Abstract
Objective: To investigate the effect of riboflavin supplementation on plasma homocysteine (tHcy) concentrations in healthy elderly people with sub-optimal riboflavin status.
Design: A double-blind, randomized, placebo-controlled riboflavin supplementation trial.
Setting: Community based study in Northern Ireland.
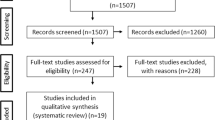
Subjects: From a screening sample of 101 healthy elderly people, 52 had sub-optimal riboflavin status (erythrocyte glutathione reductase activation coefficient, EGRAC≥1.20) and were invited to participate in the study.
Intervention: The intervention had two parts. Part 1 was a 12 week randomized double blind, placebo-controlled intervention with riboflavin (1.6 mg/day). Following completion of part 1, the placebo group went on to part 2 of the study which involved supplementation with folic acid (400 µg/day) for 6 weeks followed by folic acid and riboflavin (1.6 mg/day) for a further 12 weeks, with a 16 week washout period post-supplementation. The purpose of part 2 was: (a) to address the possibility that homocysteine-lowering in response to riboflavin may be obscured by a much greater effect of folate, and that, once folate status was optimized, a dependence of homocysteine on riboflavin might emerge; and (b) to demonstrate that these subjects had homocysteine concentrations which could be lowered by nutritional intervention.
Results: Although riboflavin supplementation significantly improved riboflavin status in both parts 1 and 2 of the study (P<0.001 for each), tHcy concentrations were unaffected (P=0.719). In contrast, folic acid supplementation (study part 2) resulted in a homocysteine lowering of 19.6% (P=0.001).
Conclusion: Despite the metabolic dependency of tHcy on riboflavin, it did not prove to be an effective homocysteine-lowering agent, even in the face of sub-optimal riboflavin status.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Andersson A, Brattstrom L, Israelsson B, Isaksson A, Hamfelt A, Hultberg B . 1992 Plasma homocysteine before and after methionine loading with regard to age, gender, and menopausal status Eur. J. Clin. Invest. 22: 79–87
Bailey AL, Maisey S, Southon S, Wright AJ, Finglas PM, Fulcher RA . 1997 Relationships between micronutrient intake and biochemical indicators of nutrient adequacy in a ‘free-living’ elderly UK population Br. J. Nutr. 77: 225–242
Bates CJ, Fuller NJ . 1986 The effect of riboflavin deficiency on methylenetetrahydrofolate reductase (NADPH) (EC 1.5.1.20) and folate metabolism in the rat Br. J. Nutr. 55: 455–464
De Bree A, Verschuren WMM, Blom HJ, Kromhout D . 2001 Association between B vitamin intake and plasma homocysteine in the general Dutch population aged 20–65 y Am. J. Clin. Nutr. 73: 1027–1031
Eikelboom JW, Lonn E, Genest J, Hankey G, Yusuf S . 1991 Homocyst(e)ine and cardiovascular disease: a critical review of the epidemiologic evidence Ann. Intern. Med. 131: 363–375
Finkelstein D . 1990 Methionine metabolism in mammals J. Nutr. Biochem. 1: 228–237
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, Boers GHJ, den Heijer M, Kluijtmans LAJ, van den Heuvel P, Rozen R . 1995 A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase Nat. Genet. 10: 111–113
Goyette P, Sumner JS, Milos R, Duncan AMV, Rosenblatt DS, Matthews RG, Rozen R . 1994 Human methylenetetrahydrofolate reductase: isolation of cDNA, mapping and mutation identification Nat. Genet. 7: 195–200
Guenther BD, Sheppard CA, Tran P, Rozen R, Matthews RG, Ludwig ML . 1999 The structure and properties of methylenetetrahydrofolate reductase from Escherichia coli suggest how folate ameliorates human hyperhomocysteinemia Nat. Struct. Biol. 6: 359–365
Guttormsen AB, Ueland PM, Nesthus I, Nygard O, Schneede J, Vollset SE, Refsum H . 1996 Determinants and vitamin responsiveness of intermediate hyperhomocysteinemia (>40 mmol/liter). The Hordaland Homocysteine Study J. Clin. Invest. 98: 2174–2183
Hustad S, Ueland PM, Vollset SE, Zhang Y, Bjorke-Monsen AL, Schneede J . 2000 Riboflavin as a determinant of plasma total homocysteine: Effect modification by the methylenetetrahydrofolate reductase C677T polymorphism Clin. Chem. 46: 1065–1071
Jacques PF, Bostom AG, Wilson PWF, Rich S, Rosenberg IH, Selhub J . 2001 Determinants of plasma total homocysteine concentration in the Framingham Offspring cohort Am. J. Clin. Nutr. 73: 613–621
Kang S-S, Wong PWK, Malinow MR . 1992 Hyperhomocyst(e)inemia as a risk factor for occlusive vascular disease A. Rev. Nutr. 12: 279–298
Kelleher BP, O'Brien SD . 1991 Microbiological assay for vitamin B12 performed in 96-well microtitre plates J. Clin. Pathol. 44: 592–595
Lakshmi AV, Ramalakshmi BA . 1998 Effect of pyridoxine or riboflavin supplementation on plasma homocysteine levels in women with oral lesions Natl Med. J. India 11: 171–172
Lakshmi R, Lakshmi AV, Bamji MS . 1990 Mechanism of impaired skin collagen maturity in riboflavin or pyridoxine deficiency J. Biosci. 15: 289–295
Madigan SM, Tracey F, McNulty H, Eaton-Evans J, Coulter J, McCartney H, Strain JJ . 1998 Dietary intake and status of riboflavin and vitamin B-6 and biochemical response to riboflavin supplementation in free-living elderly people Am. J. Clin. Nutr. 68: 389–395
McCormick DB . 1989 Two interconnected B vitamins: riboflavin and pyridoxine Physiol. Rev. 69: 1170–1198
McKinley MC, McNulty H, McPartlin J, Strain JJ, Pentieva K, Ward M, Weir DG, Scott JM . 2001 Low-dose vitamin B-6 effectively lowers fasting plasma homocysteine in healthy elderly persons who are folate and riboflavin replete Am. J. Clin. Nutr. 73: 759–764
McNulty H, McKinley MC, Wilson B, Strain JJ, McPartlin J, Weir DG, Scott JM . 2001 Riboflavin status effects the functioning of thermolabile methylenetetrahydrofolate reductase (MTHFR): implications for riboflavin requirements Ann. Nutr. Metab. 45: (Suppl 1): 60
Molloy AM, Scott JM . 1997 Microbiological assay for serum, plasma and red cell folate using cryopreserved, microtiter plate method Meth. Enzymol. 281: 43–53
Mount JN, Heduan E, Herd C, Jupp R, Kearney E, Marsh A . 1987 Adaptation of coenzyme stimulation assays for the nutritional assessment of vitamins B1, B2, and B6 using the Cobas Bio centrifugal analyser Ann. Clin. Biochem. 24: 41–46
Mudd SH, Levy HL, Skovby F . 1995 Disorders of transsulfuration In The Metabolic Basis of Inherited Disease 7th edn, ed CR Scriver, AL Beaudet, WS Sly & D Valle, pp 1279–1327 New York: McGraw-Hill
Nexo E, Engbaek F, Ueland PM, Westby C, O'Gorman P, Johnston C, Kase BF, Guttormsen AB, Alfheim I, McPartlin J, Smith D, Moller J, Rasmussen K, Clarke R, Scott JM, Refsum H . 2000 Evaluation of novel assays in clinical chemistry: quantification of plasma total homocysteine Clin. Chem. 46: 1150–1156
Olszewski AJ, Szostak WB, Bialkowska M, Rudnicki S, McCully KS . 1989 Reduction of plasma lipid and homocysteine levels by pyridoxine, folate, cobalamin, choline, riboflavin, and troxerutin in atherosclerosis Atherosclerosis 75: 1–6
Powers HJ, Bates CJ, Prentice AM, Lamb WH, Jepson M, Bowman H . 1983 The relative effectiveness of iron and iron with riboflavin in correcting a microcytic anaemia in men and children in rural Gambia Hum. Nutr. Clin. Nutr. 37C: 413–425
Quereshi KN, Hodkinson HM . 1974 Evaluation of a ten-question mental test in the institutionalised elderly Age Ageing 3: 152–157
Quinlivan EP, McPartlin J, McNulty H, Ward M, Strain JJ, Weir DG, Scott JM . 2002 Importance of both folic acid and vitamin B12 in reduction of risk of vascular disease Lancet 359: 227–228
Schneider JA, Rees DC, Liu YT, Clegg JB . 1998 Worldwide distribution of a common methylenetetrahydrofolate reductase mutation Am. J. Hum. Genet. 62: 1258–1260
Selhub J, Jacques PF, Wilson PWF, Rush D, Rosenberg IH . 1993 Vitamin status and intake as primary determinants of homocysteinemia in an elderly population JAMA 270: 2693–2698
Shimakawa T, Nieto FJ, Malinow MR, Chambless LE, Schreiner PJ, Szklo M . 1997 Vitamin intake: a possible determinant of plasma homocyst(e)ine among middle-aged adults Ann. Epidemiol. 7: 285–293
Ward M, McNulty H, McPartlin J, Strain JJ, Weir DG, Scott JM . 1997 Plasma homocysteine, a risk factor for cardiovascular disease, is lowered by physiological doses of folic acid Q. J. Med. 90: 519–524
Acknowledgements
We wish to acknowledge Clonmel Healthcare, Tipperary, Ireland for providing us with the folic acid supplements, and the volunteers who kindly participated in the study. This study was supported by EU Project BMH 4983549 and Abbott Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McKinley, M., McNulty, H., McPartlin, J. et al. Effect of riboflavin supplementation on plasma homocysteine in elderly people with low riboflavin status. Eur J Clin Nutr 56, 850–856 (2002). https://doi.org/10.1038/sj.ejcn.1601402
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1601402
Keywords
This article is cited by
-
The maternal homocysteine pathway is influenced by riboflavin intake and MTHFR polymorphisms without affecting the risk of orofacial clefts in the offspring
European Journal of Clinical Nutrition (2010)
-
Study Protocol: Randomised controlled trial to investigate the functional significance of marginal riboflavin status in young women in the UK (RIBOFEM)
BMC Public Health (2009)
-
Riboflavin supplementation and biomarkers of cardiovascular disease in the elderly
The Journal of nutrition, health and aging (2009)
-
Changes in predictors and status of homocysteine in young male adults after a dietary intervention with vegetables, fruits and bread
European Journal of Nutrition (2008)
-
A general method for selection of riboflavin-overproducing food grade micro-organisms
Microbial Cell Factories (2006)