Abstract
Objective:
To study the effect to recommend no snacks vs three snacks per day on 1-year weight loss. The hypothesis was that it is easier to control energy intake and lose weight if snacks in between meals are omitted.
Subjects/Method:
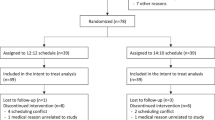
In total 140 patients (36 men, 104 women), aged 18–60 years and body mass index>30 kg/m2 were randomized and 93 patients (27 men, 66 women) completed the study. A 1-year randomized intervention trial was conducted with two treatment arms with different eating frequencies; 3 meals/day (3M) or 3 meals and 3 snacks/day (3+3M). The patients received regular and individualized counseling by dieticians. Information on eating patterns, dietary intake, weight and metabolic variables was collected at baseline and after 1 year.
Results:
Over 1 year the 3M group reported a decrease in the number of snacks whereas the 3+3M group reported an increase (−1.1 vs +0.4 snacks/day, respectively, P<0.0001). Both groups decreased energy intake and E% (energy percent) fat and increased E% protein and fiber intake but there was no differences between the groups. Both groups lost weight, but there was no significant difference in weight loss after 1 year of treatment (3M vs 3+3M=−4.1±6.1 vs −5.9±9.4 kg; P=0.31). Changes in metabolic variables did not differ between the groups, except for high-density lipoprotein that increased in the 3M group but not in 3+3M group (P<0.033 for group difference).
Conclusion:
Recommending snacks or not between meals does not influence 1-year weight loss.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Altman D (1991). Practical Statistics for Medical Research. Chapman & Hall: London. pp 87–88.
Andersson I, Rossner S (1997). Weight development, drop-out pattern and changes in obesity-related risk factors after two years treatment of obese men. Int J Obes Relat Metab Disord 21, 211–216.
Arnold L, Ball M, Mann J (1994). Metabolic effects of alterations in meal frequency in hypercholesterolaemic individuals. Atherosclerosis 108, 167–174.
Arnold L, Mann JI, Ball MJ (1997). Metabolic effects of alterations in meal frequency in type 2 diabetes. Diabetes Care 20, 1651–1654.
Arnold LM, Ball MJ, Duncan AW, Mann J (1993). Effect of isoenergetic intake of three or nine meals on plasma lipoproteins and glucose metabolism. Am J Clin Nutr 57, 446–451.
Basdevant A, Craplet C, Guy-Grand B (1993). Snacking patterns in obese French women. Appetite 21, 17–23.
Beebe CA, Van Cauter E, Shapiro ET, Tillil H, Lyons R, Rubenstein AH et al. (1990). Effect of temporal distribution of calories on diurnal patterns of glucose levels and insulin secretion in NIDDM. Diabetes Care 13, 748–755.
Bellisle F, McDevitt R, Prentice AM (1997). Meal frequency and energy balance. Br J Nutr 77, S57–S70.
Bertéus Forslund H, Lindroos A, Sjöström L, Lissner L (2002). Meal patterns and obesity in Swedish women—a simple instrument describing usual meal types, frequency and temporal distribution. Eur J Clin Nutr 56, 740–747.
Bertéus Forslund H, Torgerson JS, Sjostrom L, Lindroos AK (2005). Snacking frequency in relation to energy intake and food choices in obese men and women compared to a reference population. Int J Obes Relat Metab Disord 29, 711–719.
Booth DA (1988). Mechanism from model-actual effects from real life: the zero-calorie drink-break option. Appetite 11 (Suppl), 94–102.
Booth DA, Blair AJ, Lewis VJ, Baek SH (2004). Patterns of eating and movement that best maintain reduction in overweight. Appetite 43, 277–283.
Bray G, Bouchard C (2004). Handbook of Obesity: Etiology and Pathophysiology. Marcel Dekker: Baton Rouge, Louisiana. pp. 453–454.
Brinkworth GD, Noakes M, Keogh JB, Luscombe ND, Wittert GA, Clifton PM (2004). Long-term effects of a high-protein, low-carbohydrate diet on weight control and cardiovascular risk markers in obese hyperinsulinemic subjects. Int J Obes Relat Metab Disord 28, 661–670.
Clark MM, Guise BJ, Niaura RS (1995). Obesity level and attrition: support for patient-treatment matching in obesity treatment. Obes Res 3, 63–64.
Coakley EH, Rimm EB, Colditz G, Kawachi I, Willett W (1998). Predictors of weight change in men: results from the Health Professionals Follow-up Study. Int J Obes Relat Metab Disord 22, 89–96.
de Graaf C (2000). Nutritional definitions of the meal. In: Meiselman H (ed). Dimensions of the Meal. Aspen Publishers: Gaitersburg, MD. pp. 47–56.
DPP (2002). The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 25, 2165–2171.
Drummond S, Crombie N, Kirk T (1996). A critique of the effects of snacking on body weight status. Eur J Clin Nutr 50, 779–783.
Drummond SE, Crombie NE, Cursiter MC, Kirk TR (1998). Evidence that eating frequency is inversely related to body weight status in male, but not female, non-obese adults reporting valid dietary intakes. Int J Obes Relat Metab Disord 22, 105–112.
Dwyer JT, Evans M, Stone EJ, Feldman HA, Lytle L, Hoelscher D et al. (2001). Adolescents' eating patterns influence their nutrient intakes. J Am Diet Assoc 101, 798–802.
Elfhag K, Rossner S (2005). Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev 6, 67–85.
Fábry P, Hejl Z, Fodor J, Braun T, Zvolánkov á K (1964). The frequency of meals. Its relation to overweight, hypercholesterolemia and decreased glucose-tolerance. Lancet 2, 614–615.
Farshchi HR, Taylor MA, Macdonald IA (2004). Regular meal frequency creates more appropriate insulin sensitivity and lipid profiles compared with irregular meal frequency in healthy lean women. Eur J Clin Nutr 58, 1071–1077.
Farshchi HR, Taylor MA, Macdonald IA (2005). Beneficial metabolic effects of regular meal frequency on dietary thermogenesis, insulin sensitivity, and fasting lipid profiles in healthy obese women. Am J Clin Nutr 81, 16–24.
Garrow JS, Durrant M, Blaza S, Wilkins D, Royston P, Sunkin S (1981). The effect of meal frequency and protein concentration on the composition of the weight lost by obese subjects. Br J Nutr 45, 5–15.
Glenny AM, O'Meara S, Melville A, Sheldon TA, Wilson C (1997). The treatment and prevention of obesity: a systematic review of the literature. Int J Obes Relat Metab Disord 21, 715–737.
Harris JA, Benedict FG (1919). A Biometric Study of Basal Metabolism in Man. The Carnegie Institute: Washington DC.
Heshka S, Anderson JW, Atkinson RL, Greenway FL, Hill JO, Phinney SD et al. (2003). Weight loss with self-help compared with a structured commercial program: a randomized trial. JAMA 289, 1792–1798.
Inelmen EM, Toffanello ED, Enzi G, Gasparini G, Miotto F, Sergi G et al. (2005). Predictors of drop-out in overweight and obese outpatients. Int J Obes Relat Metab Disord 29, 122–128.
Jebb SA (2005). Dietary strategies for the prevention of obesity. Proc Nutr Soc 64, 217–227.
Jenkins DJA, Ocana A, Jenkins AL, Wolever TMS, Vuksan V, Katzman L et al. (1992). Metabolic advantages of spreading the nutrient load: effects of increased meal frequency in non-insulin-dependent diabetes. Am J Clin Nutr 55, 461–467.
Jenkins DJA, Wolever TMS, Vuksan V, Brighenti F, Cunnane SC, Venketeshwer R et al. (1989). Nibbling versus gorging: metabolic advantages of increased meal frequency. N Eng J Med 321, 929–934.
Kayman S, Bruvold W, Stern JS (1990). Maintenance and relapse after weight loss in women: behavioral aspects. Am J Clin Nutr 52, 800–807.
King S, Gibney M (1999). Dietary advice to reduce fat intake is more successful when it does not restrict habitual eating patterns. J Am Diet Assoc 99, 685–689.
Kirk TR (2000). Role of dietary carbohydrate and frequent eating in body-weight control. Proc Nutr Soc 59, 349–358.
Lantz H, Peltonen M, Agren L, Torgerson JS (2003a). A dietary and behavioural programme for the treatment of obesity. A 4-year clinical trial and a long-term posttreatment follow-up. J Intern Med 254, 272–279.
Lantz H, Peltonen M, Agren L, Torgerson JS (2003b). Intermittent versus on-demand use of a very low calorie diet: a randomized 2-year clinical trial. J Intern Med 253, 463–471.
Larsson I, Lissner L, Näslund N, Lindroos AK (2004). Leisure and occupational physical activity in relation to body mass index in men and women. Scand J Nutr 48, 165–172.
Levitsky DA, Halbmaier CA, Mrdjenovic G (2004). The freshman weight gain: a model for the study of the epidemic of obesity. Int J Obes Relat Metab Disord 28, 1435–1442.
Lindroos AK, Sjöström L, Lissner L (1993). Validity and reproducibility of a self-administered dietary questionnaire in obese and nonobese subjects. Eur J Clin Nutr 47, 461–481.
Livsmedelsverket (1997). Svenska Näringsrekommendationer PO Box 622, S-751 26 Uppsala: Sweden.
Livsmedelsverket (2005). Svenska näringsrekommendationer 2005 PO Box 622, S-751 26 Uppsala: Sweden.
Marmonier C, Chapelot D, Fantino M, Louis-Sylvestre J (2002). Snacks consumed in a nonhungry state have poor satiating efficiency: influence of snack composition on substrate utilization and hunger. Am J Clin Nutr 76, 518–528.
Mattson MP (2005). The need for controlled studies of the effects of meal frequency on health. Lancet 365, 1978–1980.
McGrath SA, Gibney MJ (1994). The effects of altered frequency of eating on plasma lipids in free-living healthy males on normal self-selected diets. Eur J Clin Nutr 48, 402–407.
Murphy MC, Chapman C, Lovegrove J, Isherwood SG, Morgan LM, Wright JW et al. (1996). Meal frequency; does it determine postprandial lipaemia? Eur j Clin Nutr 50, 491–497.
NIH (1998). Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. National Institutes of Health. Obes Res 6 (Suppl 2), 51S–209S.
Parks EJ, McCrory MA (2005). When to eat and how often? Am J Clin Nutr 81, 3–4.
Samaha FF, Iqbal N, Seshadri P, Chicano KL, Daily DA, McGrory J et al. (2003). A low-carbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med 348, 2074–2081.
SBU Statens beredning för medicinsk utvärdering (2002). Fetma—problem och åtgärder. En systematisk litteraturöversikt: Göteborg.
Speechly DP, Rogers GG, Buffenstein R (1999). Acute appetite reduction associated with an increased frequency of eating in obese males. Int J Obes Relat Metab Disord 23, 1151–1159.
Thomsen C, Christiansen C, Rasmussen OW, Hermansen K (1997). Comparison of the effects of two weeks' intervention with different meal frequencies on glucose metabolism, insulin sensitivity and lipid levels in non-insulin-dependent diabetic patients. Ann Nutr Metab 41, 173–180.
Titan SM, Bingham S, Welch A, Luben R, Oakes S, Day N et al. (2001). Frequency of eating and concentrations of serum cholesterol in the Norfolk population of the European prospective investigation into cancer (EPIC-Norfolk): cross sectional study. BMJ 323, 1286–1288.
Torgerson JS, Agren L, Sjostrom L (1999). Effects on body weight of strict or liberal adherence to an initial period of VLCD treatment. A randomised, one-year clinical trial of obese subjects. Int J Obes Relat Metab Disord 23, 190–197.
Verboeket-van de Venne WP, Westerterp KR (1993). Frequency of feeding, weight reduction and energy metabolism. Int J Obes Relat Metab Disord 17, 31–36.
Wadden T, Stunkard A (2002). Handbook of Obesity Treatment. The Guildford Press: New York. pp 191.
WHO (2003). Diet, Nutrition and the Prevention of Chronic Diseases World Health Organ Tech Rep Ser, Vol. 916, pp. i–viii, 1–149, backcover.
Wing RR, Jeffery RW, Burton LR, Thorson C, Nissinoff KS, Baxter JE (1996). Food provision vs structured meal plans in the behavioral treatment of obesity. Int J Obes Relat Metab Disord 20, 56–62.
Zizza C, Siega-Riz A-M, Popkin BM (2001). Significant increase in young adults snacking between 1977–1978 and 1994–1996 represent a cause for concern!. Prev Med 32, 303–310.
Acknowledgements
We thank Ted Lystig for statistical advice. This study was supported by a grant from Västra Götalandsregionen.
Author information
Authors and Affiliations
Corresponding author
Additional information
Contributors: HBF initiated, designed and conducted the study, collected the data, did the statistical analysis and wrote the paper. SK, HH and ML collected the data, participated in the discussion of results and reviewed the paper. JT and AKL participated in the study design, the discussion of the results and reviewed the paper.
Rights and permissions
About this article
Cite this article
Bertéus Forslund, H., Klingström, S., Hagberg, H. et al. Should snacks be recommended in obesity treatment? a 1-year randomized clinical trial. Eur J Clin Nutr 62, 1308–1317 (2008). https://doi.org/10.1038/sj.ejcn.1602860
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602860
Keywords
This article is cited by
-
The effects of eating frequency on changes in body composition and cardiometabolic health in adults: a systematic review with meta-analysis of randomized trials
International Journal of Behavioral Nutrition and Physical Activity (2023)
-
Effect of meal frequency on glucose and insulin levels in women with polycystic ovary syndrome: a randomised trial
European Journal of Clinical Nutrition (2016)
-
The Influence of Portion Size and Timing of Meals on Weight Balance and Obesity
Current Obesity Reports (2015)
-
Eating frequency, energy intake and body weight during a successful weight loss trial in overweight and obese postpartum women
European Journal of Clinical Nutrition (2014)
-
Eating frequency is inversely associated with blood pressure and hypertension in Korean adults: analysis of the Third Korean National Health and Nutrition Examination Survey
European Journal of Clinical Nutrition (2014)