Abstract
Objective:
To select a probiotic bacteria that would reduce serum lipids in hypercholesterolaemic volunteers.
Design:
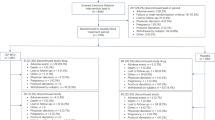
A strain of lactobacillus was selected for its ability to metabolise cholesterol under varying conditions in vitro. Freeze-dried Lactobacillus acidophilus or placebo were then given in a double-blind randomised crossover study to volunteers with high cholesterols.
Subjects:
A total of 80 volunteers with elevated cholesterols.
Interventions:
Volunteers were randomly allocated to receive either two capsules containing freeze-dried L. acidophilus 3 × 1010 CFU or placebo three times a day for 6 weeks. After a 6-week washout period, volunteers were crossed over to another 6 weeks of capsules. Serum lipids were measured at the beginning and end of each interventional period.
Results:
L. acidophilus was able to reduce cholesterol and survive in an acid and bile environment. No changes in anthropomorphic measurements or in dietary records were seen between the baseline and final records or between the two sets of baseline records. There were no changes in serum lipids seen throughout the study.
Conclusion:
Despite the ability in vitro for L. acidophilus to reduce cholesterol, no effect was seen in volunteers.
Sponsorship:
Life-Care Technologies Ltd, Worcestershire.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Agerbaek M, Gerdes LU & Richelsen B (1995): Hypocholesterolaemic effects of a new fermented milk product in healthy middle-aged men. Eur. J. Clin. Nutr. 49, 346–352.
Anderson JW & Gilliland SE (1999): Effect of fermented milk (yogurt) containing Lactobacillus acidophilus L1 on serum cholesterol in hypercholesterolemic humans. J. Am. Coll. Nutr. 18, 43–50.
De Smet I, De Boever P & Verstraete W (1998): Cholesterol lowering in pigs through enhanced bacterial bile hydrolase activity. Br. J. Nutr. 79, 185–194.
Englyst HN, Bingham SA, Runswick SA, Collinson E & Cummings JH (1988): Dietary fibre (non-starch polysaccharides) in fruit, vegetables and nuts. Gastroenterology 1, 247–286.
Englyst HN, Bingham SA, Runswick SA, Collinson E & Cummings JH (1989): Dietary fibre (non-starch polysaccharides) in cereal products. J. Hum. Nutr. Diet. 2, 253–271.
Gilliland SE, Nelson CR & Maxwell C (1985): Assimilation of cholesterol by Lactobacillus acidophilus. Appl. Environ. Microbiol. 49, 377–381.
Hepner G, Fried R, St Jeor S, Fussetti L & Morin R (1979): Hypocholesterolemic effects of yogurt and milk. Am. J. Clin. Nutr. 32, A19–A24.
Klaver FA & Meer RVD (1993): The assumed assimilation of cholesterol by Lactobacilli and Bifidobacterium bifidum is due to their bile salt-deconjugating activity. Appl. Environ. Microbiol. 59, 1120–1124.
Lin SY, Ayres JW, Winkler WJ & Sandine WE (1989): Lactobacillus effects on cholesterol: in vitro and in vivo results. J. Dairy Sci. 72, 2885–2899.
Mann GV (1977): Hypocholesterolaemic effects of milk. Lancet ii, 556.
Massey LK (1984): Effect of changing milk and yogurt consumption on human nutrient intake and serum lipoproteins. J. Dairy Sci. 67, 255–262.
Paul AA & Southgate DAT (1978): McCance and Widdowson's, The Composition of Foods. Amsterdam, New York and Oxford: Elsevier/North-Holland Biomedical Press.
Pereira DI & Gibson GR (2002): Effects of consumption of probiotics and prebiotics on serum lipid levels in humans. Crit. Rev. Biochem. Mol. Biol. 37, 259–281.
Richelsen B, Kristensen K & Pedersen SB (1996): Long-term (6 months) effect of a new fermented milk product on the level of plasma lipoproteins—a placebo controlled and double blind study. Eur. J. Clin. Nutr. 50, 811–813.
Rossouw JE, Burger EM, Van De Vyver P & Ferreira J (1981): The effect of skim milk, yogurt, and full cream milk on human subjects. Am. J. Clin. Nutr. 34, A351–A356.
Schaafsma G, Meuling WJ, Dokkum W & Bouley C (1998): Effects of a milk prodict, fermented by Lactobacillus acidophilus and with fructo-oligosaccharides added, on blood lipids in male volunteers. Eur. J. Clin. Nutr. 52, 436–440.
Thompson LU, Jenkins DJ, Amer MA, Reicher R, Jenkins A & Kamulsky J (1982): The effect of fermented and unfermented milks on serum cholesterol. Am. J. Clin. Nutr. 36, 1106–1111.
Acknowledgements
We thank all the volunteers who took part in the study. We also thank Mr B Holden and Ms C Day of Life-Care Technologies Ltd, Worcestershire for their help and support with the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guarantors: SJ Lewis and S Burmeister.
Contributors: SJL and SB researched and wrote the review.
Rights and permissions
About this article
Cite this article
Lewis, S., Burmeister, S. A double-blind placebo-controlled study of the effects of Lactobacillus acidophilus on plasma lipids. Eur J Clin Nutr 59, 776–780 (2005). https://doi.org/10.1038/sj.ejcn.1602139
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602139
Keywords
This article is cited by
-
The effects of probiotic administration on patients with prediabetes: a meta-analysis and systematic review
Journal of Translational Medicine (2022)
-
Efficacy of Probiotic Milk Formula on Blood Lipid and Intestinal Function in Mild Hypercholesterolemic Volunteers: A Placebo-control, Randomized Clinical Trial
Probiotics and Antimicrobial Proteins (2021)
-
Effects of products designed to modulate the gut microbiota on hyperlipidaemia
European Journal of Nutrition (2019)
-
Impact of Functional Foods on Prevention of Cardiovascular Disease and Diabetes
Current Cardiology Reports (2015)
-
Effects of probiotic ultra-filtered feta cheese and raw chicory root extract on lipid profile in healthy adult volunteers: a triple-blinded randomized controlled trial
Mediterranean Journal of Nutrition and Metabolism (2013)