Abstract
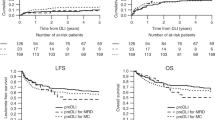
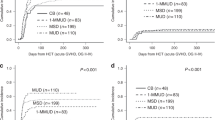
To clarify the role of donor leukocyte infusion (DLI) in the treatment of leukemia relapsing after allo-BMT, data from 100 patients were collected from 46 facilities in Japan and analyzed with respect to the efficacy and adverse effects of donor leukocyte infusion. Complete remission was achieved in 11 of 12 (91%) patients with relapsed chronic myelogenous leukemia (CML) in chronic phase, three of 11 (27%) with CML in the acute phase, eight of 21 (38%) with acute myelogenous leukemia (AML), six of 23 (25%) with acute lymphoblastic leukemia (ALL) and five of 11 (45%) with myelodysplastic syndrome (MDS). The probability of remaining in CR at 3 years was 82% in CML patients in the chronic phase, but 0% in those with CML in the acute phase, 7% in those with AML, 0% with ALL and 33% with MDS. Acute GVHD (⩾2) developed in 31 of 89 (34%) patients with HLA-identical related donors and was fatal for seven (7%). Cytopenia developed in 21 of 94 (22%) with no associated fatalities. When the outcome of patients with CML in CP and MDS was analyzed, development of GVHD, cytopenia, or both, was associated with a higher GVL effect (15 of 16, 93%) than in those without adverse affects (one of 6, 17%). A leukocyte dose of 5 × 107/kg of recipient body weight appeared to be optimal as an initial dose of DLI. Given the relatively low incidence of acute GVHD and the similar GVL effect, DLI may be more beneficial to patients in Japan with recurrent leukemia than to those in Western countries. Bone Marrow Transplantation (2000) 26, 769–774.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Kolb HJ, Mittermuller J, Clemm C et al. Donor leukocyte transfusions for treatment of recurrent chronic myelogenous leukemia in marrow transplant patients Blood 1990 76: 2462–2465
Collis JO, Jiang YZ, Schwarer AP et al. Donor leukocyte infusions for chronic myelogenous leukemia in relapse after allogeneic bone marrow transplantation Blood 1992 79: 1379–1380
Drobyski WR, Keever CA, Roth MS et al. Salvage immunotherapy using donor leukocyte infusions as treatment for relapsed chronic myelogenous leukemia after allogeneic bone marrow transplantation; efficiency and toxicity of a defined T-cell dose Blood 1993 82: 2310–2318
Helg C, Roux E, Beris P et al. Adoptive immunotherapy for recurrent CML after BMT Bone Marrow Transplant 1993 12: 125–129
Slavin S, Naparstek E, Naglar A et al. Allogeneic cell therapy for relapsed leukemia after bone marrow transplantation with donor peripheral blood lymphocytes Exp Hematol 1995 23: 1553–1562
Kolb HJ, Schattenberg A, Goldman JM et al. Graft-versus-leukemia effect of donor lymphocyte transfusions in marrow grafted patients Blood 1995 86: 2041–2050
Collins RH, Shpilberg JO, Drobyski WR et al. Donor leukocyte infusions in 140 patients with relapsed malignancy after allogeneic bone marrow transplantation J Clin Oncol 1997 15: 433–444
Weiden PL, Flournoy N, Thomas ED et al. Antileukemic effect of graft-versus-host disease in human recipients of allogeneic marrow grafts New Engl J Med 1979 300: 1068–1073
Sullivan KM, Storb R, Buckner CD et al. Graft-versus-host disease as adoptive immunotherapy in patients with advanced hematologic neoplasms New Engl J Med 1989 320: 828–834
Morishima Y, Kodera Y, Hirabayashi N et al. Low incidence of acute GVHD in patients transplanted with marrow from HLA-A,B,DR-compatible unrelated donors among Japanese Bone Marrow Transplant 1995 15: 235–239
Sasazuki T, Juji T, Morishima Y et al. Effect of matching of class I HLA alleles on clinical outcome after transplantation of hematopoietic stem cells from an unrelated donor. Japan Marrow Donor Program New Engl J Med 1998 22: 1177–1185
Kodera Y, Morishima Y, Kato S et al. Analysis of 500 bone marrow transplants from unrelated donors (UR-BMT) facilitated by the Japan Marrow Donor Program: confirmation of UR-BMT as a standard therapy for patients with leukemia and aplastic anemia Bone Marrow Transplant 1999 24: 995–1003
Alyea EP, Soiffer RJ, Canning C et al. Toxicity and efficacy of defined doses of CD4+ donor lymphocytes for treatment of relapse after allogeneic bone marrow transplant Blood 1998 91: 3671–3680
Slavin S, Naparstek E, Nagler A et al. Allogeneic cell therapy with donor peripheral blood cells and recombinant human interleukin-2 to treat leukemia relapse after allogeneic bone marrow transplantation Blood 1996 87: 2195–2204
Ogawa H, Tsuboi A, Oji Y et al. Successful donor leukocyte transfusion at molecular relapse for a patient with acute myeloid leukemia who was treated with allogenic bone marrow transplantation: importance of the monitoring of minimal residual disease by WT1 assay Bone Marrow Transplant 1998 21: 525–527
Yazaki M, Andou M, Ito T et al. Successful prevention of hematological relapse for a patient with Philadelphia-positive acute lymphoblastic leukemia after allogeneic bone marrow transplantation by donor leukocyte infusion Bone Marrow Transplant 1997 19: 393–394
Wagner FF, Flegel WA . Transfusion-associated graft-versus-host disease: risk due to homozygous HLA haplotype Transfusion 1995 35: 284–291
Mackinnon S, Papadopoulos EB, Carabasi MH et al. Adoptive immunotherapy evaluating escalating doses of donor leukocytes for relapse of chronic myeloid leukemia after bone marrow transplantation: separation of graft-versus-leukemia responses from graft-versus-host disease Blood 1995 86: 1261–1268
Acknowledgements
This work was supported in part by a grant-in-aid for Cancer Research 7–3 from the Ministry of Health and Welfare.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Shiobara, S., Nakao, S., Ueda, M. et al. Donor leukocyte infusion for Japanese patients with relapsed leukemia after allogeneic bone marrow transplantation: lower incidence of acute graft-versus-host disease and improved outcome. Bone Marrow Transplant 26, 769–774 (2000). https://doi.org/10.1038/sj.bmt.1702596
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1702596
Keywords
This article is cited by
-
Safety and efficacy of immune checkpoint inhibitors after allogeneic hematopoietic cell transplantation
Bone Marrow Transplantation (2023)
-
Relapse after allogeneic hematopoietic stem cell transplantation in acute myeloid leukemia: an overview of prevention and treatment
International Journal of Hematology (2022)
-
Donor-derived anti-CD19 CAR T cells compared with donor lymphocyte infusion for recurrent B-ALL after allogeneic hematopoietic stem cell transplantation
Bone Marrow Transplantation (2021)
-
The FLAMSA concept—past and future
Annals of Hematology (2020)
-
Haploidentical CD19/CD22 bispecific CAR-T cells induced MRD-negative remission in a patient with relapsed and refractory adult B-ALL after haploidentical hematopoietic stem cell transplantation
Journal of Hematology & Oncology (2019)