Abstract
Objectives:
To determine and compare the gastrointestinal (GI) responses of young adults following consumption of 45 g sucrose, 20, 35 and 50 g xylitol or erythritol given as a single oral, bolus dose in a liquid.
Design:
The study was a randomized, double-blind, placebo-controlled study.
Subjects:
Seventy healthy adult volunteers aged 18–24 years were recruited from the student population of the University of Salford. Sixty-four subjects completed the study.
Interventions:
Subjects consumed at home without supervision and in random order, either 45 g sucrose or 20, 35 and 50 g erythritol or xylitol in water on individual test days, while maintaining their normal diet. Test days were separated by 7-day washout periods. Subjects reported the prevalence and magnitude of flatulence, borborygmi, bloating, colic, bowel movements and the passage of faeces of an abnormally watery consistency.
Results:
Compared with 45 g sucrose, consumption of a single oral, bolus dose of 50 g xylitol in water significantly increased the number of subjects reporting nausea (P<0.01), bloating (P<0.05), borborygmi (P<0.005), colic (P<0.05), watery faeces (P<0.05) and total bowel movement frequency (P<0.01). Also 35 g of xylitol increased significantly bowel movement frequency to pass watery faeces (P<0.05). In contrast, 50 g erythritol only significantly increased the number of subjects reporting nausea (P<0.01) and borborygmi (P<0.05). Lower doses of 20 and 35 g erythritol did not provoke a significant increase in GI symptoms. At all levels of intake, xylitol produced significantly more watery faeces than erythritol: resp. 50 g xylitol vs 35 g erythritol (P<0.001), 50 g xylitol vs 20 g erythritol (P<0.001) and 35 g xylitol vs 20 g erythritol (P<0.05).
Conclusions:
When consumed in water, 35 and 50 g xylitol was associated with significant intestinal symptom scores and watery faeces, compared to the sucrose control, whereas at all levels studied erythritol scored significantly less symptoms. Consumption of 20 and 35 g erythritol by healthy volunteers, in a liquid, is tolerated well, without any symptoms. At the highest level of erythritol intake (50 g), only a significant increase in borborygmi and nausea was observed, whereas xylitol intake at this level induced a significant increase in watery faeces.
Sponsorship:
Cerestar R&D Center, Vilvoorde, Belgium.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Arrigoni E, Brouns F, Amadò R (2005). Human gut microbiota does not ferment erythritol. Br J Nutr 94, 643–646.
Asano T, Levitt MD, Goeth FC (1973). Xylitol absorption in healthy men. Diabetes 22, 279–281.
Beaugerie L, Flourié B, Pellier P, Achour L, Franchisseur C, Rambaud JC (1991). Tolerance clinique, absorption intestinale et valeur energetique de quatre polyols pris a jeun. Gastroentérol Clin Biol 15, 929–932.
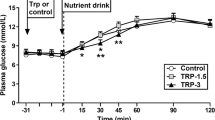
Bornet FRJ, Blayo A, Dauchy F, Slama G (1996a). Plasma and urine kinetics of erythritol after oral ingestion by healthy humans. Regulat Toxicol Pharmacol 24, S280–S285.
Bornet FRJ, Blayo A, Dauchy F, Slama G (1996b). Gastrointestinal response and plasma urine determinations in human subjects given erythritol. Regulat Toxicol Pharmacol 24, S296–S302.
Bornet FRJ, Dauchy F, Chevalier A, Slama G (1992). Etude du devenir metabolique, après ingestion chez l’homme sain, d’un nouvel edulcorant de charge basse calorie: l’ erythritol. Gastroenterol Clin Biol 16, A169.
Culbert SJ, Wang YM, Fritsche HA, Carr D, Lantin E, van Eys J (1986). Oral xylitol in American adults. Nutr Res 6, 913–922.
Cummings JH, Lee A, Storey D (2001). Workshop: physiology and tolerance of LDCs. Br J Nutr 85, S59–S60.
De Cock P (1999). Erythritol: a novel noncaloric sweetener ingredient. World Rev Nutr Diet 85, 110–116.
De Cock P, Bechert CL (2002). Erythritol. Functionality in noncaloric functional beverages. Pure Appl Chem 74, 1281–1289.
Dubach UC, Feiner E, Forgo I (1969). Orale verträglichkeit von xylit bei stoffwechselgesunden versuchspersonen. Schweiz Med Wochenschr 99, 190.
Dwivedi BK (1978). Food products for special dietary needs. In: Dwivedi BK (ed). Low Calorie and Special Dietary Foods. CRC Press: West Palm Beach, FL, pp 1–22.
Goosens J, Röper H (1994). Erythritol: a new sweetener. Food Sci Technol Today 8, 144–149.
Hiele M, Ghoos Y, Rutgeerts P, Vantrappen G (1993). Metabolism of erythritol in humans: comparison with glucose and lactitol. Br J Nutr 69, 169–176.
Ishikawa M, Miyashita M, Kawashima Y, Nakamura T, Saitou N, Modderman J (1996). Effects of oral administration of erythritol on patients with diabetes. Regulat Toxicol Pharmacol 24, S303–S308.
Kanwanabe J, Hirasawa M, Takeuchi T, Oda T, Ikeda T (1992). Noncariogenicity of erythritol as a substrate. Caries Res 26, 358–362.
Lanthier PL, Morgan MY (1985). Lactitol in the treatment of chronic hepatic encephalopathy: an open comparison with lactulose. Gut 26, 415–420.
Lederle FA, Busch DL, Mattox KM, West MJ, Aske DM (1990). Cost-effective treatment of constipation in the elderly: a randomized double-blind comparison of sorbitol and lactulose. Am J Med 89, 597–601.
Lee A, Storey DM (1999). Comparative gastrointestinal tolerance of sucrose, lactitol, or D-tagatose in chocolate. Regulat Toxicol Pharmacol 29, S78–S82.
Lee A, Storey DM, Zumbe A (1994). Breath hydrogen after ingestion of the bulk sweeteners sorbitol, isomalt and sucrose in chocolate. Br J Nutr 71, 731–737.
Livesey G (1992). Energy values of dietary fibre and sugar alcohols for man. Nutr Res Rev 5, 61–84.
Livesey G (2001). Tolerance of low-digestible carbohydrates: a general view. B J Nutr 85, S7–S16.
Maguire A, Rugg-Gunn J, Wright G (2000). Adaptation of dental plaque to metabolise maltitol compared with other sweeteners. J Dent 28, 51–59.
Marteau P, Flourie B (2001). Tolerance to low-digestible carbohydrates: symptomatology and methods. Br J Nutr 85, S17–S21.
McNemar Q (1947). Note on the sampling error of the difference between correlated proportions or percentages. Psychometrica 12, 153–157.
Munro IC, Bernt WO, Borzelleca JF, Flamm G, Lynch BS, Kennepohl E et al. (1998). Erythritol: an interpretive summary of biochemical, metabolic, toxicological and clinical data. Food Chem Toxicol 36, 1139–1174.
Noda K, Nakayama K, Oku T (1994). Serum glucose and insulin levels and erythritol balance after oral-administration of erythritol in healthy-subjects. Eur J Clin Nutr 48, 286–292.
Oku T, Okazaki M (1996). Laxative threshold of sugar alcohol erythritol in human subjects. Nutr Res 16, 577–589.
Paul AA, Southgate DAT (1978). McCance and Widdowson's The Composition of Foods, 4th edn. HM stationery Office: London.
Pepper T, Ollinger M (1988). Xylitol in sugar-free confections. Food Technol 42, 98–105.
Schiweck H, Ziesenitz SC (1996). Physiological properties of polyols in comparison with easily metabolisable saccharides. In: Grenby TH (ed). Advances in Sweeteners. Blackie Academic and Professional: Glasgow. pp 56–83.
Storey DM, Lee A, Zumbe A (2002). The comparative gastrointestinal response of young children to the ingestion of 25 g sweets containing sucrose or isomalt. Br J Nutr 87, 291–297.
Tetzloff W, Dauchy F, Medimagh S, Carr D, Bar A (1996). Tolerance to subchronic, high dose ingestion of erythritol in human volunteers. Regulat Toxicol Pharmacol 24, S286–S295.
Zumbe A, Brinkworth R (1992). Comparative studies of gastrointestinal tolerance and acceptability of milk chocolate containing either sucrose, isomalt or sorbitol in healthy consumers and type II diabetics. Z Ernahrungswiss 31, 40–48.
Zumbe A, Lee A, Storey D (2001). Polyols in confectionery: the route to sugar-free, reduced sugar and reduced calorie confectionery. Br J Nutr 85, S31–S45.
Acknowledgements
We acknowledge Dr P Scarf (Director, Centre for Operational Research and Applied Statistics at the University of Salford) for initial advice on statistical methodology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Storey, D., Lee, A., Bornet, F. et al. Gastrointestinal tolerance of erythritol and xylitol ingested in a liquid. Eur J Clin Nutr 61, 349–354 (2007). https://doi.org/10.1038/sj.ejcn.1602532
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602532
Keywords
This article is cited by
-
Kinetic study and model of fermentation parameters affected growth and xylitol production in bioreactor by Kluyveromyces marxianus ATCC 36,907
Biomass Conversion and Biorefinery (2023)
-
Experimental replacement of hops by mango in beer: production and comparison of total phenolics, flavonoids, minerals, carbohydrates, proteins and toxic substances
International Journal of System Assurance Engineering and Management (2022)
-
Health benefits of xylitol
Applied Microbiology and Biotechnology (2020)
-
Erythritol reduces small intestinal glucose absorption, increases muscle glucose uptake, improves glucose metabolic enzymes activities and increases expression of Glut-4 and IRS-1 in type 2 diabetic rats
European Journal of Nutrition (2018)
-
Chewing gum for intestinal function recovery after caesarean section: a systematic review and meta-analysis
BMC Pregnancy and Childbirth (2017)