Abstract
Objective:
To know the prevalence of malnutrition and to validate a nutritional screening protocol (SP) in patients hospitalised in Hospitals representative of inpatients admitted for acute illnesses in Galicia.
Design:
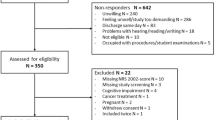
Cross-sectional study of 376 randomised patients (189 female, 210 ⩾65 y old) from 12 public hospitals admitted to hospital for acute medical, surgical or trauma illnesses. The patients elicited were evaluated by a simple SP, including variables relative to recent weight changes, serum albumin, lymphocytes, food ingestion and diagnosis at admission (Cardona's Protocol), and with a diagnostic protocol (DP, Subjective Global Assessment). Both SP and DP were performed by personnel trained in nutritional evaluation. Results of SP and DP were compared; principal factors related to malnutrition were also analysed; statistical significance was considered at P<0.05.
Results:
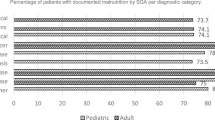
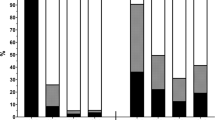
From patients studied, according to DP 169/360 (46.94%), patients presented malnutrition (134 B category and 35C category). SP rate was significantly related to severity of malnutrition detected by DP (P<0.001). The principal factors related to the presence of malnutrition were older age and degree of metabolic stress.
Conclusions:
In adult patients admitted for acute illnesses, the prevalence of protein-energy malnutrition is high. The risk was related to age and to metabolic stress. The risk of malnutrition in a hospital setting is evaluated appropriately by a simple screening procedure that may contribute to detecting and correcting malnutrition risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Alastrué A, Rull M, Campos I, Ginesta C, Mellus MR & Salvá JA (1988): Nuevas normas y consejos en la valoración de los parámetros antropométricos en nuestra población: índice adiposo-muscular, índices ponderales y tablas de percentiles de los datos antropométricos útiles en una valoración nutricional. Med. Clin. (Barc.) 91, 223–236.
Alcok NW (1999): Laboratory tests for assessing nutritional status. In Modern Nutrition in Health and Disease 9th Edition, eds Shils ME, Olson JA, Shike M, Ross AC, pp 923–936. Baltimore: Williams and Wilkins.
Aznarte Padial P, Pareja Rodríguez de Vera A, de la Rubia Nieto A, López Soriano F & Martínez de Guzmán M (2001): Influence of hospitalization on patients following nutritional assessment on admission. Nutr. Hosp. 16, 14–18.
Cardona D (1998): La nutrición artificial y la mejora de la calidad asistencial. Rev. Calidad Assist. 13, 120–135.
Detsky AS, McLaghlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA & Jeejeebhoy KN (1987): What is Subjective Global Assessment of nutritional status? J. Parenter. Enter. Nutr. 11, 8–13.
de Ulíbarri Pérez JI, Picón César MJ, García Benavent E & Mancha Álvarez-Estrada A (2002): Early detection and control of undernourishment in hospitals. Nutr. Hosp. 17, 139–146.
Nagel MR (1991): Nutrition screening: identifying patients at risk for malnutrition. Nutr. Clin. Pract. 6, 151:155.
Esquius M, Schwartz S, López Helín J, Andreu AL & García E (1993): Parámetros antropométricos de referencia en la población anciana. Med. Clin. (Barc.) 100, 692–698.
González Sánchez J, Hernando Cuñado M, Kazemzadeh A, Luna García R, Martínez-Cañavate Montero MJ, Luna García R & Ramos Martínez A (2000): Malnutrición en un servicio de Medicina Interna: influencia de los pacientes procedentes de residencias de ancianos. Ann. Med. Intern. (Madrid) 17, 347–350.
Guigoz Y, Vellas B & Garry PJ (1996): Assessing the nutritional status of the elderly: the Mini Nutritional Assessment as part of the geriatric evaluation. Nutr. Rev. 54, S59–S65.
Kondrup J, Johansen N, Plum LM, Bak L, Hjlund Larsen I, Martinsen A, Andersen JR, Brnthsen H, Bunch E & Lauesen N (2002): Incidence of nutritional risk and causes of inadequate nutritional care in hospitals. Clin. Nutr. 21, 461–468.
Kondrup J, Allison SP, Elia M, Vellas B & Plauth M (2003): ESPEN Guidelines for Nutrition Screening 2002. Clin. Nutr. 22, 415–421.
Kruizenga HM, Wierdsma NJ, Van Bokhorst MAE, Van Der Schueren DE, Hollander HJ, Jonkers-schuitema CF, Van der Heijden E, Melis GC & Van Staveren WA (2003): Screening of nutritional status in The Netherlands. Clin. Nutr. 22, 147–152.
Martínez Olmos MA, Martínez Vázquez MJ, López Sierra A, Morales Gorría MJ, Cal Bouzón S, Castro Núñez I, Del Campo V & Pena González E (2002): Detection of the risk of malnutrition in hospitalized elderly patients. Nutr. Hosp. 17, 22–27.
McWhirter JP & Pennington CR (1994): Incidence and recognition of malnutrition in hospital. BMJ 308, 945–948.
Powewll-Tuck J & Hennessy EM (2003): A comparison of mid upper arm circumference, body mass index and weight loss as indices of undernutrition in acutely hospitalized patients. Clin. Nutr. 22, 307–312.
Roldán JP, Pérez I, Irles JA & Martín R (1985): Malnutrición en pacientes hospitalizados: estudio prospectivo y aleatorio. Nutr. Hosp. 10, 192–198.
The malnutrition prevalence group (2000): Prevalence of malnutrition on admission to four hospitals in England. Clin. Nutr. 19, 191–195.
Thorsdottir I, Eriksen B & Eysteinsdottir S (1999): Nutritional status at submission for dietetic services and screening for malnutrition at admission to hospital. Clin. Nutr. 18, 15–21.
Acknowledgements
This study has been conducted by means of a Grant of the Nutrition and Dietetics Society of Galicia (Beca SONUDIGA 2003). We want to acknowledge all participants in the study for their kind efforts in performing this study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Guarantor: Nutrition and Dietetic Society of Galicia.
Contributors: Nutrition and Dietetic Society of Galicia.
Appendices
Appendix A1

Appendix A2




Rights and permissions
About this article
Cite this article
Olmos, M., Vázquez, M., López, EP. et al. Nutritional status study of inpatients in hospitals of Galicia. Eur J Clin Nutr 59, 938–946 (2005). https://doi.org/10.1038/sj.ejcn.1602157
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602157
Keywords
This article is cited by
-
Burden assessment in caregivers of patients with home artificial nutrition: a need and a challenge
European Journal of Clinical Nutrition (2017)