Abstract
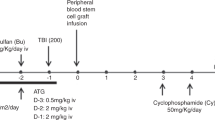
Thrombotic thrombocytopenic purpura (TTP) has emerged as one of the main transplant-related complications over the last 15 years. The current study defines the incidence and the risk factors for the occurrence of TTP in 131 consecutive leukemic children who were transplanted between January 1994 and December 1997 at four Italian pediatric centers. Patients with ALL (101), AML (21), MDS (9), underwent an HLA-identical sibling BMT (82) or an HLA-identical unrelated BMT (49), receiving a conditioning regimen consisting of high-dose chemotherapy in 24 patients and of F-TBI combined with high-dose chemotherapy in 107 patients. The diagnosis of TTP was retrospectively evaluated on the basis of parallel criteria. TTP treatment varied according to the protocol of each treatment center. Twenty-eight of 131 patients (21.4%) developed TTP at a median of 46 days (range 21–80) after BMT. Multivariate analysis demonstrated that the risk of TTP was higher in patients who underwent unrelated BMT (P value = 0.02). Acute GVHD, stage of disease at BMT, conditioning with TBI, gender, age, did not appear to be associated with the occurrence of TTP. As to the outcome, TTP resolved in 19 patients while in nine it was the principal cause of death (32.1%). In patients with TTP, LDH peak value was the only statistically significant factor (P = 0.001) related to severe TTP. In conclusion, our experience demonstrates that leukemic children undergoing BMT, especially from an unrelated donor, should be carefully assessed for TTP which appears to be a severe and relatively common transplant-related complication when strict diagnostic criteria are applied. Bone Marrow Transplantation (2000) 26, 1005–1009.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Spruce WE, Forman SJ, Blume KG et al. Hemolytic uremic syndrome after bone marrow transplantation Acta Haematol 1982 67: 206–210
Juckett M, Perry EH, Daniels BS et al. Hemolytic uremic syndrome following bone marrow transplantation Bone Marrow Transplant 1991 7: 405–409
Holler E, Kolb JH, Hiller F et al. Microangiopathy in patients on cyclosporine prophylaxis who developed acute graft-vs-host-disease after HLA-identical bone marrow transplantation Blood 1989 73: 2018–2024
Pettitt AR, Clark RE . Thrombotic microangiopathy following bone marrow transplantation Bone Marrow Transplant 1994 14: 495–504
Valilis PH, Zeigler ZR, Shadduck RK et al. A prospective study of bone marrow transplant associated thrombotic microangiopathy (BMT-TM) in autologous and allogeneic BMT Blood 1995 86: 970a (Abstr.)
Schriber JR, Herzig GP . Transplantation-associated thrombotic thrombocytopenic purpura and hemolytic uremic syndrome Semin Hematol 1997 34: 126–133
Zeigler ZR, Shadduck RK, Nemumaitis J et al. Bone marrow transplant-associated thrombotic microangiopathy: a case series Bone Marrow Transplant 1995 15: 247–253
Iacopino P, Pucci G, Arcese W et al. Severe thrombotic microangiopathy: an infrequent complication of bone marrow transplantation Bone Marrow Transplant 1999 24: 47–51
George JM, Berkowitz SD, Raskob GE . Platelets: acute thrombocytopenia – thrombotic thrombocytopenic purpura and hemolytic uremic syndrome. The ASH Meeting Blood Education Program Book 1998 379–383
Bennett JM, Catovsky D, Daniel MT et al. Proposals for the classification of the acute leukemias: French–American–British (FAB) Cooperative Group Br J Haematol 1976 33: 451–458
Bennett JM, Catovsky D, Daniel MT et al. Proposed revised criteria for the classification of acute myeloid leukemia: a report of the French–American–British cooperative group Ann Intern Med 1985 103: 626–629
Sullivan KM . Graft versus host disease. In: Thomas ED, Blume KG, Forman SJ (eds) Hematopoietic Cell Transplantation 2nd edn. Blackwell Science: USA 1999 pp 515–536
Uderzo C, Valsecchi MG, Bacigalupo A et al. Treatment of childhood acute lymphoblastic leukemia in second remission with allogeneic bone marrow transplantation and chemotherapy: ten-year experience of the Italian Bone Marrow Transplantation Group and the Italian Pediatric Hematology oncology Association J Clin Oncol 1995 13: 352–358
Van Lint MT, Uderzo C, Locasciulli A et al. Early treatment of acute graft-vs-host disease with high or low dose 6-methylprednisolone: a multicenter randomized trial from the Italian Group for Bone Marrow Transplantation Blood 1998 92: 2288–2293
Hosmer DN, Lemeshow S . Applied Logistic Regression Wiley & Sons: New York 1989 pp 25–36
Busca A, Uderzo C . Bone marrow transplant associated thrombotic microangiopathy Hematology 2000 5: 53–67
Kondo M, Kojima S, Horibe K et al. Hemolytic uremic syndrome after allogeneic or autologous hemapoietic stem cell transplantation for childhood malignancies Bone Marrow Transplant 1998 21: 281–286
Guinan EC, Tarbell J, Niemeyer CM et al. Intravascular hemolysis and renal insufficiency after BMT Blood 1998 72: 451–455
Rock AG, Shumak KH, Buskard NA . et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura New Engl J Med 1991 325: 393–397
Dua A, Zeigler Z, Shadduck RK et al. Apheresis in grade four bone marrow transplant associated thrombotic microangiopathy: a case series J Clin Apheresis 1996 11: 176–184
Sarode R, McFarland JC, Flamemberg N et al. Therapeutic plasma exchange does not appear to be effective in the management of TTP and hemolytic uremic syndrome following bone marrow transplantation Bone Marrow Transplant 1995 16: 271–275
Zeigler ZR, Shadduck RK, Nath R et al. Pilot study of combined cryosupernatant and protein A immunoadsorption exchange in the treatment of grade 3–4 bone marrow transplantation associated thrombotic microangiopathy Bone Marrow Transplant 1996 17: 81–86
Wada H, Kaneko T, Ohiwa M et al. Plasma cytokine levels in thrombotic thrombocytopenic purpura Am J Hematol 1992 40: 167–170
Krenger W, Hill GR, Ferrara JLM . Cytokine cascades in acute graft-versus-host disease Transplantation 1997 64: 553–558
Chong BH, Murray B, Berndt MC et al. Plasma P-selectin is increased in thrombotic consumptive platelet disorders Blood 1994 83: 1535–1541
Anthony MT, Zeigler ZR, Lister J et al. Plasminogen activator inhibitor (PAI-1) antigen levels in primary TTP and secondary TTP post bone marrow transplantation Am J Hematol 1998 59: 9–14
Moake JL, Rudy CK, Troll JH . Unusually large plasma VIII von Willebrand factor multimers in chronic relapsing thrombotic thrombocytopenic purpura New Engl J Med 1982 307: 1432–1436
Natazuka T, Kajimoto K, Ogawa R et al. Coagulation abnormalities and thrombotic microangiopathy following bone marrow transplantion from HLA-matched unrelated donors in patients with hematological malignancies Bone Marrow Transplant 1998 21: 815–819
Llamas P, Romero R, Cabrera R et al. Management of thrombotic microangiopathy following allogeneic transplantation: what is the role of plasma exchange? Bone Marrow Transplant 1997 20: 305–306
Clark WF, Rock GA, Buskard N et al. Therapeutic plasma exchange: an update from Canadian Apheresis Group Ann Intern Med 1999 131: 453–462
Atkinson K, Biggs JC, Hayes J . Cyclosporin A associated nephrotoxicity in the first 100 days after BMT: three distinct syndromes Br J Haematol 1983 54: 59–67
Srivastava A, Gottlieb D, Bradstock KF . Diffuse alveolar haemorrhage associated with microangiopathy after allogeneic bone marrow transplantation Bone Marrow Transplant 1995 15: 863–867
Carlson K, Smedmyr B, Hagberg H et al. Haemolytic uraemic syndrome and renal disfunction following BEAC (BCNU, etoposide, ara-c, cyclophosphamide) plus/minus TBI and autologous BMT for malignant lymphomas Bone Marrow Transplant 1993 11: 205–208
Uderzo C, Fumagalli M, De Lorenzo P et al. Thrombotic thrombocytopenic purpura (TTP) as early complication in children who undergo bone marrow transplantation Blood 1999 94:: (Suppl. 1) 363b (Abstr.)
Hamblin N, Powles R, Treleaven J et al. Defibrotide for refractory thrombotic thrombocytopenic purpura after bone marrow transplantation Blood 1996 88: (10 Suppl.) 2966
Bayik MM, Akoglu T, Tuglular TF et al. Treatment of TTP with defibrotide Am J Hematol 1993 43: 74–75
Mantovani M, Primo G, Pescador R . Activation of fibrinolytic process by a substance of polydesoxyriboneucleotidic nature (fraction P), in strand, advance in coagulation, fibrinolysis and platelet aggregation and aterosclerosis. CEPI: Rome 1978 pp 274–281
Violi F, Ferro D, Alessandri C et al. Inhibition of tissue plasminogen activator inhibitor by defibrotide in aterosclerotic patients Semin Thromb Haematol 1989 15: 226–229
Pogliani EM, Salvatore M, Foust C et al. Effects of defibrotide-heparin combination of some measures of haemostasis in health volunteers J Intern Med Res 1989 17: 36–40
Richardson PG, Elias AD, Krishnan A . Treatment of severe venoocclusive disease with defibrotide: compassionate use results in response without significant toxicity in high-risk population Blood 1998 92: 737–744
Acknowledgements
We would like to thank the ‘Comitato Maria Letizia Verga per lo Studio e Cura della Leucemia del Bambino’, the Associazione Italiana Ricerca Cancro and Miss Joanna Upton for her language review.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Uderzo, C., Fumagalli, M., De Lorenzo, P. et al. Impact of thrombotic thrombocytopenic purpura on leukemic children undergoing bone marrow transplantation. Bone Marrow Transplant 26, 1005–1009 (2000). https://doi.org/10.1038/sj.bmt.1702648
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1702648
Keywords
This article is cited by
-
Role of the lectin pathway of complement in hematopoietic stem cell transplantation-associated endothelial injury and thrombotic microangiopathy
Experimental Hematology & Oncology (2021)
-
Use of defibrotide to treat adult patients with transplant-associated thrombotic microangiopathy
Bone Marrow Transplantation (2019)
-
Successful Treatment of Transplant Associated Thrombotic Microangiopathy (TA-TMA) with Low Dose Defibrotide
Indian Journal of Hematology and Blood Transfusion (2018)
-
Transplant-associated thrombotic microangiopathy: opening Pandora’s box
Bone Marrow Transplantation (2017)
-
Remission of Microangiopathy in Transplanted Thalassemic Child
Indian Journal of Hematology and Blood Transfusion (2014)