Abstract
Objective:
To define the clinical measures of obesity that best predict all cause mortality and cardiovascular disease (CVD) mortality.
Design and Setting:
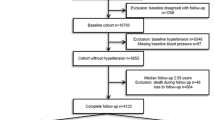
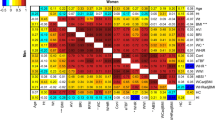
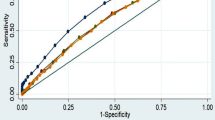
Eleven-year mortality follow-up of an Australian urban population sample of 9309 adults aged 20–69 years in 1989. Baseline measures of obesity included body mass index (BMI), waist circumference (WC), waist-to-stature ratio and the waist-to-hip ratio. The age-standardized hazard ratios for mortality were calculated for 1 s.d. above the mean for each measure of obesity using Cox regression analysis. We constructed receiver operator characteristic (ROC) curves to assess sensitivity and specificity of the measures and to identify approximate cut-points for the prediction of risk.
Results:
Waist-to-hip ratio was superior by magnitude and significance in predicting all cause mortality (male hazard ratio 1.25, P=0.003, female hazard ratio 1.24, P=0.003) and CVD mortality (male hazard ratio 1.62, P<0.001, female hazard ratio 1.59, P<0.001). Waist-to-stature ratio and WC were highly significant but less powerful predictors for CVD mortality. ROC analysis showed higher ‘area under the curve’ values for waist-related measures in males, with similar less marked trends in females. The ROC cut-points yielded values that corresponded to current promulgated criteria.
Conclusions:
The waist-to-hip ratio is the preferred clinical measure of obesity for predicting all cause and CVD mortality. WC is a practical alternative. Waist-to-stature ratio is not more useful than WC alone.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Bennett SA, Magnus P (1994). Trends in cardiovascular risk factors in Australia: results from the National Heart Foundation's Risk Factor Prevalence Study 1980–1989. Med J Aust 161, 519–527.
Boyle CA, Dobson AJ, Egger G, Bennett SA (1993). Waist-to-hip ratios in Australia: a different picture of obesity. Aust J Nutr Diet 50, 57–64.
Calle EF, Thun MJ, Petrelli JM, Rodriguez C, Heath CW (1999). Body mass index and mortality in a prospective cohort of US adults. N Engl J Med 341, 1097–1115.
Dagenais GR, Yi Q, Mann JFE, Pogue J, Yusuf S (2005). Prognostic impact of body weight and abdominal obesity in women and men with cardiovascular disease. Am Heart J 149, 54–60.
Desprès J-P, Lemieux I, Prud'homme D (2001). Treatment of obesity: need to focus on high-risk abdominally obese patients. BMJ 322, 716–720.
Executive summary of the third report of the national cholesterol education program (2001). Expert panel on detection evaluation and treatment of high blood cholesterol in adults. JAMA 285, 2486–2497.
Haijian-Tilaki KO (1997). Sampling Variability of nonparametric estimates of the areas under Receiver Operating Characteristic Curves: an update. Acade Radiol 4, 49–58.
Han TS, Seidell JC, Currall JE, Morrison Ce, Deurenberg P, Lean ME (1997). The influences of height and age on waist circumference as an index of adiposity in adults. Int J Obes 21, 83–89.
Heitmann BL, Frederiksen P, Lissner L (2004). Hip circumference and cardiovascular morbidity and mortality in men and women. Obes Res 12, 482–487.
Ho S-Y, Lam T-H, Janus ED, Hong Kong Cardiovascular Risk Factor Prevalence Study Steering Committee (2003). Waist-to-stature ratio is more strongly associated with cardiovascular risk factors than other simple anthropometric indices. Ann Epidemiol 13, 683–691.
Hu G, Tuomilehto J, Silventoinen K, Barengo N, Jousilahti P (2004). Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur Hea J 25, 2212–2219.
International Diabetes Federation (2005). The IDF consensus worldwide definition of the metabolic syndrome Available from http://www.idf.orgaccessed June 2005.
Larsson B, Bengtsson C, Bjorntorp P, Lapidus L, Sjostrom L, Svardsudd K et al. (1992). Is abdominal body fat distribution a major explanation for the sex difference in the incidence of myocardial infarction? The study of men born in 1913 and the study of women, Goteborg, Sweden. Am J Epidemiol 135, 266–273.
Lean MEJ, Han TS, Morrison CE (1995). Waist circumference as a measure for indicating need for weight management. BMJ 311, 158–161.
McGee DL, the Diverse Populations Collaboration (2005). Body mass index and mortality: a meta-analysis based on personal level data from 26 observational studies. Ann Epidemiol 15, 87–97.
Mokdad AH, Marks JS, Stroup DF, Gerberding JL (2004). Actual causes of death in the United States. JAMA 291, 1238–1245.
Molarius A, Seidell JC (1998). Selection of anthropometric indicators for classification of abdominal fatness – a critical review. Int J Obes 22, 719–727.
Rexrode KM, Carey VJ, Hennekeus CH, Walters EE, Colditz GA, Stampfer MJ et al. (1998). Abdominal adiposity and coronary heart disease in women. JAMA 280, 1843–1848.
Schisterman Ef, Perkins NJ, Liu A, Bondell H (2005). Optimal cut-point and its corresponding Youden Index to discriminate individuals using pooled blood samples. Epidemiology 16, 73–81.
Van der Kooy, Leenan R, Seidell JC, Deurenberg P, Hautvast GAG (1993). Effect of a weight cycle on visceral fat accumulation. Am J Clin Nutr 58, 853–857.
Welborn TA, Dhaliwal SS, Bennett SA (2003). Waist-hip ratio is the dominant risk factor predicting cardiovascular deaths in Australia. Med J Aust 179, 580–585.
World Health Organisation (1977). International classification of diseases Manual of the international statistical classification of diseases, injuries, and causes of death, 9th revision (ICD-9). Geneva:WHO.
World Health Organisation (1998). International classification of diseases. Manual of the international statistical classification of diseases, injuries, and causes of death, 10th revision (ICD-10). Geneva:WHO.
World Health Organisation (1998). Obesity: preventing and managing the global epidemic. Report of a WHO consultation on obesity. WHO: Geneva.
Yusuf S, Hawken S, Öunpuu S, On behalf of the INTERHEART Study Investigators (2005). Obesity and the risk of myocardial infarction in 27 000 participants from 52 countries: a case–control study. Lancet 366, 1640–1649.
Acknowledgements
We are indebted to the National Heart Foundation of Australia for permission to use data from the 1989 Risk Factor Prevalence Survey and to the officers of the Australian Institute of Health and Welfare who linked the survey data to the National Death Index; Stan Bennett, Gabrielle Hodgson, Robert Vanderhoek, Paul Jelfs, Tracy Dixon and John Harding. The initial study was supported by Healthway, the Western Australian Health Promotion Foundation, and this analysis was funded with the assistance of a grant-in-aid provided by Merck, Sharp and Dohme (Australia) Pty Ltd.
Dr Welborn reports receiving consulting fees and conference support from Abbott Australasia, Roche Products Pty Ltd and Sanofi–Aventis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guarantor: TA Welborn.
Rights and permissions
About this article
Cite this article
Welborn, T., Dhaliwal, S. Preferred clinical measures of central obesity for predicting mortality. Eur J Clin Nutr 61, 1373–1379 (2007). https://doi.org/10.1038/sj.ejcn.1602656
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602656
Keywords
This article is cited by
-
Relationships between obesity and functional outcome after ischemic stroke: a Mendelian randomization study
Neurological Sciences (2024)
-
Waist to height ratio as a simple tool for predicting mortality: a systematic review and meta-analysis
International Journal of Obesity (2023)
-
Associations of five obesity indicators with cognitive performance in 30,697 Taiwan Biobank participants
BMC Geriatrics (2022)
-
The Impact of Obesity on Sudden Cardiac Death Risk
Current Cardiology Reports (2022)
-
Correlation of staging and risk factors with cardiovascular autonomic neuropathy in patients with type II diabetes mellitus
Scientific Reports (2021)