Abstract
Background/Objectives:
Investigate dietary salt intake trends by gender, and their associations with risk factors for cardiovascular diseases in Geneva, Switzerland.
Subjects/Methods:
Continuous surveillance of the Geneva general adult (35–74 years) population for 12 years (1993–2004) using a validated, semi-quantitative food frequency questionnaire (FFQ) in random, cross-sectional, representative samples (6688 men, 6647 women). Dietary salt intake assessment by FFQ excluded discretionary salt, but was calibrated on total salt intake using an independent validation substudy of 100 volunteers who additionally provided 24-h urine collections.
Results:
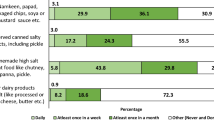
Quartiles (mean) of calibrated dietary salt intake (g per day) were 9.9, 10.5, 11.2 (10.6) in men, and 7.0, 7.8, 8.9 (8.1) in women and were above current recommendations. Quartiles (mean) of salt density (g MJ−1) were 0.99, 1.16, 1.39 (1.23) in men, and 0.98, 1.12, 1.30 (1.17) in women. Both measures were stable during the 12-year surveillance period, regardless of hypertension treatment. Salt-density differences between cardiovascular disease risk factor subgroups were moderate. Salt density increased with age and body mass index. The main dietary non-discretionary salt food sources (men/women: 47/48%) were breads (17/17%), cheeses (11/10%), meat and meat products (8/7%), soups (6/9%) and ready-to-eat foods (5/5%).
Conclusions:
Salt intakes from all sources for the Geneva, and perhaps the Swiss adult population are above current recommendations. The quantitative and qualitative data provided in this paper could be used to develop and implement strategies for salt-intake reduction in Switzerland.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Agence française de sécurité sanitaire des aliments (ed). (2001). Apports Nutritionnels Conseillés Pour La Population Française. Editions TEC & DOC: Paris.
Agence française de sécurité sanitaire des aliments (ed). (2002). Rapport du groupe de travail sur le sel (Report of the salt working group 4.1.2002)http://www.afssa.fr/ftp/basedoc/rapportselnet2.pdf; 24.10.2006.
aid (ed) (2002). Salz in unserer Nahrung. aid-Heft 1014. aid infodienst Verbraucherschutz Ernährung Landwirtschaft eV: Bonn.
Alderman MH (2002). Salt, blood pressure and health: a cautionary tale. Int J Epidemiol 31, 311–315.
Bates CJ, Thurnham DI, Bingham SA, Margetts BM, Nelson M (1997). Biochemical markers of nutrient intake. In Margetts BM and Nelson M (eds). Design Concepts in Nutritional Epidemiology. Oxford University Press: Oxford. pp 170–240.
Beer-Borst S, Costanza MC, Pechère-Bertschi A, Wolff H, Burnier M, Morabia A (2006). Calibration of Geneva Adult Population Dietary Sodium (salt) Intake Estimates from Food Frequency Questionnaire (FFQ): Validation Study Comparing FFQ versus 24-h Urinary Measurements of Sodium and Potassium. Report on behalf of the Swiss Federal Office of Public Health, Berne, 28.09.2006 (available on http://www.bag.admin.ch/themen/ernaehrung/00211/03529/03534/index.html?lang=de; choose ‘Von der Genfer Erwachsenenbevölkerung aufgenommenes Natrium (Kochsalz): Kalibrierung der anhand eines Food Frequency Fragebogens geschätzten Daten’).
Bernstein M, Morabia A, Costanza MC, Landis JR, Ross A, Flandre P et al. (1994). [Nutritional balance of the diet of the adult residents of Geneva]. Soz Praventiv Med 39, 333–344.
Centre Informatique sur la Qualité des Aliments et Fondation Française pour la Nutrition (ed). (1991). Répertoire Général Des Aliments. Table De Composition. Lavoisier TEC & DOC: Paris.
Costanza MC (2004). Estimating and approximating prevalence trends. Soz Praventiv Med 49, 224–226.
Deutsche Gesellschaft für Ernährung (DGE), Österreichische Gesellschaft für Ernährung (ÖGE), Schweizerische Gesellschaft für Ernährungsforschung (SGE) und Schweizerische Vereinigung für Ernährung (SVE) (eds) (2000). Referenzwerte für die Nährstoffzufuhr. Umschau Braus: Frankfurt am Main.
Elliott P, Stamler J (2002). Evidence on salt and blood pressure is consistent and persuasive. Int J Epidemiol 31, 316–319.
European Commission (2005). The DAFNE food classification system. Operationalisation in 16 European Countries. European Commission: Luxembourg.
Galobardes B, Costanza MC, Bernstein MS, Delhumeau C, Morabia A (2003). Trends in risk factors for lifestyle-related diseases by socioeconomic position in Geneva, Switzerland, 1993–2000: health inequalities persist. Am J Public Health 93, 1302–1309.
Geleijnse JM, Grobbee DE, Koks FJ (2005). Impact of dietary and lifestyle factors on the prevalence of hypertension in Western populations. J Hum Hypertens 19 (Suppl 3), S1–S4.
He J, Whelton PK (2002). Salt intake, hypertension and risk of cardiovascular disease: an important public health challenge. Int J Epidemiol 31, 327–331.
Henderson L, Irving K, Gregory J (2003). The national diet & nutrition survey: adults aged 19–64 years. Vitamin and Mineral Intake and Urinary Analytes (Volume 3) TSO: London.
Joint WHO/FAO Expert Consultation (2003). Diet, Nutrition and the Prevention of Chronic Diseases WHO Technical Report Series 916 WHO: Geneva.
Kaplan NM (2000). The dietary guideline for sodium: should we shake it up? No. Am J Clin Nutr 71, 1020–1026.
Laatikainen T, Pietenen P, Valsta I, Sudval J, Reinivuo H, Tuomilehto J (2006). Sodium in the Finnish diet: 20-year trends in urinary sodium excretion among the adult population. Eur J Clin Nutr 60, 965–970.
Leclercq C, Ferro-Luzzi A (1991). Total and domestic consumption of salt and their determinants in three regions of Italy. Eur J Clin Nutr 45, 151–159.
MacGregor G, de Wardener HE (2002). Salt, blood pressure and health. Int J Epidemiol 31, 320–327.
Männistö S, Reinivuo H, Ovaskainen ML, Tapanainen H, Pietinen P, Valsta L (2003). Dietary factors of cardiovascular disease after 30-years of systematic prevention work. Ann Nutr Metab 47, 439 (abstract).
McCarron DA (2000). The dietary guideline for sodium: should we shake it up? Yes!. Am J Clin Nutr 71, 1013–1019.
McCarron DA (2001). Reply to Strazzullo. Am J Clin Nutr 73, 663–664.
Morabia A, Bernstein M, Kumanyika S, Sorenson A, Mabiala I, Prodolliet B et al. (1994). [Development and validation of a semi-quantitative food questionnaire based on a population survey]. Soz Praventiv Med 39, 345–369.
National Nutrition Council (2005). Finnish Nutrition Recommendations. Ministry of Agriculture and Forestry: Helsinki.
Pietinen P, Vartiainen E, Seppanen R, Aro A, Puska P (1996). Changes in diet in Finland from 1972 to 1992: impact on coronary heart disease risk. Prev Med 25, 243–250.
Reinivuo H, Valsta I, Laatikainen T, Tuomilehto J, Pietenen P (2006). Sodium in the Finnish diet: II trends in dietary sodium intake and comparison between intake and 24-h excretion of sodium. Eur J Clin Nutr 60, 1160–1167.
Sanchez-Castillo CP, Warrender S, Whitehead TP, James WP (1987). An assessment of the sources of dietary salt in a British population. Clin Sci (Lond) 72, 95–102.
Scientific Advisory Committee on Nutrition (2003). Salt and Health. TSO: Norwich, UK.
Strazzullo P (2001). The salt controversy at the turn of the century: no to prejudiced thinking, yes to concerted action. Am J Clin Nutr 73, 662–663.
Swiss Federal Office of Public Health (SFOPH) and Swiss Federal Institute of Technology Zurich (SFITZ) (eds) (2003). Swiss Food Data [Version 1.0] CD-Rom. SFOPH: Bern.
Thompson FE, Byers T (1994). Dietary assessment resource manual. J Nutr 124, 2245S–2317S.
World Health Organization (2000). Estimating levels and patterns of alcohol consumption from national surveys. In: International Guide for Monitoring Alcohol Consumption and Related Harm. WHO: Geneva. pp 37–62.
Acknowledgements
The surveys were funded by the Swiss National Fund for Scientific Research (Grant nos. 32-31.326.91, 32-37986.93, 32-46142-95, 32-47219.96, 32-49847.96, 32-054097.98, 32-57104.99). The salt-specific studies were funded by the Swiss Federal Office of Public Health (Contracts nos. 03.001605, 05.001008). We also thank Mr Lau Ba-Luong for his assistance in preparing the study-specific sodium database.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guarantor: A Morabia.
Contributors: SBB drafted the paper, supervised Bus Santé surveys/data collection, PI for Swiss Federal Office of Public Health salt studies, compiled sodium food composition table; MCC performed and interpreted all biostatistical analyses, coordinated writing of final version of paper; APB was medical PI of salt validation substudy; AM directed Bus Santé surveys, PI of salt projects. All authors contributed equally to the writing of the final paper.
Conflicts of interest
None declared.
Ethical approval
The surveys were approved by the ethical committee for epidemiological research and public health, Institute for Social and Preventive Medicine at the University of Geneva. The salt intake validation study was approved by the Geneva University Hospital institutional ethics committee.
Rights and permissions
About this article
Cite this article
Beer-Borst, S., Costanza, M., Pechère-Bertschi, A. et al. Twelve-year trends and correlates of dietary salt intakes for the general adult population of Geneva, Switzerland. Eur J Clin Nutr 63, 155–164 (2009). https://doi.org/10.1038/sj.ejcn.1602922
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602922
Keywords
This article is cited by
-
No changes in dietary intake after quitting smoking; a prospective study in Switzerland
BMC Nutrition (2021)
-
The association between adherence to the Mediterranean diet and hepatic steatosis: cross-sectional analysis of two independent studies, the UK Fenland Study and the Swiss CoLaus Study
BMC Medicine (2019)
-
Twenty-four-year trends and determinants of change in compliance with Swiss dietary guidelines
European Journal of Clinical Nutrition (2019)
-
Overlapping spatial clusters of sugar-sweetened beverage intake and body mass index in Geneva state, Switzerland
Nutrition & Diabetes (2019)
-
No association between vitamin C and E supplementation and grip strength over 5 years: the Colaus study
European Journal of Nutrition (2019)