Abstract
Background/Objective:
Carboxylic acids (CAs), especially butyric acid, have been suggested to counteract colonic diseases, such as ulcerative colitis and colon cancer. Colonic formation of CAs can be influenced by the diet, but the concentrations and pattern formed need to be evaluated for different food products in humans. To elucidate how the colonic concentration of CAs in healthy subjects is influenced by dietary supplementation with oat bran, and whether the concentration varies over time and during consecutive days.
Subjects/Methods:
Twenty-five healthy subjects (age 24±1.3) were recruited to the study. The subjects were given 40 g β-glucan enriched oat bran per day, corresponding to 20 g dietary fibre, in 4 slices of bread. CAs were analysed in faeces during three consecutive days after 0, 4, 8 and 12 weeks on this diet.
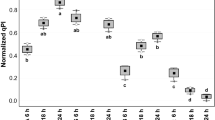
Results:
The concentration of acetic, propionic, butyric, isobutyric and isovaleric acid was higher (P<0.05–0.001) after 8 weeks on the oat bran diet as compared with values at entry, whereas that of lactic acid was lower (P<0.05). After 12 weeks, the concentrations of acetic, propionic and isobutyric acid were still higher and that of lactic acid lower. The variation between individuals was considerable, whereas in the same individuals there was little variation.
Conclusions:
Oat bran increased the faecal concentration of CAs after 8 weeks, indicating an increased concentration also in the distal colon. The concentration of all main acids increased, except for lactic acid, which decreased. Oat bran may therefore have a preventive potential adjunct to colonic diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Berggren AM, Björck IME, Nyman EMGL, Eggum BO (1993). Short-chain fatty-acid content and pH in cecum of rats given various sources of carbohydrates. J Sci Food Agric 63, 397–406.
Bird AR, Hayakawa T, Marsono Y, Gooden JM, Record IR, Correll RL et al. (2000). Coarse brown rice increases fecal and large bowel short-chain fatty acids and starch but lowers calcium in the large bowel of pigs. J Nutr 130, 1780–1787.
Bourriaud C, Robins RJ, Martin L, Kozlowski F, Tenailleau E, Cherbut C et al. (2005). Lactate is mainly fermented to butyrate by human intestinal microfloras but inter-individual variation is evident. J Appl Microbiol 99, 201–212.
Brown I, Warhurst M, Arcot J, Playne M, Illman RJ, Topping DL (1997). Fecal numbers of bifidobacteria are higher in pigs fed Bifidobacterium longum with a high amylose cornstarch than with a low amylose cornstarch. J Nutr 127, 1822–1827.
Bullock NR, Booth JC, Gibson GR (2004). Comparative composition of bacteria in the human intestinal microflora during remission and active ulcerative colitis. Curr Issues Intest Microbiol 5, 59–64.
Casterline JL, Oles CJ, Ku Y (1997). In vitro fermentation of various food fiber fractions. J Agric Food Chem 45, 2463–2467.
Chapman MA, Grahn MF, Boyle MA, Hutton M, Rogers J, Williams NS (1994). Butyrate oxidation is impaired in the colonic mucosa of sufferers of quiescent ulcerative colitis. Gut 35, 73–76.
Cummings J (1995). The Large Intestine in Nutrition and Disease. Institut Danone: Bruxelles.
Cummings JH (1997). Short-chain fatty acid enemas in the treatment of distal ulcerative colitis. Eur J Gastroenterol Hepatol 9, 149–153.
Den Hond E, Hiele M, Evenepoel P, Peeters M, Ghoos Y, Rutgeerts P (1998). In vivo butyrate metabolism and colonic permeability in extensive ulcerative colitis. Gastroenterology 115, 584–590.
Di Sabatino A, Morera R, Ciccocioppo R, Cazzola P, Gotti S, Tinozzi FP et al. (2005). Oral butyrate for mildly to moderately active Crohn's disease. Aliment Pharmacol Ther 22, 789–794.
Djouzi Z, Andrieux C (1997). Compared effects of three oligosaccharides on metabolism of intestinal microflora in rats inoculated with a human faecal flora. Br J Nutr 78, 313–324.
Galvez J, Rodriguez-Cabezas ME, Zarzuelo A (2005). Effects of dietary fiber on inflammatory bowel disease. Mol Nutr Food Res 49, 601–608.
Hallert C, Björck I, Nyman M, Pousette A, Granno C, Svensson H (2003). Increasing fecal butyrate in ulcerative colitis patients by diet: controlled pilot study. Inflamm Bowel Dis 9, 116–121.
Hanauer SB (2004). Update on the etiology, pathogenesis and diagnosis of ulcerative colitis. Nat Clin Pract Gastroenterol Hepatol 1, 26–31.
Henningsson AM, Björck IM, Nyman EM (2002). Combinations of indigestible carbohydrates affect short-chain fatty acid formation in the hindgut of rats. J Nutr 132, 3098–3104.
Henningsson AM, Nyman MEGL, Björck IM (2003). Influences of dietary adaptation and source of resistant starch on short-chain fatty acids in the hindgut of rats. Br J Nutr 89, 319–328.
Jenkins DJ, Kendall CW, Popovich DG, Vidgen E, Mehling CC, Vuksan V et al. (2001). Effect of a very-high-fiber vegetable, fruit, and nut diet on serum lipids and colonic function. Metabolism 50, 494–503.
Karppinen S, Liukkonen K, Aura AM, Forssell P, Poutanen K (2000). In vitro fermentation of polysaccharides of rye, wheat and oat brans and inulin by human faecal bacteria. J Sci Food Agric 80, 1469–1476.
Lambo-Fodje AM, Öste R, Nyman ME (2006). Short-chain fatty acid formation in the hindgut of rats fed native and fermented oat fibre concentrates. Br J Nutr 96, 47–55.
Luhrs H, Gerke T, Muller JG, Melcher R, Schauber J, Boxberge F et al. (2002). Butyrate inhibits NF-kappaB activation in lamina propria macrophages of patients with ulcerative colitis. Scand J Gastroenterol 37, 458–466.
Macfarlane GT, Cummings JH (1991). The colonic flora, fermentation, and large bowel digestive function. In: Phillips SF (ed). The Large Intestine: Physiology, Pathophysiology, and Disease. Raven Press, Ltd.: pp 51–92.
McCleary BV, Codd R (1991). Measurement of (1-3),(1-4)-beta-D-glucan in barley and oats – a streamlined enzymatic procedure. J Sci Food Agric 55, 303–312.
McIntyre A, Gibson PR, Young GP (1993). Butyrate production from dietary fibre and protection against large bowel cancer in a rat model. Gut 34, 386–391.
Menzel T, Luhrs H, Zirlik S, Schauber J, Kudlich T, Gerke T et al. (2004). Butyrate inhibits leukocyte adhesion to endothelial cells via modulation of VCAM-1. Inflamm Bowel Dis 10, 122–128.
Nilsson U, Nyman M (2005). Short-chain fatty acid formation in the hindgut of rats fed oligosaccharides varying in monomeric composition, degree of polymerisation and solubility. Br J Nutr 94, 705–713.
Nilsson U, Nyman M, Ahrne S, Sullivan EO, Fitzgerald G (2006). Bifidobacterium lactis Bb-12 and Lactobacillus salivarius UCC500 modify carboxylic acid formation in the hindgut of rats given pectin, inulin, and lactitol. J Nutr 136, 2175–2180.
Pryde SE, Duncan SH, Hold GL, Stewart CS, Flint HJ (2002). The microbiology of butyrate formation in the human colon. FEMS Microbiol Lett 217, 133–139.
Reddy BS, Hirose Y, Cohen LA, Simi B, Cooma I, Rao CV (2000). Preventive potential of wheat bran fractions against experimental colon carcinogenesis: implications for human colon cancer prevention. Cancer Res 60, 4792–4797.
Richardson AJ, Calder AG, Stewart CS, Smith A (1989). Simultaneous determination of volatile and non-volatile acidic fermentation products of anaerobes by capillary gas-chromatography. Lett Appl Microbiol 9, 5–8.
Roland N, Nugon-Baudon L, Andrieux C, Szylit O (1995). Comparative study of the fermentative characteristics of inulin and different types of fibre in rats inoculated with a human whole faecal flora. Br J Nutr 74, 239–249.
Scheppach W (1996). Treatment of distal ulcerative colitis with short-chain fatty acid enemas. A placebo-controlled trial. German-Austrian SCFA Study Group. Dig Dis Sci 41, 2254–2259.
Scheppach W, Bartram HP, Richter F (1995). Role of short-chain fatty acids in the prevention of colorectal cancer. Eur J Cancer 31A, 1077–1080.
Scheppach W, Sommer H, Kirchner T, Paganelli GM, Bartram P, Christl S et al. (1992). Effect of butyrate enemas on the colonic mucosa in distal ulcerative colitis. Gastroenterology 103, 51–56.
Simpson EJ, Chapman MA, Dawson J, Berry D, Macdonald IA, Cole A (2000). In vivo measurement of colonic butyrate metabolism in patients with quiescent ulcerative colitis. Gut 46, 73–77.
Smith JG, Yokoyama WH, German JB (1998). Butyric acid from the diet: actions at the level of gene expression. Crit Rev Food Sci Nutr 38, 259–297.
Soergel KH, Harig JM, Loo FD, Ramaswamy K, Wood CM (1989). Colonic fermentation and absorption of SCFA in man. Acta Vet Scand Suppl 86, 107–115.
Steinhart AH, Hiruki T, Brzezinski A, Baker JP (1996). Treatment of left-sided ulcerative colitis with butyrate enemas: a controlled trial. Aliment Pharmacol Ther 10, 729–736.
Vernia P, Annese V, Bresci G, d'Albasio G, D'Inca R, Giaccari S et al. (2003). Topical butyrate improves efficacy of 5-ASA in refractory distal ulcerative colitis: results of a multicentre trial. Eur J Clin Invest 33, 244–248.
Vernia P, Caprilli R, Latella G, Barbetti F, Magliocca FM, Cittadini M (1988). Fecal lactate and ulcerative colitis. Gastroenterology 95, 1564–1568.
Wong JM, de Souza R, Kendall CW, Emam A, Jenkins DJ (2006). Colonic health: fermentation and short chain fatty acids. J Clin Gastroenterol 40, 235–243.
Wood PJ (2004). Relationships between solution properties of cereal beta-glucans and physiological effects – a review. Trends Food Sci Technol 15, 313–320.
Zoran DL, Turner ND, Taddeo SS, Chapkin RS, Lupton JR (1997). Wheat bran diet reduces tumor incidence in a rat model of colon cancer independent of effects on distal luminal butyrate concentrations. J Nutr 127, 2217–2225.
Acknowledgements
We thank Kjell Damstedt, Cerealia RD for baking the bread and dietician Ulrika Koppers-Watting for help with the diet registration. This study was financially supported by the VL- and SL-foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Contributors: ÅN, IB and MN contributed to the conception and the design of the study and critically revising the paper. MJ contributed to the design of the study, the analyses and critically revising the paper. UN supervised all the analyses, did the interpretation of the data and was responsible for writing the paper.
Rights and permissions
About this article
Cite this article
Nilsson, U., Johansson, M., Nilsson, Å. et al. Dietary supplementation with β-glucan enriched oat bran increases faecal concentration of carboxylic acids in healthy subjects. Eur J Clin Nutr 62, 978–984 (2008). https://doi.org/10.1038/sj.ejcn.1602816
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602816
Keywords
This article is cited by
-
Surface glycan-binding proteins are essential for cereal beta-glucan utilization by the human gut symbiont Bacteroides ovatus
Cellular and Molecular Life Sciences (2019)
-
Bacterial communities and metabolic activity of faecal cultures from equol producer and non-producer menopausal women under treatment with soy isoflavones
BMC Microbiology (2017)
-
Identification of weak and gender specific effects in a short 3 weeks intervention study using barley and oat mixed linkage β-glucan dietary supplements: a human fecal metabolome study by GC-MS
Metabolomics (2017)
-
Development and characterization of an oat TILLING-population and identification of mutations in lignin and β-glucan biosynthesis genes
BMC Plant Biology (2010)