Abstract
Objective:
To explore the independent associations of body height, body mass index (BMI), waist circumference and hip circumference with high-density lipoprotein-cholesterol (HDL-cholesterol) and non-high-density lipoprotein-cholesterol (non-HDL-cholesterol), in a large general population sample.
Design:
Cross sectional.
Setting:
Urban and rural areas throughout Greece.
Subjects:
In total,10 837 volunteers, 2034 men and 8803 women, aged 25–82 years, participants in the European Prospective Investigation into Cancer and Nutrition study (EPIC), who have never smoked and never been treated for dyslipidemia.
Interventions:
None.
Results:
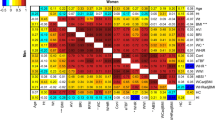
The effect of height on non-HDL-cholesterol was opposite but in absolute terms almost as important as that of BMI with no gender interaction. Among women, hip circumference was inversely associated with non-HDL-cholesterol (standardized coefficient bst=−1.11, with standard error (s.e.)=0.42) and positively with HDL-cholesterol (bst=0.85, s.e.=0.12) whereas, waist circumference was inversely associated with HDL-cholesterol (bst=−1.16, s.e.=0.13) and strongly positively with non-HDL-cholesterol (bst=8.83, s.e.=0.45). Among men, associations were generally weaker (in absolute terms by about 50%) and for hip circumference the association with non-HDL-cholesterol was actually non significantly positive.
Conclusions:
Height was inversely associated with HDL and non-HDL-cholesterol implicating early life phenomena in the regulation of these variables. Larger hip circumference among women had beneficial effects on blood cholesterol fractions by increasing HDL-cholesterol and reducing non-HDL-cholesterol, whereas among men the relevant effects were less clear cut. The detrimental consequences of large waist circumference on both HDL (reduction) and non-HDL-cholesterol (increase) were also particularly marked among women.
Sponsorship:
The European Prospective Investigation into Cancer and Nutrition (EPIC) is coordinated by the International Agency for Research on Cancer (World Health Organization) and supported by the Europe Against Cancer Program of the European Commission. The Greek segment of the EPIC study is also supported by the Greek Ministry of Health and the Greek Ministry of Education. This study was additionally supported by the fellowship ‘Vassilios and Nafsika Tricha’.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Abdu TA, Neary R, Elhadd TA, Akber M, Clayton RN (2001). Coronary risk in growth hormone deficient hypopituitary adults: increased predicted risk is due largely to lipid profile abnormalities. Clin Endocrinol (Oxford) 55, 209–216.
Aronne LJ, Segal KR (2002). Adiposity and fat distribution outcome measures: assessment and clinical implications. Obes Res 10, 14S–21S.
Benetou V, Chloptsios Y, Zavitsanos X, Karalis D, Naska A, Trichopoulou A (2000). Total cholesterol and HDL-cholesterol in relation to socioeconomic status in a sample of 11, 645 Greek adults: the EPIC study in Greece. Scand J Public Health 28, 260–265.
Bergstrom E, Hernell O, Persson LA, Vessby B (1995). Serum lipid values in adolescents are related to family history, infant feeding, and physical growth. Atherosclerosis 117, 1–13.
Billewicz WZ, Thomson AM, Kemsley WFF (1962). Indices of adiposity. Br J Prev Soc Med 16, 183–188.
Brown CD, Higgins M, Donato KA, Rohde FC, Garrison R, Obarzanek E et al. (2000). Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res 8, 605–619.
Carr DB, Utzschneider KM, Hull RL, Kodama K, Retzlaff BM, Brunzell JD et al. (2004). Intra-abdominal Fat is a major determinant of the National Cholesterol Education Program Adult Treatment Panel III Criteria for the metabolic syndrome. Diabetes 53, 2087–2094.
Cianfarani S, Geremia C, Scott CD, Germani D (2002). Growth, IGF system, and cortisol in children with intrauterine growth retardation: is catch-up growth affected by reprogramming of the hypothalamic-pituitary-adrenal axis? Pediatr Res 51, 94–99.
Cruz ML, Wong WW, Mimouni F, Hachey DL, Setchell KD, Klein PD et al. (1994). Effects of infant nutrition on cholesterol synthesis rates. Pediatr Res 35, 135–140.
Cui Y, Blumenthal RS, Flaws JA, Whiteman MK, Langenberg P, Bachorik PS et al. (2001). Non-high-density lipoprotein cholesterol level as a predictor of cardiovascular disease mortality. Arch Intern Med 61, 1413–1419.
Denke MA, Sempos CT, Grundy SM (1993). Excess body weight. An underrecognized contributor to high blood cholesterol levels in white American men. Arch Intern Med 153, 1093–1103.
Denke MA, Sempos CT, Grundy SM (1994). Excess body weight. An underrecognized contributor to dyslipidemia in white American women. Arch Intern Med 154, 401–410.
Despres JP (1994). Dyslipidemia and obesity. Balliere's Clin Endocrinol Metab 8, 629–660.
Despres JP, Lemieux I, Prud’homme D (2001). Treatment of obesity: need to focus on the high risk abdominally obese patients. BMJ 322, 716–720.
Farwell WR, Sesso HD, Buring JE, Gaziano JM (2005). Non-high-density lipoprotein cholesterol as a risk factor for a first non-fatal myocardial infarction. Am J Cardiol 96, 1129–1134.
Forsen T, Eriksson J, Qiao Q, Tervahauta M, Nissinen A, Tuomilehto J (2000). Short stature and coronary heart disease: a 35-year follow-up of the Finnish cohorts of The Seven Countries Study. J Intern Med 248, 326–332.
Frayn KN (2002). Adipose tissue as abuffer for daily lipid flux. Diabetologia 45, 1201–1210.
Gunnell D, Whitley E, Upton MN, McConnachie A, Davey Smith Gand G, Watt CM (2003). Associations of height, leg length, and lung function with cardiovascular risk factors in the Midspan Family Study. J Epidemiol Comm Health 57, 141–146.
Hebert PR, Rich-Edwards JW, Manson JE, Ridker PM, Cook NR, O’Connor GT et al. (1993). Height and incidence of cardiovascular disease in male physicians. Circulation 88, 1437–1443.
Henriksson KM, Lindblad U, Agren B, Nilsson-Ehle P, Rastam L (2001). Associations between body height, body composition and cholesterol levels in middle-aged men. The Coronary Risk Factor study in Southern Sweden (CRISS). Eur J Epidemiol 17, 521–526.
Hu D, Hannah J, Gray RS, Jablonski KA, Henderson JA, Robbins DC et al. (2000a). Effects of obesity and body fat distribution on lipids and lipoproteins in nondiabetic American Indians: the Strong Heart Study. Obes Res 8, 411–421.
Hu FB, Wang B, Chen C, Jin Y, Yang J, Stampfer MJ et al. (2000b). Body mass index and cardiovascular risk factors in a rural Chinese population. Am J Epidemiol 151, 88–97.
Hunter GR, Kekes-Szabo T, Snyder SW, Nicholson C, Nyikos I, Berland L (1997). Fat distribution, physical activity, and cardiovascular risk factors. Med Sci Sports Exerc 29, 362–369.
Innis SM (1985). The role of diet during development on the regulation of adult cholesterol homeostasis. Can J Physiol Pharmacol 63, 557–564.
Kanaya AM, Vittinghoff E, Shlipak MG, Resnick HE, Visser M, Grady D et al. (2003). Association of total and central obesity with mortality in postmenopausal women with coronary heart disease. Am J Epidemiol 158, 1161–1170.
Kannam J, Levy D, Larson M, Wilson P (1994). Short stature and risk for mortality and cardiovascular disease events. The Framingham Heart Study. Circulation 90, 2241–2247.
Khosla T, Lowe CR (1967). Indices of obesity derived from body weight and height. Br J Prev Soc Med 21, 122–128.
Kolacek S, Kapetanovic T, Zimolo A, Luzar V (1993). Early determinants of cardiovascular risk factors in adults. A. Plasma lipids. Acta Paediatr 82, 699–704.
Krahn AD, Manfreda J, Tate RB, Mathewson FA, Cuddy TE (1994). Evidence that height is an independent risk factor for coronary artery disease (the Manitoba Follow-Up Study). Am J Cardiol 74, 398–399.
La Batide-Alanore A, Tregouet DA, Sass C, Siest G, Visvikis S, Tiret L (2003). Family study of the relationship between height and cardiovascular risk factors in the STANISLAS cohort. Int J Epidemiol 32, 607–614.
Lawlor DA, Taylor M, Davey Smith G, Gunnell D, Ebrahim E (2004). Associations of components of adult height with coronary heart disease in postmenopausal women: the British women's heart and health study. Heart 90, 745–749.
Lissner L, Bjorkelund C, Heitmann BL, Seidell JC, Bengtsson C (2001). Larger hip circumference independently predicts health and longevity in a Swedish female cohort. Obes Res 10, 644–646.
Marmot MG, Page CM, Atkins E, Douglas JW (1980). Effect of breast-feeding on plasma cholesterol and weight in young adults. J Epidemiol Community Health 34, 164–167.
National Cholesterol Education Program Expert Panel. Third report of the National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (ATP III) (2001). NIH Publication. National Heart, Lung and Blood Institute: Bethesda, MD.
National Task Force on the Prevention and Treatment of Obesity (2000). Overweight, Obesity, and Health Risk. Arch Intern Med 160, 898–904.
Palmer JR, Rosenberg L, Shapiro S (1990). Stature and the risk of myocardial infarction in women. Am J Epidemiol 132, 27–32.
Parker DR, Lapane KL, Lasater TM, Carleton RA (1998). Short stature and cardiovascular disease among men and women from two southeastern New England communities. Int J Epidemiol 27, 970–975.
Peck AM, Vagero DH (1989). Adult body height, self perceived health and mortality in the Swedish population. J Epidemiol Comm Health 43, 380–384.
Pi-Sunyer FX (2002). The Obesity epidemic: Pathophysiology and consequences of Obesity. Obes Res 10, 97S–104S.
Ravussin E, Smith SR (2002). Increased fat intake, impaired fat oxidation, and failure of fat cell proliferation result in fat storage, insulin resistance, and type 2 diabetes mellitus. Ann N Y Acad Sci 967, 363–378.
Riboli E, Hunt KJ, Slimani N, Ferrari P, Norat T, Fahey M et al. (2002). European Prospective Investigation into Cancer and Nutrition (EPIC) study populations and data collection. Public Health Nutr 5, 1113–1124.
Riboli E, Kaaks R (1997). The EPIC Project: Rationale and Study Design. Intern J Epidemiol 26 (Suppl 1), S6–S14.
Ridker PM, Rifai N, Cook NR, Bradwin G, Buring JE (2005). Non-HDL cholesterol, apolipoproteins A-I and B100, standard lipid measures, lipid ratios, and CRP as risk factors for cardiovascular disease in women. JAMA 294 (3), 326–333.
Rossman I (1977). Anatomic and body composition changes with age. In: Finch CE, Hayflick L (Eds). Handbook of the biology of aging. Van Nostrand Reinhold: New York, pp. 189–221.
Sakai Y, Ito H, Egami Y, Ohoto N, Hijii C, Yanagawa M et al. (2005). Favourable association of leg fat with cardiovascular risk factors. J Intern Med 257, 194–200.
Seidell JC, Pérusse L, Després JP, Bouchard C (2001). Waist and hip circumferences have independent and opposite effects on cardiovascular disease risk factors: the Quebec Family Study. Am J Clin Nutr 74, 315–321.
Shai I, Rimm EB, Hankinson SE, Curhan G, Manson JE, Rifai N et al. (2004). Multivariate assessment of lipid parameters as predictors of coronary heart disease among postmenopausal women: potential implications for clinical guidelines. Circulation 110, 2824–2830.
Sheehan MT, Jensen MD (2000). Metabolic complications of obesity. Pathophysiologic considerations. Med Clin North Am 84, 363–385.
Snijder MB, Zimmet PZ, Visser M, Dekker JM, Seidell JC, Shaw JE (2004a). Independent association of hip circumference with metabolic profile in different ethnic groups. Obes Res 12, 1370–1374.
Snijder MB, Zimmet PZ, Visser M, Dekker JM, Seidell JC, Shaw JE (2004b). Independent and opposite associations of waist and hip circumferences with diabetes, hypertension and dyslipidemia: the AusDiab Study. Int J Obes Relat Metab Disord 28, 402–409.
Svanborg ES, Mellstrom D (1991). Metabolic changes in aging: predictors of diseases. The Swedish experience. In: Ingram DK, Baker GT, Shock NW (Eds). The potential of nutritional modulation of aging. Food and Nutrition Press: Trumbull, CT, pp. 81–90.
Takada D, Ezura Y, Ono S, Iino Y, Katayama Y, Xin Y et al. (2003). Growth hormone receptor variant (L526I) modifies plasma HDL cholesterol phenotype in familial hypercholesterolemia: intra-familial association study in an eight-generation hyperlipidemic kindred. Am J Med Genet A 121, 136–140.
Thomas GN, Ho SY, Lam KS, Janus ED, Hedley AJ, Lam TH, Hong Kong Cardiovascular Risk Factor Prevalence Study Steering Committee (2004). Impact of obesity and body fat distribution on cardiovascular risk factors in Hong Kong Chinese. Obes Res 12, 1805–1813.
Wahrenberg H, Hertel K, Leijonhufvud BM, Persson LG, Toft E, Arner P (2005). Use of waist circumference to predict insulin resistance: retrospective study. BMJ 330, 1363–1364.
Wamala SP, Mittleman MA, Horsten M, Schenck-Gustafsson K, Orth-Gomer K (1999). Short stature and prognosis of coronary heart disease in women. J Intern Med 245, 557–563.
Willett WC, Stampfer MJ (1986). Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 124, 17–24.
Williams MJ, Hunter GR, Kekes-Szabo T, Snyder S, Treuth M (1997). Regional fat distribution in women and risk of cardiovascular disease. Am J Clin Nutr 65, 855–860.
Yarnell JW, Limb ES, Layzell JM, Baker IA (1992). Height: a risk marker for ischaemic heart disease: prospective results from the Caerphilly and Speedwell Heart Disease Studies. Eur Heart J 13, 1602–1605.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guarantor: A Trichopoulou.
Contributors: VB has initiated and implemented this study. CB was the lead biostatistician. DT is consultant epidemiologist. AT is the principal investigator in the Greek EPIC project. All authors have contributed to the drafting of the manuscript and have approved the final version.
Rights and permissions
About this article
Cite this article
Benetou, V., Bamia, C., Trichopoulos, D. et al. Associations of anthropometric characteristics with blood cholesterol fractions among adults. The Greek EPIC study. Eur J Clin Nutr 60, 942–948 (2006). https://doi.org/10.1038/sj.ejcn.1602403
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602403