Abstract
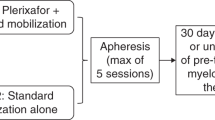
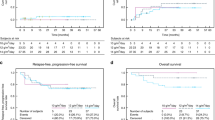
A phase I dose-escalation study of multicyclic, ifosfamide, carboplatin, and etoposide (ICE) with sequential reinfusion of peripheral blood stem cells (PBSCs) was conducted to determine the maximum-tolerated dose (MTD) of ICE. Twenty-four patients with SCLC (LD: 6, ED: 18) were treated with ifosfamide (3000–9000 mg/m2, 24-h infusion), carboplatin (300–400 mg/m2), and etoposide (300 mg/m2) followed by subcutaneous filgrastim (75 μg/day) from day 4 to the day of PBSC collection. PBSC were harvested when the WBC count reached ⩾5 × 109/l. The leukapheresis product was cryopreserved and reinfused on day 4 of the next cycle, which was started 48 h after the last PBSC collection. The ifosfamide dose was escalated as follows: 3000 mg/m2 (level 1), 5000 mg/m2 (level 2), 7000 mg/m2 (level 3), 9000 mg/m2 (level 4). Patients with LD were treated with concurrent radiotherapy at 1.5 Gy twice daily for the initial 3 weeks to a total dose of 45 Gy and MTD, defined separately. Patients were evaluated for hematologic and non-hematologic toxicity, actual dose intensities, as well as response to therapy. The maximum-tolerated dose (MTD) was defined as the dose level at which more than 5 days of grade 4 myelo- suppression or non-hematologic toxicity greater than grade 3 developed in two thirds of the patients. For ED cases, MTD was level 4 and the recommended dose of ifosfamide was 7000 mg/m2. For LD cases, the recommended dose of ifosfamide was 5000 mg/m2. The dose limiting toxicity of multicyclic ICE was hemato- logic toxicity and CNS toxicity which manifested as ataxia. Tumor responses were seen in all patients, with 14 patients showing a complete response. The actual total dose-intensity at the recommended dose level was 2.2 and 1.74, for ED and LD, respectively, compared with previously reported ICE regimens. PBSC support for dose-intensive ICE regimen permitted dose escalation of ifosfamide with a mean interval of 16–17 days. We conclude that this regimen is well tolerated, with acceptable hematological and non-hematological toxicity. Bone Marrow Transplantation (2000) 25, 5–11.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Gurney H, Dodwell D, Thatcher N, Tattersall MH . Escalating drug delivery in cancer chemotherapy: a review of concepts and practice – part 1 Ann Oncol 1993 4: 23–34
Gurney H, Dodwell D, Thatcher N, Tattersall MH . Escalating drug delivery in cancer chemotherapy: a review of concepts and practice – part 2 Ann Oncol 1993 4: 103–115
Coldman AJ, Goldie JH . Impact of dose-intense chemotherapy on the development of permanent drug resistance Semin Oncol 1987 14: (Suppl.4) 29–33
DeVita VT Jr . The influence of information on drug resistance on protocol design Ann Oncol 1991 2: 93–106
Arriagada R, Le Chevalier T, Pignon JP et al. Initial chemotherapeutic doses and survival in patients with limited small-cell lung cancer New Engl J Med 1993 329: 1848–1852
Humblet Y, Symann M, Bosly A et al. Late intensification chemotherapy with autologous bone marrow transplantation in selected small-cell carcinoma of the lung: a randomized study J Clin Oncol 1987 5: 1864–1873
Shea TC, Mason JR, Storniolo AM et al. Sequential cycles of high-dose carboplatin administered with recombinant human granulocyte–macrophage colony-stimulating factor and repeated infusions of autologous peripheral blood progenitor cells: a novel and effective method for delivering multiple courses of dose-intensive therapy J Clin Oncol 1992 10: 464–473
Tepler I, Cannistra SA, Frei E et al. Use of peripheral blood progenitor cells abrogates the myelotoxicity of repetitive outpatient high-dose carboplatin and cyclophosphamide chemotherapy J Clin Oncol 1993 11: 1583–1591
Pettengell R, Woll PJ, Thatcher N et al. Multicyclic, dose-intensive chemotherapy supported by sequential reinfusion of hematopoietic progenitors in whole blood J Clin Oncol 1995 13: 148–156
Kohno A, Takeyama K, Narabayashi M et al. Low-dose granulocyte colony-stimulating factor enables the efficient collection of peripheral blood stem cells after disease-oriented, conventional-dose chemotherapy for breast cancer, malignant lymphoma and germ cell tumor Bone Marrow Transplant 1995 15: 49–54
Martinez C, Sureda A, Martino R et al. Efficient peripheral blood stem cell mobilization with low-dose G-CSF (50μg/m2) after salvage chemotherapy for lymphoma Bone Marrow Transplant 1997 20: 855–858
Hryniuk W, Bush H . The importance of dose intensity in chemotherapy of metastatic breast cancer J Clin Oncol 1984 2: 1281–1288
Smith IE, Perren TJ, Ashley SA et al. Carboplatin, etoposide, and ifosfamide as intensive chemotherapy for small-cell lung cancer J Clin Oncol 1990 8: 899–905
Gatzemeier U, Hossfeld DK, Neuhauss R et al. Combination chemotherapy with carboplatin, etoposide, and vincristine as first-line treatment in small-cell lung cancer J Clin Oncol 1992 10: 818–823
Loehrer PJ Sr, Rynard S, Ansari R et al. Etoposide, ifosfamide, and cisplatin in extensive small cell lung cancer Cancer 1992 69: 669–673
Seifter EJ, Ihde DC . Therapy of small cell lung cancer: a perspective on two decades of clinical research Semin Oncol 1988 15: 278–299
Skarlos DV, Samantas E, Kosmidis P et al. Randomized comparison of etoposide-cisplatin vs etoposide-carboplatin and irradiation in small-cell lung cancer. A Hellenic Co-operative Oncology Group study Ann Oncol 1994 5: 601–607
Thatcher N . Ifosfamide/carboplatin/etoposide (ICE) regimen in small cell lung cancer Lung Cancer 1993 9: S51–S67
Blackstein ME . Advances in chemotherapy for small cell lung cancer Semin Oncol 1994 21: (Suppl. 1) 38–42
Van der Wall E, Richel DJ, Holtkamp MJ et al. Bone marrow reconstitution after high-dose chemotherapy and autologous peripheral blood progenitor cell transplantation: effect of graft size Ann Oncol 1994 5: 795–802
Woll PJ, Hodgetts J, Lomax L et al. Can cytotoxic dose intensity be increased by using granulocyte colony-stimulating factor? A randomized controlled trial of lenograstim in small-cell lung cancer J Clin Oncol 1995 13: 652–659
Thatcher N, Sambrook RJ, Stephens RJ et al . Dose intensification (DI) with G-CSF improves survival in small cell lung cancer (SCLC): results of a randomized trial Proc Am Soc Clin Oncol 1998 18:: (Abstr. 1754) 17456a
Pignon JP, Arriagada R, Ihde DC et al. A meta-analysis of thoracic radiotherapy for small-cell lung cancer (see comments) New Engl J Med 1992 327: 1618–1624
Murray N, Coy P, Pater JL et al. Importance of timing for thoracic irradiation in the combined modality treatment of limited-stage small-cell lung cancer. The National Cancer Institute of Canada Clinical Trials Group J Clin Oncol 1993 11: 336–344
Perry MC, Herndon JE, Eaton WL, Green MR . Thoracic radiation therapy added to chemotherapy for small-cell lung cancer: an update of Cancer and Leukemia Group B Study 8083 J Clin Oncol 1998 16: 2466–2467
Turrisi AT, Kim K, Blum R et al. Twice-daily compared with once-daily thoracic radiotherapy in limited small-cell lung cancer treated concurrently with cisplatin and etoposide New Engl J Med 1999 340: 265–271
Acknowledgements
We are grateful to Satomi Takeuchi for technical assistance.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Takahashi, M., Yoshizawa, H., Tanaka, H. et al. A phase I dose escalation study of multicyclic, dose-intensive chemotherapy with peripheral blood stem cell support for small cell lung cancer. Bone Marrow Transplant 25, 5–11 (2000). https://doi.org/10.1038/sj.bmt.1702088
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1702088
Keywords
This article is cited by
-
Successful liquid storage of peripheral blood stem cells at subzero non-freezing temperature
Bone Marrow Transplantation (2002)