PCR counts for those who had received campath/fludarabine/melphalan were 4.54 and 5.22 log copies/ml respectively, while for cyclophosphamide/TBI, the corresponding figures were 3.85 and 4.12 log copies/ml respectively (P = 0.2986 and P = 0.0472 for index and peak values). 85% of those who had significant CMV PCR positivity with the campath/fludarabine/melphalan regimen developed more than one such episode, while 50% of those receiving cyclophosphamide/TBI regimen did so (P = 0.491). Significant CMV PCR positivity was associated with symptoms in a proportion of patients (pyrexia 45%, cough 18%, rise in AST 72%). No patient developed overt CMV disease. CMV PCR is useful for guiding pre-emptive anti-CMV therapy and for monitoring response. Bone Marrow Transplantation (2001) 27, 301–306.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Nguyen Q, Champlin R, Giralt S et al. Late cytomegalovirus pneumonia in adult allogeneic blood and marrow transplant recipients Clin Infect Dis 1999 28: 618–623
Noble S, Faulds D . Ganciclovir. An update of its use in the prevention of cytomegalovirus infection and disease in transplant recipients Drugs 1998 56: 115–146
Stocchi R, Ward KN, Fanin R et al. Management of human cytomegalovirus infection and disease after allogeneic bone marrow transplantation Haematologica 1999 84: 71–79
Prentice HG, Kho P . Clinical strategies for the management of cytomegalovirus infection and disease in allogeneic bone marrow transplant Bone Marrow Transplant 1997 19: 135–142
Milpied N . Prophylaxis of cytomegalovirus infection in bone marrow transplant patients Int J Antimicrobial Agents 1996 7: 277–281
Tsinontides AC, Bechtel TP . Cytomegalovirus prophylaxis and treatment following bone marrow transplantation Ann Pharmacother 1996 30: 1277–1290
Zaia JA, Forman SJ . Cytomegalovirus infection in the bone marrow transplant recipient Infect Dis Clin North Am 1995 9: 879–900
Griffiths PD . Prophylaxis against CMV infection in transplant patients J Antimicrob Chemother 1997 39: 299–301
Salzberger B, Bowden RA, Hackman RC . Neutropenia in allogeneic marrow transplant recipients receiving ganciclovir for the prevention of cytomegalovirus disease: risk factors and outcome Blood 1997 90: 2502–2508
Carella AM, Camplin R, Slavin S et al. Mini-allografts: ongoing trials in humans Bone Marrow Transplant 2000 25: 345–350
Guiver M, Fox AJ, Mutton K et al. Comparative evaluation of CMV viral load using Taqman quantitative CMV PCR and comparison with CMV antigenaemia in heart and lung transplants Transplantation (in press)
Keating MJ, O'Brien S, Lerner S et al. Long-term follow-up of patients with chronic lymphocytic leukemia (CLL) receiving fludarabine regimens as initial therapy Blood 1998 92: 1165–1171
Osterborg A, Fassas AS, Anagnostopoulos A et al. Humanized CD52 monoclonal antibody Campath-1H as first line treatment in chronic lymphocytic leukaemia Br J Haematol 1996 93: 151–153
Grigg A, Chapman R, Szer J . Fatal CMV pneumonia associated with steroid therapy after autologous transplantation in patients previously treated with fludarabine Bone Marrow Transplant 1998 21: 619–621
Bowen AL, Zomas A, Emmett E et al. Subcutaneous CAMPATH-1H in fludarabine-resistant/relapsed chronic lymphocytic and B-prolymphocytic leukaemia Br J Haematol 1997 96: 617–619
Manteiga R, Martino R, Sureda A et al. Cytomegalovirus pp65 antigenemia-guided pre-emptive treatment with ganciclovir after allogeneic stem transplantation: a single-center experience Bone Marrow Transplant 1998 22: 899–904
Koehler M, St George K, Ehrlich GD et al. Prevention of CMV disease in allogeneic BMT recipients by cytomegalovirus antigenemia-guided preemptive ganciclovir therapy J Pediatr Hematol Oncol 1997 19: 43–47
Humar A, O'Rourke K, Lipton J et al. The clinical utility of CMV surveillance cultures and antigenemia following bone marrow transplantation Bone Marrow Transplant 1999 23: 45–51
Egan JJ, Barber L, Lomax J et al. Detection of human cytomegalovirus antigenaemia: a rapid diagnostic technique for predicting cytomegalovirus infection/pneumonitis in lung and heart transplant recipients Thorax 1995 50: 9–13
Ljungman P, Aschan J, Lewensohn-Fuchs I et al. Results of different strategies for reducing cytomegalovirus-associated mortality in allogeneic stem cell transplant recipients Transplantation 1998 66: 1330–1334
Boeckh M, Gallez-Hawkins GM, Myerson D et al. Plasma polymerase chain reaction for cytomegalovirus DNA after allogeneic marrow transplantation: comparison with polymerase chain reaction using peripheral blood leukocytes, pp65 antigenemia, and viral culture Transplantation 1997 64: 108–113
Matsunaga T, Sakamaki S, Ishigaki S et al. Use of PCR serum in diagnosing and monitoring cytomegalovirus reactivation in bone marrow transplant recipients Int J Hematol 1999 69: 105–111
Kanda Y, Chiba S, Suzuki T et al. Time course analysis of semi-quantitative PCR and antigenaemia assay for prevention of cytomegalovirus disease after bone marrow transplantation Br J Haematol 1998 100: 222–225
Emery VC, Sabin CA, Cope AV et al. Application of viral-load kinetics to identify patients who develop cytomegalovirus disease after transplantation Lancet 2000 355: 2032–2036
Acknowledgements
We thank the staff on the Acute Leukaemia Unit at the Christie Hospital for their assistance during this study.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Qamruddin, A., Oppenheim, B., Guiver, M. et al. Screening for cytomegalovirus (CMV) infection in allogeneic bone marrow transplantation using a quantitative whole blood polymerase chain reaction (PCR) method: analysis of potential risk factors for CMV infection. Bone Marrow Transplant 27, 301–306 (2001). https://doi.org/10.1038/sj.bmt.1702778
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1702778
Keywords
This article is cited by
-
CMV quantitative PCR in the diagnosis of CMV disease in patients with HIV-infection – a retrospective autopsy based study
BMC Infectious Diseases (2007)
-
The effect of quantification standards used in real-time CMV PCR assays on guidelines for initiation of therapy in allogeneic stem cell transplant patients
Bone Marrow Transplantation (2007)
-
Low mortality of children undergoing hematopoietic stem cell transplantation from 7 to 8/10 human leukocyte antigen allele-matched unrelated donors with the use of antithymocyte globulin
Bone Marrow Transplantation (2006)
-
Once daily ganciclovir as initial pre-emptive therapy delayed until threshold CMV load ⩾10000 copies/ml: a safe and effective strategy for allogeneic stem cell transplant patients
Bone Marrow Transplantation (2006)
-
A novel reduced intensity regimen for allogeneic hematopoietic stem cell transplantation associated with a reduced incidence of graft-versus-host disease
Bone Marrow Transplantation (2004)